Preliminary Analysis
- Abdominal Pain - Female
- Abdominal Pain - Male
- Acne
- Animal or Human Bite
- Antibiotics: When Do They Help?
- Arm Injury
- Arm Pain
- Asthma Attack
- Athlete's Foot
- Back Pain
- Bed Bug Bite
- Bee or Yellow Jacket Sting
- Blisters
- Boil
- Bottle-Feeding (Formula)
- Breast Feeding
- Breath-holding Spell
- Bronchiolitis-RSV
- Bruises and Cuts
- Burn
- Chest Pain
- Chickenpox
- Circumcision Problems
- Colds
- Constipation
- Cough
- Coughs: Meds or Home Remedies?
- Cracked or Dry Skin
- Cradle Cap
- Croup
- Crying Baby - Before 3 Months Old
- Crying Child - 3 Months and Older
- Cut, Scrape, or Bruise
- Diaper Rash
- Diarrhea
- Diarrhea Diseases From Travel
- Dizziness
- Drinking Fluids - Decreased
- Dry Skin
- Ear - Congestion
- Ear - Discharge
- Ear - Pulling At or Rubbing
- Ear - Swimmer's
- Ear Infection
- Ear Injury
- Earache
- Earwax Buildup
- Ebola Exposure
- Eczema
- Emergency Symptoms
- Eye - Allergy
- Eye - Foreign Object
- Eye - Pus or Discharge
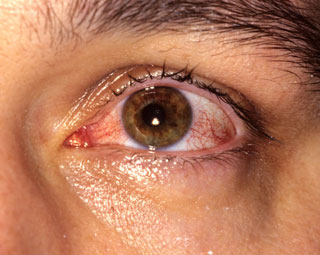
- Eye - Red Without Pus
- Eye Injury
- Eye Swelling
- Fainting
- Fever
- Fever - How to Take the Temperature
- Fever - Myths Versus Facts
- Fifth Disease
- Finger Injury
- Fire Ant Sting
- Flu
- Fluid Intake Decreased
- Food Allergy
- Foreskin Care Questions
- Frostbite
- Genital Injury - Female
- Genital Injury - Male
- Hair Loss
- Hand-Foot-And-Mouth Disease (HFMD)
- Hay Fever
- Head Injury
- Head Lice
- Headache
- Heat Exposure and Reactions
- Heat Rash
- Hives
- Human or Animal Bite
- Immunization Reactions
- Impetigo - Infected Sores
- Infection Exposure Questions
- Influenza - Seasonal
- Influenza Exposure
- Insect Bite
- Jaundiced Newborn
- Jellyfish Sting
- Jock Itch
- Leg Injury
- Leg Pain
- Lymph Nodes - Swollen
- Medicine - Refusal to Take
- Menstrual Cramps
- Menstrual Period - Missed or Late
- Mental Health Problems
- Molluscum
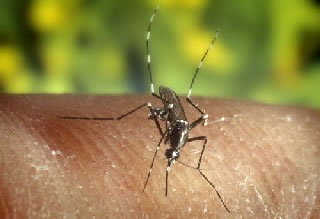
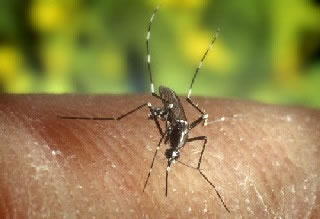
- Mosquito Bite
- Mosquito-Borne Diseases from Travel
- Motion Sickness
- Mouth Injury
- Mouth Ulcers
- Neck Pain or Stiffness
- Newborn Appearance Questions
- Newborn Illness - How to Recognize
- Newborn Rashes and Birthmarks
- Newborn Reflexes and Behavior
- Nose Allergy (Hay Fever)
- Nose Injury
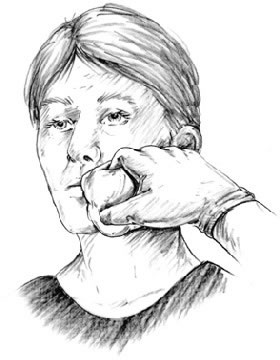
- Nosebleed
- Penis-Scrotum Symptoms
- Pinworms
- Poison Ivy - Oak - Sumac
- Puncture Wound
- Rash or Redness - Localized
- Rash or Redness - Widespread
- Reflux (Spitting Up)
- Ringworm
- Roseola
- RSV-Bronchiolitis
- Scabies
- Scorpion Sting
- Scrape
- Sinus Pain or Congestion
- Skin Foreign Object
- Skin Injury
- Skin Lump
- Sliver or Splinter
- Sore Throat
- Spider Bite
- Stomach Pain - Female
- Stomach Pain - Male
- Stools - Blood In
- Stools - Unusual Color
- Strep Throat Exposure
- Strep Throat Infection
- Sty
- Sunburn
- Suture Questions
- Swallowed Foreign Object
- Swallowed Harmless Substance
- Swimmer's Itch - Lakes and Oceans
- Tear Duct - Blocked
- Teething
- Thrush
- Tick Bite
- Toe Injury
- Toenail - Ingrown
- Tooth Injury
- Toothache
- Umbilical Cord Symptoms
- Urinary Tract Infection - Female
- Urination Pain - Female
- Urination Pain - Male
- Vaginal Bleeding
- Vaginal Symptoms
- Vomiting With Diarrhea
- Vomiting Without Diarrhea
- Warts
- Weakness and Fatigue
- Wheezing (Other Than Asthma)
- Wound Infection
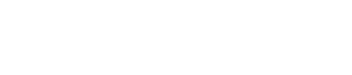
Stomach Pain - Female
Is this your child's symptom?
- Pain or discomfort in the stomach or belly area
- Female
- Pain found between the bottom of the rib cage and the groin crease
- The older child complains of stomach pain
- The younger child points to or holds the stomach
- Before 12 months of age, use the Crying care guides
If NOT, try one of these:
Causes of Acute Stomach Pain
- Eating Too Much. Eating too much can cause an upset stomach and mild stomach pain.
- Hunger Pains. Younger children may complain of stomach pain when they are hungry.
- GI Virus (such as Rotavirus). A GI virus can cause stomach cramps as well as vomiting and/or diarrhea.
- Food Poisoning. This causes sudden vomiting and/or diarrhea within hours after eating the bad food. It is caused by toxins from germs growing in foods left out too long. Most often, symptoms go away in less than 24 hours. It often can be treated at home without the need for medical care.
- Constipation. The need to pass a stool may cause cramps in the lower abdomen.
- Strep Throat. A strep throat infection causes 10% of new onset stomach pain with fever.
- Bladder Infection. Bladder infections usually present with painful urination, urgency and bad smelling urine. Sometimes the only symptom is pain in the lower abdomen.
- Appendicitis (Serious). Suspect appendicitis if pain is low on the right side and walks bent over. Other signs are the child won't hop and wants to lie still.
- Intussusception (Serious). Sudden attacks of severe pain that switch back and forth with periods of calm. Caused by one segment of bowel telescoping into a lower piece of bowel. Peak age is 6 months to 2 years.
Causes of Recurrent Stomach Pains
- Stress or Worries. The most common cause of frequent stomach pains is stress. Over 10% of children have a "worried stomach." These children tend to be sensitive and too serious. They often are model children. This can make them more at risk to the normal stresses of life. Examples of these events are changing schools, moving or family fights. The pain is in the pit of the stomach or near the belly button. The pain is real.
- Abdominal Migraine. Attacks of stomach pain and vomiting with sudden onset and offset. Often occur in children who later develop migraine headaches. Strongly genetic.
- Functional Abdominal Pains. Functional means the stomach pains are due to a sensitive GI tract. The GI tract is free of any disease.
- School Avoidance. Stomach pains that mainly occur in the morning on school days. They keep the child from going to school.
Pain Scale
- Mild: Your child feels pain and tells you about it. But, the pain does not keep your child from any normal activities. School, play and sleep are not changed.
- Moderate: The pain keeps your child from doing some normal activities. It may wake him or her up from sleep.
- Severe: The pain is very bad. It keeps your child from doing all normal activities.
When to Call for Stomach Pain - Female
Call 911 Now
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Self Care at Home
|
Call 911 Now
- Not moving or too weak to stand
- You think your child has a life-threatening emergency
Call Doctor or Seek Care Now
- Pain low on the right side
- Could be pregnant
- Constant pain (or crying) for more than 2 hours
- Recent injury to the stomach
- High-risk child (such as diabetes, sickle cell disease, recent abdominal surgery)
- Age less than 2 years old
- Fever over 104° F (40° C)
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Call Doctor Within 24 Hours
- Moderate pain that keeps from some normal activities
- Mild pain that comes and goes (cramps), but lasts more than 24 hours
- Fever is present
- Bladder infection (UTI) suspected (passing urine hurts, new onset wetting)
- You think your child needs to be seen, but the problem is not urgent
Call Doctor During Office Hours
- Stomach pains are a frequent problem
- You have other questions or concerns
Self Care at Home
- Mild stomach pain
Care Advice for Stomach Pain
-
What You Should Know About Stomach Pain:
- Mild stomach pain can be caused by something simple. It could be from gas pains or eating too much.
- Sometimes, stomach pain signals the start of a viral infection. This will lead to vomiting or loose stools.
- Watching your child for 2 hours will help tell you the cause.
- Here is some care advice that should help.
-
Lie Down:
- Have your child lie down and rest until feeling better.
-
Clear Fluids:
- Offer clear fluids only (such as water, flat soft drinks or half-strength Gatorade).
- For mild pain, offer a regular diet.
-
Prepare for Vomiting:
- Keep a vomiting pan handy.
- Younger children often talk about stomach pain when they have nausea. Nausea is the sick stomach feeling that comes before they throw up.
-
Pass a Stool:
- Have your child sit on the toilet and try to pass a stool.
- This may help if the pain is from constipation or diarrhea.
- Note: For constipation, moving a warm wet cotton ball on the anus may help.
-
Do Not Give Medicines:
- Any drug (like ibuprofen) could upset the stomach and make the pain worse.
- Do not give any pain medicines or laxatives for stomach cramps.
- For fever over 102° F (39° C), acetaminophen (such as Tylenol) can be given.
-
What to Expect:
- With harmless causes, the pain is most often better or gone in 2 hours.
- With stomach flu, belly cramps may happen before each bout of vomiting or diarrhea. These cramps may come and go for a few days.
- With serious causes (such as appendicitis), the pain worsens and becomes constant.
-
Call Your Doctor If:
- Pain becomes severe
- Constant pain lasts more than 2 hours
- Mild pain that comes and goes lasts more than 24 hours
- You think your child needs to be seen
- Your child becomes worse
-
Extra Help: Worried Stomach:
- Help your child talk about events that trigger the stomach pain. Talk to your child about how to cope with these the next time around.
- Help your child worry less about things she can't control.
- To treat the pain, help your child get very relaxed. Lying down in a quiet place and taking slow deep breaths may help. Make the belly go up and down with each breath. Then try to relax all the muscles in the body. Think about something pleasant. Listening to audios that teach how to relax might also help.
- Make sure your child gets enough sleep.
- Make sure that your child doesn't miss any school because of stomach pains. Stressed children tend to want to stay home when the going gets rough.
- Caution: Your child should see her doctor for an exam. Do this before concluding frequent stomach pains are from worrying too much.
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.
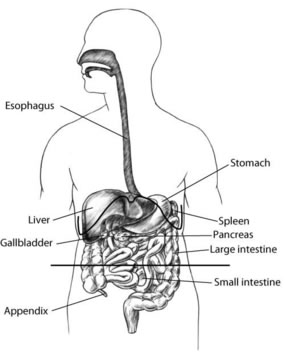
Stomach Pain - Male
Is this your child's symptom?
- Pain or discomfort in the stomach or belly area
- Male
- Pain found between the bottom of the rib cage and the groin crease
- The older child complains of stomach pain
- The younger child points to or holds the stomach
- Before 12 months of age, use the Crying care guides
If NOT, try one of these:
Causes of Acute Stomach Pain
- Eating Too Much. Eating too much can cause an upset stomach and mild stomach pain.
- Hunger Pains. Younger children may complain of stomach pain when they are hungry.
- GI Virus (such as Rotavirus). A GI virus can cause stomach cramps as well as vomiting and/or diarrhea.
- Food Poisoning. This causes sudden vomiting and/or diarrhea within hours after eating the bad food. It is caused by toxins from germs growing in foods left out too long. Most often, symptoms go away in less than 24 hours. It often can be treated at home without the need for medical care.
- Constipation. The need to pass a stool may cause cramps in the lower abdomen.
- Strep Throat. A strep throat infection causes 10% of new onset stomach pain with fever.
- Bladder Infection. Bladder infections usually present with painful urination, urgency and bad smelling urine. Sometimes the only symptom is pain in the lower abdomen.
- Appendicitis (Serious). Suspect appendicitis if pain is low on the right side and walks bent over. Other signs are the child won't hop and wants to lie still.
- Intussusception (Serious). Sudden attacks of severe pain that switch back and forth with periods of calm. Caused by one segment of bowel telescoping into a lower piece of bowel. Peak age is 6 months to 2 years.
Causes of Recurrent Stomach Pains
- Stress or Worries. The most common cause of frequent stomach pains is stress. Over 10% of children have a "worried stomach." These children tend to be sensitive and too serious. They often are model children. This can make them more at risk to the normal stresses of life. Examples of these events are changing schools, moving or family fights. The pain is in the pit of the stomach or near the belly button. The pain is real.
- Abdominal Migraine. Attacks of stomach pain and vomiting with sudden onset and offset. Often occur in children who later develop migraine headaches. Strongly genetic.
- Functional Abdominal Pains. Functional means the stomach pains are due to a sensitive GI tract. The GI tract is free of any disease.
- School Avoidance. Stomach pains that mainly occur in the morning on school days. They keep the child from going to school.
Pain Scale
- Mild: Your child feels pain and tells you about it. But, the pain does not keep your child from any normal activities. School, play and sleep are not changed.
- Moderate: The pain keeps your child from doing some normal activities. It may wake him or her up from sleep.
- Severe: The pain is very bad. It keeps your child from doing all normal activities.
When to Call for Stomach Pain - Male
Call 911 Now
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Self Care at Home
|
Call 911 Now
- Not moving or too weak to stand
- You think your child has a life-threatening emergency
Call Doctor or Seek Care Now
- Pain low on the right side
- Pain or swelling in the scrotum
- Constant pain (or crying) for more than 2 hours
- Recent injury to the stomach
- High-risk child (such as diabetes, sickle cell disease, recent abdominal surgery)
- Age less than 2 years old
- Fever over 104° F (40° C)
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Call Doctor Within 24 Hours
- Moderate pain that keeps from some normal activities
- Mild pain that comes and goes (cramps), but lasts more than 24 hours
- Fever is present
- Bladder infection (UTI) suspected (passing urine hurts, new onset wetting)
- You think your child needs to be seen, but the problem is not urgent
Call Doctor During Office Hours
- Stomach pains are a frequent problem
- You have other questions or concerns
Self Care at Home
- Mild stomach pain
Care Advice for Stomach Pain
-
What You Should Know About Stomach Pain:
- Mild stomach pain can be caused by something simple. It could be from gas pains or eating too much.
- Sometimes, stomach pain signals the start of a viral infection. This will lead to vomiting or loose stools.
- Watching your child for 2 hours will help tell you the cause.
- Here is some care advice that should help.
-
Lie Down:
- Have your child lie down and rest until feeling better.
-
Clear Fluids:
- Offer clear fluids only (such as water, flat soft drinks or half-strength Gatorade).
- For mild pain, offer a regular diet.
-
Prepare for Vomiting:
- Keep a vomiting pan handy.
- Younger children often talk about stomach pain when they have nausea. Nausea is the sick stomach feeling that comes before they throw up.
-
Pass a Stool:
- Have your child sit on the toilet and try to pass a stool.
- This may help if the pain is from constipation or diarrhea.
- Note: For constipation, moving a warm wet cotton ball on the anus may help.
-
Do Not Give Medicines:
- Any drug (like ibuprofen) could upset the stomach and make the pain worse.
- Do not give any pain medicines or laxatives for stomach cramps.
- For fever over 102° F (39° C), acetaminophen (such as Tylenol) can be given.
-
What to Expect:
- With harmless causes, the pain is most often better or gone in 2 hours.
- With stomach flu, belly cramps may happen before each bout of vomiting or diarrhea. These cramps may come and go for a few days.
- With serious causes (such as appendicitis), the pain worsens and becomes constant.
-
Call Your Doctor If:
- Pain becomes severe
- Constant pain lasts more than 2 hours
- Mild pain that comes and goes lasts more than 24 hours
- You think your child needs to be seen
- Your child becomes worse
-
Extra Help: Worried Stomach:
- Help your child talk about events that trigger the stomach pain. Talk to your child about how to cope with these the next time around.
- Help your child worry less about things he can't control.
- To treat the pain, help your child get very relaxed. Lying down in a quiet place and taking slow deep breaths may help. Make the belly go up and down with each breath. Then try to relax all the muscles in the body. Think about something pleasant. Listening to audios that teach how to relax might also help.
- Make sure your child gets enough sleep.
- Make sure that your child doesn't miss any school because of stomach pains. Stressed children tend to want to stay home when the going gets rough.
- Caution: Your child should see his doctor for an exam. Do this before concluding frequent stomach pains are from worrying too much.
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.
Acne
Is this your child's symptom?
- Pimples and blackheads on the face caused by blocked oil glands
If NOT, try one of these:
Symptoms of Acne
- Whiteheads (pimples) are plugged oil glands that are closed.
- Blackheads are plugged oil glands that are open. Reason: The oil turns black when it is exposed to air.
- Whiteheads and blackheads are also called "zits."
- Red bumps are from blocked oil glands that have leaked oil. This causes irritation in the skin around them. Larger red bumps can be quite painful.
- Acne mainly appears on your face, neck, and shoulders
Causes of Acne
- Acne skin changes are from plugged oil glands. Acne has several causes.
- Increased levels of hormones during puberty have a part. Heredity also plays an important role.
- Some skin bacteria can make it worse.
- Acne is not caused by diet. You do not need to avoid eating fried foods, chocolate, or any other food.
- Acne is not caused by dirt or by not washing your face often enough.
When to Call for Acne
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Self Care at Home
|
Call Doctor or Seek Care Now
- Spreading red area around the acne with fever
- Spreading red area or streak that's very large
- Your child looks or acts very sick
Call Doctor Within 24 Hours
- Spreading red area or streak around the acne, but no fever
- You think your child needs to be seen
Call Doctor During Office Hours
- Tender red lumps that are large occur
- Yellow soft scab that drains pus or gets bigger occurs
- After treating with Benzoyl Peroxide (BP) for 2 months, acne not improved
- BP makes the face itchy or swollen
- You have other questions or concerns
Self Care at Home
- Mild acne
Care Advice for Acne
-
What You Should Know About Acne:
- More than 90% of teenagers have some acne. Acne is a normal part of the teen years.
- There is no medicine at this time that will cure acne.
- However, good skin care can keep acne under control and at a mild level.
- Here is some care advice that should help.
-
Benzoyl Peroxide Gel:
- Benzoyl Peroxide (BP) is the best OTC medicine for bringing acne under control. Use a Benzoyl Peroxide 5% gel product (such as the store brand). OTC means no prescription is needed.
- It helps to open pimples and to unplug blackheads. It also kills bacteria.
- Apply the lotion once a day at bedtime to the area with acne. Redheads and blonds should apply it every other day for the first 2 weeks. Reason: More sensitive skin.
- Use an amount of lotion the size of a pea. This should be enough to cover most of the acne.
- If the skin becomes red or peels, use less of it. Other option: You can use it less often.
- Caution: Avoid the corners of the eyes, nose and mouth. Reason: These areas are very sensitive.
- Caution: Benzoyl Peroxide bleaches clothing, towels, blankets, etc. Apply it only at bedtime and put it on sparingly. Use a plain white pillowcase.
-
Antibiotics for Red Bumps:
- Large red bumps mean the infection has spread beyond the oil gland. If you have several red bumps, your doctor may prescribe an antibiotic.
- Antibiotics come as solutions for the skin or as pills.
- The antibiotic will kill the bacteria that are causing the infection.
- Give the antibiotic as directed.
-
Washing the Face:
- Wash your skin twice a day. The most important time to wash is bedtime. Just use warm water or you can use a mild soap (such as Dove).
- Shampoo your hair daily.
- Avoid scrubbing your skin. Reason: Hard scrubbing of the skin irritates the openings of the oil glands. This causes them to close off even more tightly.
-
Pimple Opening:
- Opening (popping) pimples is not advised by many doctors. But, most teens and adults do it anyway.
- So, here's how to open a pimple safely without any squeezing.
- Never open a pimple before it has come to a head.
- Wash your face and hands first.
- Use a sterile needle (cleaned with rubbing alcohol). Nick the surface of the yellow pimple with the tip of the needle. The pus should run out without squeezing.
- Wipe away the pus and wash the area with soap and water.
- Opening small pimples in this way will not cause skin damage.
-
Avoid Picking or Squeezing Acne:
- Many young people pick at their acne when they are not thinking about it. Picking makes acne worse.
- Try not to touch the face at all during the day.
- Squeezing blackheads causes bleeding into the skin. The bleeding turns into brownish blotches on the skin. They can take 1 or 2 months to fade.
- Squeezing red lumps can force bacteria into the skin. This too leaves blotches. It can also cause a serious face infection.
-
Prevention - Avoid Triggers of Acne:
- Avoid putting any oily or greasy substances on your face. Reason: They block oil glands and make acne worse. If you use cosmetics, use water-based cosmetics.
- Avoid hair tonics or hair creams (especially greasy ones). When you sweat, they will get on the face and irritate the acne.
-
What to Expect:
- With treatment, new whiteheads and blackheads will decrease. But, it takes 6 to 8 weeks.
- Acne usually lasts until age 20 or 25.
- So, you will need to continue the treatment for several years.
- You don't need to worry about scarring. It is very rare for acne to leave any scars.
-
Call Your Doctor If:
- With treatment, the acne has not improved after 2 months
- It looks infected (large, red, tender bumps)
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.
Animal or Human Bite
Is this your child's symptom?
- Bite from a pet, wild animal or human
Types of Wounds
- Bruise. There is no break in the skin. No risk of infection.
- Scrape (Abrasion) or Scratch. A wound that doesn't go all the way through the skin. Low chance of infection. Antibiotic drugs are not needed.
- Cut (Laceration). A wound that goes through the skin to the fat or muscle tissue. Some chance of infection. Most need to be seen. Cleaning the wound can help prevent this. Antibiotic drugs may be needed.
- Puncture Wound. These wounds break through the skin. Greater risk of infection. Puncture wounds from cat bites are more likely to get infected. Antibiotic drugs may be needed.
- Wound Infection. This is the main risk of an animal bite. The main finding is redness around the bite and pain. It starts 8 hours to 3 days after the bite. It can often be prevented by early, careful cleaning of the bite. This is why most animal bites need to be seen.
Types of Animal Bites
- Large Wild Animal Bites. Rabies is a disease that can kill people. Bites or scratches from any large wild animal can pass on rabies. Animals at highest risk are bats, skunks, raccoons, foxes, or coyotes. These animals may spread rabies even if they have no symptoms.
- Small Wild Animal Bites. Small animals such as mice, rats, moles, or gophers do not carry rabies. Chipmunks, prairie dogs, squirrels and rabbits also do not carry rabies. Exception: one of these small animals actually attacks a human (an unprovoked bite). Sometimes, their bites can get infected.
- Large Pet Animal Bites. Most bites from pets are from dogs or cats. Bites from other pets such as horses can be handled using this guide. Dogs and cats are free of rabies in most U.S. and Canadian cities. Stray animals are always at risk for rabies until proven otherwise. Cats and dogs that always stay indoors should be safe. The main risk in pet bites is wound infection, not rabies. Cat bites become infected more often than dog bites. Cat scratches can get infected just like a bite because cats lick their claws.
- Small Indoor Pet Animal Bites. Small indoor pets are not at risk for rabies. Examples of these pets are gerbils, hamsters, guinea pigs, or mice. Tiny puncture wounds from these small animals also don't need to be seen. They carry a small risk for wound infections.
- Human Bites. Most human bites occur during fights, especially in teenagers. Sometimes a fist is cut when it strikes a tooth. Human bites are more likely to become infected than animal bites. Bites on the hands are at higher risk. Many toddler bites are safe because they don't break the skin.
- Bat Bites and Rabies. In the U.S., 90% of cases of rabies in humans are caused by bats. Bats have spread rabies without a visible bite mark.
Animals at Risk for Rabies
- Bat, skunk, raccoon, fox, or coyote
- Other large wild animals
- Pets that have never had rabies shots and spend time outdoors
- In the U.S., rabies occurs 4 times more in cats than in dogs.
- Outdoor animals who are sick or stray
- Dogs or cats in countries that do not require rabies shots
- In the U.S. and Canada, bites from city dogs and cats are safe.
- In the U.S., there are 2 - 3 deaths from rabies per year in humans.
When to Call for Animal or Human Bite
Call 911 Now
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Self Care at Home
|
Call 911 Now
- Major bleeding that can't be stopped
- Not moving or too weak to stand
- You think your child has a life-threatening emergency
Call Doctor or Seek Care Now
- Wild animal bite that breaks the skin
- Pet animal (such as dog or cat) bite that breaks the skin. Exception: minor scratches that don't go through the skin.
- Puncture wound (holes through skin) from a Cat's teeth or claws
- Puncture wound (holes through skin) of hand or face
- Human bite that breaks the skin
- Bite looks infected (redness or red streaks) or has a fever
- Bat contact or exposure, even without a bite mark
- Contact with a rabies-prone animal, even without a bite mark
- Minor cut or scrape and no past tetanus shots
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Call Doctor Within 24 Hours
- Last tetanus shot more than 5 years ago
- You think your child needs to be seen, but the problem is not urgent
Call Doctor During Office Hours
- You have other questions or concerns
Self Care at Home
- Bite did not break the skin or is only a bruise
- Minor scratches that don't go through the skin from a pet
- Tiny puncture wound from small pet, such as a hamster or puppy. Exception: cat puncture wound.
Care Advice for Animal or Human Bite
-
What You Should Know About Bites:
- Bites that don't break the skin can't become infected.
- Cuts and punctures always are at risk for infection.
- Here is some care advice that should help.
-
Clean the Bite:
- Wash all wounds right now with soap and water for 5 minutes.
- Also, flush well under running water for a few minutes. Reason: Can prevent many wound infections.
-
Bleeding - How to Stop:
- For any bleeding, put pressure on the wound.
- Use a gauze pad or clean cloth.
- Press for 10 minutes or until the bleeding has stopped.
-
Antibiotic Ointment:
- For small cuts, use an antibiotic ointment (such as Polysporin). No prescription is needed.
- Put it on the cut 3 times a day.
- Do this for 3 days.
-
Pain Medicine:
- To help with the pain, give an acetaminophen product (such as Tylenol).
- Another choice is an ibuprofen product (such as Advil).
- Use as needed.
-
Cold Pack for Pain:
- For pain or bruising, use a cold pack. You can also use ice wrapped in a wet cloth. Apply it to the bruise once for 20 minutes. Reason: Helps with bleeding, pain and swelling.
-
What to Expect:
- Most scratches, scrapes and other minor bites heal up fine in 5 to 7 days.
-
Call Your Doctor If:
- Bite starts to look infected (pus, redness, red streaks)
- Fever occurs
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.
Antibiotics: When Do They Help?
Antibiotics are strong medicines that can kill bacteria. They have saved many lives and prevented bad outcomes. These drugs do not kill viruses. They only work on bacteria. Every day, doctors must decide if a child's infection is viral or bacterial. Here's how they do it:
Bacterial Infections
Much less common than viral infections. Antibiotics can help. Bacteria cause:
- Most ear infections
- Most sinus infections (not sinus congestion)
- 20% of sore throats which are Strep throats
- 10% of pneumonia (a lung infection)
Viral Infections
Most infections in children are caused by a virus. Antibiotics do not help. Viruses cause:
- 100% of colds. (Note: unless they turn into an ear or sinus infection. This happens with 5 to 10% of colds.)
- 95% of new coughs. (Note: asthma can also start with a cough.)
- 95% of fevers
- 80% of sore throats
- 90% of pneumonia. (Note: most cases in children are caused by a virus.)
- 99% of diarrhea and vomiting
- Note: There are a few anti-viral drugs that can treat viral infections. An example is Tamiflu used for severe influenza.
Cold Symptoms that are Normal
Parents sometimes are worried about common cold symptoms. The symptoms below are not signs of bacterial infections. Nor, are they a reason to start antibiotics.
- Green or yellow nose discharge. This is a normal part of getting over a cold. It is not a clue to a sinus infection.
- Green or yellow coughed up phlegm. This is a normal part of getting over viral bronchitis. It is not a sign of pneumonia.
- High fevers. High fevers (more than 104° F or 40° C) can be caused by a virus or bacteria.
Side Effects of Antibiotics
All antibiotics have side effects. Some children taking these drugs can get side effects. Examples are diarrhea, nausea, vomiting, or a rash. Loose stools occur because the drug kills off the good bacteria in the gut. If your child gets a rash, it can be from the drug. Your doctor has to decide if the rash is an allergy or not. The biggest side effect of overuse is called antibiotic resistance. This is when the germs are no longer killed by the drug. That's why we only use antibiotics if your child really needs one.
Giving Antibiotics for Viral Infections: What Happens?
If your child has a virus, an antibiotic won't get rid of the fever. It will not help the other symptoms. The drug will not get your child back to school sooner. It will not get you back to work any faster. If your child has side effects from the drug, he will feel worse.
What You Can Do
- Save antibiotics for bacterial infections when your child really needs them
- Don't pressure your child's doctor for an antibiotic
- Treat your child's cold and cough symptoms with home treatment that works
- Keep in mind that fever is fighting the infection. It also boosts the immune system to prevent future infections.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.
Arm Injury
Is this your child's symptom?
- Injuries to the arm (shoulder to fingers)
- Injuries to a bone, muscle, joint or ligament
- Excluded: Muscle pain caused by too much exercise or work (overuse). Covered in Arm Pain.
If NOT, try one of these:
Types of Arm Injuries
- Fractures. Fractures are broken bones. A broken collarbone is the most common broken bone in children. It's easy to notice because the collar bone is tender to touch. Also, the child cannot raise the arm upward.
- Dislocations. This happens when a bone is pulled out of a joint. A dislocated elbow is the most common type of this injury in kids. It's caused by an adult quickly pulling or lifting a child by the arm. Mainly seen in 1 to 4 year olds. It's also easy to spot. The child will hold his arm as if it were in a sling. He will keep the elbow bent and the palm of the hand down.
- Sprains. Sprains are stretches and tears of ligaments.
- Strains. Strains are stretches and tears of muscles (such as a pulled muscle).
- Muscle Overuse. Muscle pain can occur without an injury. There is no fall or direct blow. Muscle overuse is from hard work or sports (such as a sore shoulder).
- Muscle bruise from a direct blow
- Bone bruise from a direct blow
- Skin Injury. Examples are a cut, scratch, scrape or bruise. All are common with arm injuries.
Pain Scale
- Mild: your child feels pain and tells you about it. But, the pain does not keep your child from any normal activities. School, play and sleep are not changed.
- Moderate: the pain keeps your child from doing some normal activities. It may wake him or her up from sleep.
- Severe: the pain is very bad. It keeps your child from doing all normal activities.
When to Call for Arm Injury
Call 911 Now
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Self Care at Home
|
Call 911 Now
- Serious injury with many broken bones
- Major bleeding that can't be stopped
- Bone is sticking through the skin
- You think your child has a life-threatening emergency
Call Doctor or Seek Care Now
- Can't move the shoulder, elbow or wrist normally
- Can't open and close the hand normally
- Skin is split open or gaping and may need stitches
- Cut over knuckle of hand
- Age less than 1 year old
- Severe pain and not better 2 hours after taking pain medicine
- You think your child has a serious injury
- You think your child needs to be seen, and the problem is urgent
Call Doctor Within 24 Hours
- Very large bruise or swelling
- Pain not better after 3 days
- You think your child needs to be seen, but the problem is not urgent
Call Doctor During Office Hours
- Injury limits sports or school work
- Dirty cut and no tetanus shot in more than 5 years
- Clean cut and no tetanus shot in more than 10 years
- Pain lasts more than 2 weeks
- You have other questions or concerns
Self Care at Home
- Bruised muscle or bone from direct blow
- Pain in muscle from minor pulled muscle
- Pain around joint from minor stretched ligament
- Minor cut or scrape
Care Advice for Minor Arm Injuries
-
What You Should Know About Minor Arm Injuries:
- During sports, muscles and bones get bruised.
- Muscles get stretched.
- Here is some care advice that should help.
-
Pain Medicine:
- To help with the pain, give an acetaminophen product (such as Tylenol).
- Another choice is an ibuprofen product (such as Advil). Ibuprofen works well for this type of pain.
- Use as needed.
-
Small Cut or Scrape Treatment:
- Use direct pressure to stop any bleeding. Do this for 10 minutes or until bleeding stops.
- Wash the wound with soap and water for 5 minutes. Try to rinse the cut under running water.
- Gently scrub out any dirt with a washcloth.
- Use an antibiotic ointment (such as Polysporin). No prescription is needed. Then, cover it with a bandage. Change daily.
-
Cold Pack for Pain:
- For pain or swelling, use a cold pack. You can also use ice wrapped in a wet cloth.
- Put it on the sore muscles for 20 minutes.
- Repeat 4 times on the first day, then as needed.
- Reason: Helps the pain and helps stop any bleeding.
- Caution: Avoid frostbite.
-
Use Heat After 48 Hours:
- If pain lasts over 2 days, put heat on the sore muscle.
- Use a heat pack, heating pad or warm wet washcloth.
- Do this for 10 minutes, then as needed.
- Reason: Increase blood flow and improve healing.
- Caution: Avoid burns.
-
Rest the Arm:
- Rest the injured arm as much as possible for 48 hours.
-
What to Expect:
- Pain and swelling most often peak on day 2 or 3.
- Swelling should be gone by 7 days.
- Pain may take 2 weeks to fully go away.
-
Call Your Doctor If:
- Pain becomes severe
- Pain is not better after 3 days
- Pain lasts more than 2 weeks
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.
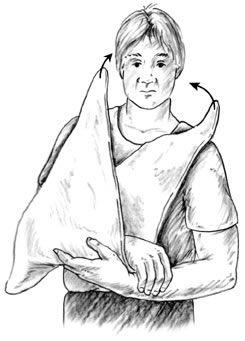
To put on a sling you first need to have a triangular bandage. Many first aid kits have a triangular bandage.
- Find the two ends of the triangle that are farthest apart. These are the ends that you will tie around the neck.
- Lay the arm down the middle of the triangle.
- Take the two ends of the triangle that are farthest apart and tie them behind the neck. (a square knot is best, but any knot will do).

- Apply direct pressure to the entire wound with a sterile gauze dressing or a clean cloth.

- Immobilize the hand and wrist by placing them on a rigid splint (see drawing).
- Tie several cloth strips around hand/wrist to keep the splint in place. You can use a roll of gauze or tape instead of cloth strips.
Notes:
- You can make a splint from: a wooden board, magazine folded in half, folded-up newspaper, cardboard, or a pillow.
- If you have no splinting materials, then support the injured arm by resting it on a pillow or folded up blanket.
- After putting on the splint, apply a cold pack or an ice pack (wrapped in a towel) to the area.
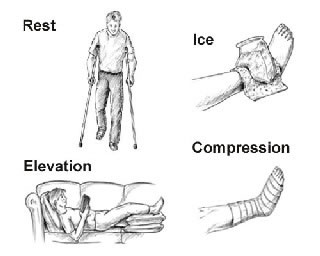
RICE is an acronym for how to take care of a sprain, strain, or bruise. There are four things you should do:
- REST the injured part of your body for 24 hours. Can return to normal activity after 24 hours of rest if the activity does not cause severe pain.
- Apply a cold pack or an ICE bag (wrapped in a moist towel) to the area for 20 minutes. Repeat in 1 hour, then every 4 hours while awake.
- Apply COMPRESSION by wrapping the injured part with a snug, elastic bandage for 48 hours. If numbness, tingling, or increased pain occurs in the injured part, the bandage may be too tight. Loosen the bandage wrap.
- Keep the injured part of the body ELEVATED and at rest for 24 hours. For example, for an injured ankle, place that leg up on a pillow and stay off the feet as much as possible.
Arm Pain
Is this your child's symptom?
- Pain in the arm (shoulder to fingers)
- Includes shoulder, elbow, wrist and finger joints
- Includes minor muscle strains from hard work or sports (overuse)
- Pain is not caused by an injury
If NOT, try one of these:
Causes of Arm Pain
- Muscle Overuse (Strained Muscles). Arm pains are often from hard muscle work or sports. Examples are too much throwing or swimming. They are most common in the shoulder. This type of pain can last from hours up to 7 days.
- Muscle Cramps. Brief pains that last 1 to 15 minutes are often due to muscle cramps. These occur in the hand after too much writing or typing.
- Viral Illness. Mild muscle aches in both arms also occur with many viral illnesses.
- Septic Arthritis (Serious). This is a bacterial infection of a joint space. Main symptoms are fever and severe pain with movement of the joint. Range of motion is limited or absent (a "frozen joint").
Pain Scale
- Mild: your child feels pain and tells you about it. But, the pain does not keep your child from any normal activities. School, play and sleep are not changed.
- Moderate: the pain keeps your child from doing some normal activities. It may wake him or her up from sleep.
- Severe: the pain is very bad. It keeps your child from doing all normal activities.
When to Call for Arm Pain
Call 911 Now
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Self Care at Home
|
Call 911 Now
- Not moving or too weak to stand
- You think your child has a life-threatening emergency
Call Doctor or Seek Care Now
- Can't use arm or hand normally
- Can't move the shoulder, elbow or wrist normally
- Swollen joint
- Muscles are weak (loss of strength)
- Numbness (loss of feeling) lasts more than 1 hour
- Severe pain or cries when arm is touched or moved
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Call Doctor Within 24 Hours
- Fever is present
- Bright red area on skin
- You think your child needs to be seen, but the problem is not urgent
Call Doctor During Office Hours
- Cause of arm pain is not clear
- Arm pain lasts more than 7 days
- Arm pains or muscle cramps are a frequent problem
- You have other questions or concerns
Self Care at Home
- Caused by overusing the muscles
- Cause is clear and harmless. (Examples are a sliver that's removed or a recent shot)
Care Advice for Strained Arm Muscles
-
What You Should Know About Mild Arm Pain:
- Strained muscles are common after using them too much during sports.
- An example is throwing a ball over and over again.
- Weekend warriors who are out of shape get the most muscle pains.
- Here is some care advice that should help.
-
Pain Medicine:
- To help with the pain, give an acetaminophen product (such as Tylenol).
- Another choice is an ibuprofen product (such as Advil).
- Use as needed.
-
Cold Pack for Pain:
- For pain or swelling, use a cold pack. You can also use ice wrapped in a wet cloth.
- Put it on the sore muscles for 20 minutes.
- Repeat 4 times on the first day, then as needed.
- Caution: Avoid frostbite.
-
Use Heat After 48 Hours:
- If pain lasts over 2 days, put heat on the sore muscle.
- Use a heat pack, heating pad or warm wet washcloth.
- Do this for 10 minutes, then as needed.
- Reason: Increase blood flow and improve healing.
- Caution: Avoid burns.
-
What to Expect:
- A strained muscle hurts for 2 or 3 days.
- The pain often peaks on day 2.
- After severe overuse, the pain may last a week.
-
Call Your Doctor If:
- Fever or swollen joint occurs
- Pain caused by work or sports lasts over 7 days
- You think your child needs to be seen
- Pain gets worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.
Asthma Attack
Is this your child's symptom?
- Your child is having an asthma attack
- Use this guide only if a doctor has told you your child has asthma
No previous asthma diagnosis or use of asthma medicines, see
Symptoms of Asthma
- Symptoms of an asthma attack are wheezing, a cough, tight chest, and trouble breathing.
- Wheezing is the classic symptom. Wheezing is a high-pitched whistling or purring sound. You can hear it best when your child is breathing out.
- The diagnosis of asthma requires attacks of wheezing that recur. The diagnosis is rarely made before 1 year of age.
Causes (Triggers) of Asthma Attacks
- Infections that affect breathing (like colds or the flu)
- Pollens (trees, grass and weeds)
- Animals (like cats or rabbits)
- Tobacco smoke
- Irritants (such as smog, car exhaust, menthol vapors, barns, dirty basement)
- Food Allergy (Serious). Asthma attacks caused by food allergy can be life-threatening (anaphylaxis). Examples are nuts or fish.
Asthma Attack Scale
- Mild: No Shortness of Breath (SOB) at rest. Mild SOB with walking. Can talk normally. Speaks in sentences. Can lay down flat. Wheezes not heard or mild. (Green Zone: Peak Flow Rate 80-100% of normal rate)
- Moderate: SOB at rest. Speaks in phrases. Wants to sit (can't lay down flat). Wheezing can be heard. Retractions are present (ribs pull in with each breath). (Yellow Zone: Peak Flow Rate 50-80% of normal rate)
- Severe: Severe SOB at rest. Speaks in single words. Struggling to breathe. Wheezing may be loud. Rarely, wheezing is absent due to poor air movement. Retractions may be severe. (Red Zone: Peak Flow Rate less than 50% of normal rate)
- Peak Flow Meter: a peak flow meter measures Peak Flow Rates (PFR). It tells us how well a person can move air out of the lungs. A PFR can be used in children 6 years and older.
When to Call for Asthma Attack
Call 911 Now
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Self Care at Home
|
Call 911 Now
- Wheezing and life-threatening allergic reaction to similar substance in the past
- Start to wheeze suddenly after a bee sting, taking medicine, or eating an allergic food
- Severe trouble breathing (struggling for each breath, can barely speak or cry)
- Passed out
- Lips or face are bluish when not coughing
- You think your child has a life-threatening emergency
Call Doctor or Seek Care Now
- Pulse oxygen level less than 90% during asthma attack
- Lips or face have turned bluish during coughing
- Ribs are pulling in with each breath (retractions)
- PEFR is 50-80% of normal rate after using nebulizer or inhaler (Yellow Zone)
- Wheezing not gone 20 minutes after using neb or inhaler
- Breathing is much faster than normal
- Nonstop coughing not better after using nebulizer or inhaler
- Severe chest pain
- Need to use asthma medicine (neb or inhaler) more often than every 4 hours
- Fever over 104° F (40° C)
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Call Doctor Within 24 Hours
- Mild wheezing lasts more than 24 hours on neb or inhaler treatments
- Sinus pain (not just congestion)
- Fever lasts more than 3 days
- Fever returns after being gone more than 24 hours
- You think your child needs to be seen, but the problem is not urgent
Call Doctor During Office Hours
- Don't have written asthma action plan from your doctor
- Use an inhaler, but don't have a spacer
- Miss more than 1 day of school per month for asthma
- Asthma limits exercise or sports
- Asthma attacks wake child up from sleep
- Use more than 1 inhaler per month
- No asthma check-up in more than 1 year
- You have other questions or concerns
Self Care at Home
- Mild asthma attack
Care Advice for Asthma Attack
-
What You Should Know About Asthma:
- Over 10% of children have asthma.
- Your child's asthma can flare up at any time.
- When you are away from your home, always take your child's medicines with you.
- The sooner you start treatment, the faster your child will feel better.
- Here is some care advice that should help.
-
Asthma Quick-Relief Medicine:
- Your child's quick-relief (rescue) medicine is albuterol or xopenex.
- Start it at the first sign of any wheezing, shortness of breath or hard coughing.
- Give by inhaler with a spacer (2 puffs each time) or use a neb machine.
- Repeat it every 4 hours if your child is having any asthma symptoms.
- Never give it more often than 4 hours without talking with your child's doctor.
- Coughing. The best "cough med" for a child with asthma is always the asthma medicine. Caution: Don't use cough suppressants. If over 6 years old, cough drops may help a tickly cough.
- Caution: If the inhaler hasn't been used in over 7 days, prime it. Test spray it twice into the air before using it for treatment. Also, do this if it is new.
- Use the medicine until your child has not wheezed or coughed for 48 hours.
- Spacer. Always use inhalers with a spacer. It will get twice the amount of medicine into the lungs.
-
Asthma Controller Medicine:
- Your child may have been told to use a controller drug. An example is an inhaled steroid.
- It's for preventing attacks and must be used daily.
- During asthma attacks, keep giving this medicine to your child as ordered.
-
Allergy Medicine for Hay Fever:
- For signs of nasal allergies (hay fever), it's okay to give allergy medicine. Reason: Poor control of nasal allergies makes asthma worse.
-
Fluids - Offer More:
- Try to get your child to drink lots of fluids.
- Goal: Keep your child well hydrated.
- Reason: It will loosen up any phlegm in the lungs. Then it's easier to cough up.
-
Humidifier:
- If the air in your home is dry, use a humidifier. Reason: Dry air makes coughs worse.
-
Avoid Tobacco Smoke:
- Tobacco smoke makes asthma much worse.
- Don't let anyone smoke around your child.
-
Avoid or Remove Triggers:
- Shower to remove pollens or other allergens from the body and hair.
- Avoid known causes of asthma attacks (such as smoke or cats).
- During attacks, reduce exercise or sports if it makes your child's asthma worse.
-
What to Expect:
- If treatment is started early, most asthma attacks are quickly brought under control.
- All wheezing should be gone by 5 days.
-
Inhaler With a Spacer: How to Use
- Step 1. Shake the inhaler well. Then attach it to the spacer (holding chamber).
- Step 2. Breathe out completely and empty the lungs.
- Step 3. Close the lips and teeth around the spacer mouthpiece.
- Step 4. Press down on the inhaler. This will put one puff of the medicine in the spacer.
- Step 5. Breathe in slowly until the lungs are full.
- Step 6. Hold a deep breath for 10 seconds. Allow the medicine to work deep in the lungs.
- If your doctor has ordered 2 or more puffs, wait 1 minute. Then repeat steps 1-6.
-
Metered Dose Inhaler (MDI): How to Use Without a Spacer (if you don't have one)
- Step 1. Shake the inhaler well.
- Step 2. Breathe out completely and empty the lungs.
- Step 3. Close the lips and teeth around the inhaler mouthpiece.
- Step 4. Press down on the inhaler to release a puff. Do this just as your child starts to breathe in.
- Step 5. Breathe in slowly until the lungs are full.
- Step 6. Hold a deep breath for 10 seconds. Allow the medicine to work deep in the lungs.
- If your doctor has ordered 2 or more puffs, wait 1 minute. Then repeat steps 1-6.
- Ask your doctor for a spacer if you don't have one. It will help send more medicine into the lungs.
- Older children who don't like a spacer can be prescribed an albuterol dry powder device.
-
Home Nebulizer: How to Use:
- A nebulizer machine changes a liquid medicine (med) into a fine mist. The fine mist can carry the med deep into the lungs. This is called a nebulizer (neb) treatment.
- Step 1. Prepare the medicine. First, wash your hands with soap and water. For pre-mixed single dose vials, just add one vial to the neb holding cup. For multi-dose vials, you need to do the mixing. First, add the correct amount of normal saline to the neb cup. Then carefully measure and add the correct amount of medicine to the saline.
- Step 2. Connect the nebulizer to the air compressor tubing. The air compressor is run by electricity. Portable ones run on a battery. Compressors make the jet of air that turns the medicine into a fine mist.
- Step 3. Turn on the air compressor. It will start making the fine mist that your child needs.
- Step 4 for an Older Child. Place the mouthpiece between your child's teeth and seal with the lips. Ask your child to breathe slowly and deeply. Ask your child to hold a deep breath for 10 seconds once a minute.
- Step 4 for a Younger Child. If your child refuses the mouthpiece, use a face mask. It should cover the nose and mouth. It should fit snugly.
- Step 5. Continue the treatment until the med is gone. If the med sticks to the side of the cup, shake it a little. An average neb treatment takes 10 minutes.
- Step 6. After each treatment, take the nebulizer apart. Rinse and clean it as directed. Reason: It can't produce mist if it becomes clogged up.
- Caution: Closely follow your doctor's instructions. Use the exact amount of med your doctor ordered. Don't give a neb treatment more often than every 4 hours.
-
Call Your Doctor If:
- Trouble breathing occurs
- Asthma quick-relief medicine (neb or inhaler) is needed more than every 4 hours
- Wheezing lasts over 24 hours
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.
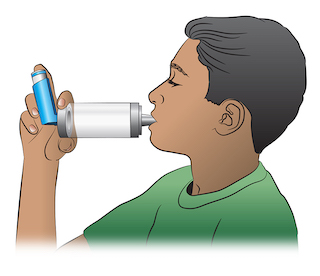
A spacer (or holding chamber) can be useful for all people with asthma. A spacer makes it easier to correctly inhale the asthma medicine from the metered dose inhaler (MDI). A spacer is very useful in younger children and older adults.
- STEP 1 - Shake the inhaler and then attach it to the spacer (holding chamber).
- STEP 2 - Breathe out completely.
- STEP 3 - Place the mouthpiece of the spacer in your mouth.
- STEP 4 - Press down on the inhaler. This will put one puff of the medicine in the holding chamber or spacer.
- STEP 5 - Breathe in slowly for 5 seconds.
- STEP 6 - Hold your breath for 10 seconds and then exhale.
- If your doctor has prescribed two or more puffs, wait 1 minute between each puff and then repeat steps 1-6.
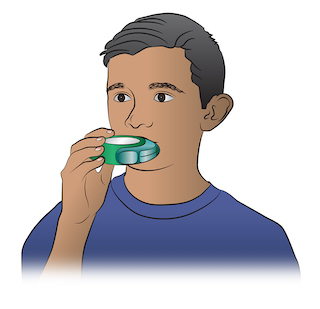
Dry powder inhalers require a different inhaling technique than regular metered dose inhalers (MDI). To use a dry powder inhaler, it is important to close your mouth tightly around the mouthpiece of the inhaler and to inhale rapidly. Here are the steps:
- STEP 1 - Remove the cap and follow package instructions to load a dose of medicine.
- STEP 2 - Breathe out completely.
- STEP 3 - Put the mouthpiece of the inhaler in the mouth.
- STEP 4 - Breathe in quickly and deeply.
- STEP 5 - Hold your breath for ten seconds to allow the medicine to reach deeply into your lungs.
- If your doctor has prescribed two or more inhalations, wait 1 minute and then repeat steps 2-5.
Back Pain
Is this your child's symptom?
- Pain or discomfort in the upper, mid or lower back
- Minor muscle strain from overuse and back injury are included
If NOT, try one of these:
Causes of Back Pain
- Strained Back Muscles. New backaches in teens are mostly from strained back muscles (muscle overuse). The pain is mostly in the lower back and near the center. There are 200 muscles in the back that allow us to stand upright.
- Work Triggers. Carrying something too heavy or lifting from an awkward position can cause back pain. Bending too far backward or sideways can cause back pain. Digging in the garden for too long causes overuse of back muscles.
- Exercise. New exercises or changes in an exercise routine can cause back pain. This is also called muscle overuse.
- Back Packs. In school-age children, heavy backpacks have become a common cause. They also can cause shoulder and neck pains. Children who have not gone into puberty are at greater risk. Reason: They lack the muscle mass.
- Kidney Infection (Serious). Pain is on one side in the middle of the back. Other symptoms are fever and pain when passing urine.
- Kidney Stone (Serious). Pain is on one side of the mid-back and shoots into the lower belly. The pain is extremely severe. The urine has blood in it.
- Sciatic Nerve Pain (Serious). Sciatica is pain caused by a pinched nerve in the lower back. Sciatica gives a burning pain in one buttock. The pain shoots into the back of the leg on that side. The most intense pain can be in the lower leg and foot. Leg weakness, numbness or tingling can also occur. A ruptured disk causes the pressure on the nerve. Sciatica is rare in children but common in adults.
Symptoms of Back Pain
- Strained back muscles cause most of these symptoms:
- The pain is in the middle or lower back
- The pain is made worse by bending
- The muscles near the spine are tender to the touch
- The muscles may be tight (in spasm)
Pain Scale
- Mild: Your child feels pain and tells you about it. But, the pain does not keep your child from any normal activities. School, play and sleep are not changed.
- Moderate: The pain keeps your child from doing some normal activities. It may wake him or her up from sleep.
- Severe: The pain is very bad. It keeps your child from doing all normal activities.
When to Call for Back Pain
Call 911 Now
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Self Care at Home
|
Call 911 Now
- Pain starts after major injury (such as a car crash or football). Caution: do not move your child until a spine board is put on.
- You think your child has a life-threatening emergency
Call Doctor or Seek Care Now
- Severe pain
- Pain shoots into the buttock or back of the thigh
- Tingling or numbness (loss of feeling) in the legs or feet
- Blood in urine
- Pain or burning when passing urine and fever
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Call Doctor Within 24 Hours
- Pain or burning when passing urine, but no fever
- Fever
- Walks different than normal for more than 3 days
- You think your child needs to be seen, but the problem is not urgent
Call Doctor During Office Hours
- Age is less than 5 years
- Pain in the upper back
- Cause is not clear (no history of overuse or twisting)
- Cause is bending backwards (such as in gymnastics)
- Back pain from overuse (exercise or work) lasts more than 2 weeks
- Back pains are a frequent problem
- You have other questions or concerns
Self Care at Home
- Strained back muscles (from exercise or work) present less than 2 weeks
Care Advice for Strained Back Muscles
-
What You Should Know About Back Pain:
- Most new lower back pain is caused by lifting heavy objects. Lifting while the back is twisted is a common cause. Muscle overuse from exercise also causes strained back muscles.
- Pain is not the only symptom. Walking a little bent over or stiff may occur for a few days.
- Here is some care advice that should help.
-
Pain Medicine:
- To help with the pain, give an acetaminophen product (such as Tylenol).
- Another choice is an ibuprofen product (such as Advil).
- Use as needed.
- Reason: Helps back pain and muscle spasms.
-
Cold Pack for Pain:
- For pain or swelling, use a cold pack. You can also use ice wrapped in a wet cloth.
- Put it on the sore muscles for 20 minutes.
- Repeat 4 times on the first day, then as needed.
- Reason: Helps with the pain and muscle spasms.
- Caution: Avoid frostbite.
-
Use Heat After 48 Hours:
- If pain lasts over 2 days, put heat on the sore muscle.
- Use a heat pack, heating pad or warm wet washcloth.
- Do this for 10 minutes, then as needed.
- Reason: Increase blood flow and improve healing.
- Caution: Avoid burns.
-
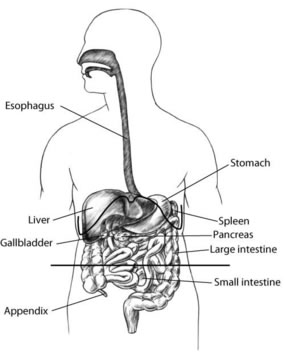
Sleep on the Side:
- Sleep on the side with a pillow between the knees.
- If your child only sleeps on the back, put a pillow under the knees.
- Avoid sleeping on the stomach.
- The mattress should be firm. Do not sleep on a waterbed.
-
Activity:
- Avoid any sports or work that increase the pain.
- Avoid lifting or jumping until well.
- After 48 hours, start gentle back stretching exercises.
- Complete bed rest is not needed.
-
Prevent Backpack Pain:
- Limit the weight of what is carried. It needs to less than 15% of body weight. That means a 100-pound (45 kg) child should not carry more than 15 pounds (7 kg).
- A sign of carrying too much weight is having to lean forward when walking.
- Buy a well-made backpack with wide, padded shoulder straps.
- Never carry the pack on just one shoulder. Reason: causes shoulder and neck pain.
-
What to Expect:
- New back pain without a reason most often goes away in a few days.
- Back pain from muscle overuse (strained back muscles) goes away in 1 to 2 weeks.
-
Call Your Doctor If:
- Pain becomes severe
- Walks different than normal for more than 3 days
- Pain starts to shoot into the leg
- Fever occurs
- Pain lasts more than 2 weeks
- You think your child needs to be seen
- Pain gets worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.
Bed Bug Bite
Is this your child's symptom?
- Bites from bed bugs
If NOT, try one of these:
Symptoms of Bed Bug Bites
- Usually cause itchy, red bumps in a group or line
- Often they look like a hive or mosquito bite
- Bite may have a red dot (puncture) in the center. This is where the bed bug bit through the skin.
- Occasionally, a small blister can occur in the center
- Bites are usually on exposed skin (arms, legs and face)
- Bites are usually first noted in the morning
Diagnosis of Bed Bug Bites
- Live bed bugs hide and are not usually seen. Close inspection of the mattress may find some.
- They are ¼ inch (6 mm), flat, oval shaped, reddish-brown bugs.
- Suspect bed bugs if over 3 red bumps in a row are on exposed skin. The bumps or bites are very itchy.
- Bed bug waste is found on bedding or mattress seams. It looks like dark brown flecks or coffee grounds.
- A blood stain on the sheet may sometimes be found. This is from a bug smashed after feeding.
Cause of Bed Bug Bite Reactions
- The skin bumps are the body's reaction to the bug's saliva.
- While the bug is sucking blood, some of its secretions get mixed in.
- Bed bugs are small visible blood-sucking bugs. They are about ¼ inch (6 mm) in length.
- During the day, bed bugs hide in the corners of mattresses. They may also be found in bed crevices, floors, and walls.
- At night, the bed bugs come out of hiding. They feed on humans for about 5 minutes.
Prevention of Getting Bed Bugs
- Over half of bed bug infestations within homes start after recent travel.
- Avoid hotels and hostels where bed bugs have been reported.
- When you check into a hotel room, look for signs of bed bugs. Look for flecks of their waste (like coffee grounds) in the bedding and mattress. If present, ask for another room.
- Keep your luggage and clothing on a luggage rack off the floor.
- When you return from a trip, place all travel clothing into the clothes dryer. Run the dryer for 20 minutes. (Reason: The heat will kill any bed bugs or their eggs that are present). One pregnant bed bug can spread bed bugs to an entire house.
Frequent Questions (FAQs)
- Can bed bugs transmit HIV or hepatitis? This is highly unlikely. It has never been reported.
- Do bed bugs like dirt? Not really. What bed bugs like is the warmth of the human body. Dirty and cluttered spaces just give bed bugs a place to hide.
- Are bed bugs too small to be seen? No. You can see adult bed bugs. They are about the size of an apple seed (4-7 mm; ¼ inch).
- Are bed bugs scared of the light? They do prefer darkness. But keeping the light on will not stop bed bugs from biting you.
When to Call for Bed Bug Bite
Call 911 Now
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Self Care at Home
|
Call 911 Now
- Life-threatening allergic reaction suspected. Symptoms include sudden onset of trouble breathing or swallowing.
- You think your child has a life-threatening emergency
Call Doctor or Seek Care Now
- Spreading red area or streak with fever
- Spreading red area or streak that's very large
- Your child looks or acts very sick
Call Doctor Within 24 Hours
- Painful spreading redness started more than 24 hours after the bite. Note: any redness starting in the first 24 hours is a reaction to the bite.
- More than 48 hours since the bite and redness gets larger
- You think your child needs to be seen
Call Doctor During Office Hours
- Severe itching not better after 24 hours of using steroid cream
- Scab that looks infected (drains pus or gets bigger) not better with antibiotic ointment
- After 7 days, bites not better
- After 14 days, bites not gone
- You have other questions or concerns
Self Care at Home
- Normal bed bug bite
Care Advice for Bed Bug Bites
-
What You Should Know About Bed Bug Bites:
- Bed bug bites cause itchy red bumps.
- They are usually less than ½ inch (12 mm) in size.
- Some are larger (like a hive). These are normal reactions to a bed bug.
- A large hive does not mean your child has an allergy.
- The redness does not mean the bite is infected.
- Bed bugs do not carry any infectious diseases.
- Don't panic: You can get rid of bed bugs from your home.
- Here is some care advice that should help.
-
Steroid Cream for Itching:
- To reduce the itching, use 1% hydrocortisone cream (such as Cortaid). No prescription is needed.
- Apply 3 times a day until the itch is gone.
- If you don't have, apply a baking soda paste until you can get some.
-
Allergy Medicine For Itching:
- If the bite is still itchy, try an allergy medicine by mouth.
- Benadryl is a good one. No prescription is needed.
-
Try Not to Scratch:
- Cut the fingernails short.
- Help your child not to scratch.
- Reason: Prevent a skin infection at the bite site.
-
Bed Bug Repellents - Not Helpful:
- Insect repellents do not keep bed bugs from biting.
- Repellents containing DEET (used on skin) and permethrin (used on clothing) do not help.
-
Removing Bed Bugs from Your Home:
- Getting rid of bed bugs requires a licensed pest control service.
- Look in the phone book or on the internet under Pest Control.
-
What to Expect:
- Any pinkness or redness usually lasts 3 days.
- The swelling may last 7 days.
- The itch may last for 2 weeks.
-
Call Your Doctor If:
- Bite looks infected (redness gets larger after 48 hours)
- Large red bumps last more than 7 days
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.

This is what a bed bug bite looks like. It can take a few days for the bites to appear after a bed bug bites you. The bites are usually itchy and often have a burning feeling. Try not to scratch and break the skin because this can cause an infection.

This is a full-grown bedbug. Bedbugs are small brown bugs which are less than ¼ of an inch (6 mm) long. Bedbugs hide in the seams, folds and creases of mattresses and upholstery. They come out at night. During the day, you might see signs of them, such as shed skin, waste or blood marks on the linens.
Bee or Yellow Jacket Sting
Is this your child's symptom?
- Sting from a bee, hornet, wasp, or yellow jacket
- Over 95 percent of stings are from honey bees or yellow jackets
- The main symptoms are pain and redness
If NOT, try one of these:
Cause of Bee Sting Reactions
- The bee's stinger injects venom into the skin.
- The venom is what causes the symptoms.
Local Skin Reactions to the Sting
- The main symptoms are pain, itching, swelling and redness at the sting site.
- Pain. Severe pain or burning at the site lasts 1 to 2 hours. Itching often follows the pain.
- Swelling. The bee sting may swell for 48 hours after the sting. The swelling can be small or large. Stings on the face can cause a lot of swelling around the eye. It looks bad, but this is not serious. The swelling may last for 7 days.
- Redness. Bee stings are often red. That doesn't mean they are infected. Infections rarely happen with stings. The redness can last 3 days.
Anaphylactic Reaction to the Sting
- A severe life-threatening allergic reaction is called anaphylaxis.
- The main symptoms are hives with trouble breathing and swallowing. It starts within 2 hours of the sting.
- This severe reaction to bee stings happens in 4 out of a 1,000 children.
- Hives. After a bee sting, some children just develop hives all over or face swelling. Hives or face swelling alone may be able to be treated at home. But, at times, these symptoms can also lead to anaphylaxis. Be sure to call your doctor now to help decide.
Prevention of Bee Stings
- Don't go barefoot if bees are around.
- Be careful in gardens and orchards.
- Insect repellents do not work against these stinging insects.
When to Call for Bee or Yellow Jacket Sting
Call 911 Now
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Self Care at Home
|
Call 911 Now
- Past severe allergic reaction to bee stings (not just hives) and stung less than 2 hours ago
- Wheezing or trouble breathing
- Hoarseness, cough or tightness in the throat or chest
- Trouble swallowing or drooling
- Speech is slurred
- Acts or talks confused
- Passed out (fainted) or too weak to stand
- You think your child has a life-threatening emergency
Call Doctor or Seek Care Now
- Sting inside the mouth
- Sting on the eye
- Stomach pain or vomiting
- More than 5 stings for 10 pounds (5 kg) of weight. In teens, more than 50 stings.
- Fever and sting looks infected (spreading redness)
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Call Doctor Within 24 Hours
- More than 48 hours since the sting and redness getting larger. Note: Infection is not common. It does not start until at least 24-48 hours after the sting. Redness that starts in the first 24 hours is due to venom.
- Swelling is huge (4 inches or 10 cm). It spreads across a joint such as the wrist.
- You think your child needs to be seen, but the problem is not urgent
Call Doctor During Office Hours
- You have other questions or concerns
Self Care at Home
- Normal reaction to bee, wasp, or yellow jacket sting
Care Advice for Bee or Yellow Jacket Sting
-
What You Should Know About Bee Stings:
- Bee stings are common.
- The main symptoms are pain and redness.
- The swelling can be large. This does not mean it's an allergy.
- Here is some care advice that should help.
-
Try to Remove the Stinger (if present):
- Only honey bees leave a stinger.
- The stinger looks like a tiny black dot in the sting.
- Use a fingernail or credit card edge to scrape it off.
- If the stinger is below the skin surface, leave it alone. It will come out with normal skin shedding.
-
Meat Tenderizer for Pain Relief:
- Make a meat tenderizer paste with a little water. Use a cotton ball to rub it on the sting. Do this once for 20 minutes. Reason: This may neutralize the venom and reduce the pain and swelling. Caution: Do not use near the eye.
- If you don't have any, use an aluminum-based deodorant. You can also put a baking soda paste on the sting. Do this for 20 minutes.
-
Cold Pack for Pain:
- If pain does not improve after using the meat tenderizer paste, rub with an ice cube.
- Do this for 20 minutes.
-
Pain Medicine:
- To help with the pain, give an acetaminophen product (such as Tylenol).
- Another choice is an ibuprofen product (such as Advil).
- Use as needed.
-
Steroid Cream for Itching:
- For itching or swelling, put 1% hydrocortisone cream (such as Cortaid) on the sting.
- No prescription is needed.
- Use 3 times per day.
-
Allergy Medicine for Itching:
- For hives or severe itching, give a dose of Benadryl.
-
What to Expect:
- Severe pain or burning at the site lasts 1 to 2 hours.
- Normal swelling from venom can increase for 48 hours after the sting.
- The redness can last 3 days.
- The swelling can last 7 days.
-
Call Your Doctor If:
- Trouble breathing or swallowing occurs (mainly during the 2 hours after the sting). Call 911.
- Redness gets larger after 2 days
- Swelling becomes huge
- Sting starts to look infected
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.

This photo shows the typical localized reaction to a bee sting. There is mild redness in an oval 4 inches (10 cm) wide of the left upper arm.

Moderate swelling of left hand from a bee sting that occurred the day before.
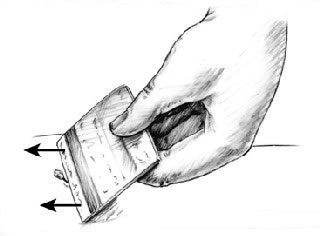
The stinger looks like as a tiny black dot in the center of the sting. There are several different methods of removal. Removing the stinger quickly is more important than the type of removal used.
- You can scrape it out with a credit card or finger nail.
- You can also use adhesive tape.
- If only a small fragment remains, don't worry about it. It will shed with the skin.
Special Notes:
- In many cases no stinger will be present.
- Only bees leave their stingers. Wasps, yellow jackets, and hornets do not.
Blisters
Is this your child's symptom?
- Raised pocket of fluid (usually clear) covered by skin
- Friction Blister: Friction blisters usually occur on the palms, fingers, heels or toes.
- Blood Blister: Raised pocket of bloody fluid, covered by skin. Dark red or purple in color. A blood blister can occur when the skin gets pinched (in a hinge or a closing door).
- Blisters when the cause is unknown are also covered.
If NOT, try one of these:
Causes of Blisters
- Friction Blisters. Friction is the most common cause of blisters.
- Burns - Chemical (Second-degree)
- Burns - Thermal (Second-degree)
- Frostbite (Second-degree)
- Hand-Foot-and-Mouth Disease. Viral rash from Coxsackie virus gives tiny blisters on palms and soles.
- Impetigo. Staph bacteria can cause impetigo with blisters.
- Insect Bites. In young children, insect bites (such as fleas) can cause small blisters.
- Poison Ivy, Poison Oak, Poison Sumac
- Sunburn (Second-degree)
- Staph Scalded Skin Syndrome (Serious). SSSS is caused by the Staph bacteria. The main finding is widespread large blisters.
Friction Blisters - Hands and Feet
- Friction causes most blisters on the hands and feet.
- A friction blister is a raised pocket of clear fluid covered by skin.
- Cause. A friction blister is the result of forces on the skin. Shear forces separate the top layer of the skin from the lower layer. This forms a cushion (blister) of fluid over the spot of friction or pressure.
- Common Sites. Fingers, palm, back of heel, top of toes, side of foot.
- Hand Friction Blisters. Hand blisters are often due to friction from using a tool too much. Examples are a shovel, pick, or rake. They can also be caused by sports equipment. Examples are a tennis racquet or boat oars. Gymnastics equipment (such as high bars) may also cause hand blisters.
- Foot Friction Blisters. Foot blisters are likely due to friction from an activity. Examples are hiking or running. Usually, a child has new shoes or poorly-fitting shoes. Children starting a new sport may develop blisters. Also, a risk factor to forming blisters is recently increasing the activity time.
- Prevention. There are two general approaches to prevent friction blisters. These are toughening the skin and lowering the friction force.
- Complications. Pain or infection.
- Treatment. Painless or mildly painful small blisters can be treated at home. Use moleskin or tape that has a hole cut in the center. Larger or very painful blisters sometimes need to be drained. This can be done by making a small hole in the blister. Use a clean needle or pin. Let all the blister fluid drain out. Then the blister can be covered with antibiotic ointment and a dressing.
When to Call for Blisters
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Self Care at Home
|
Call Doctor or Seek Care Now
- Fever and looks infected (spreading redness)
- Widespread blisters
- Cause not clear and blisters on face
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Call Doctor Within 24 Hours
- Looks infected (spreading redness or pus)
- Severe pain and you want your doctor to drain the blister
- Cause not clear and blister on one or more finger pads
- Cause not clear and new blisters are developing
- You think your child needs to be seen, but the problem is not urgent
Call Doctor During Office Hours
- No new blisters but cause not clear
- You have other questions or concerns
Self Care at Home
- Normal blister from friction
- Normal blood blister from pinch injury to skin
- Questions about prevention of foot blisters from hiking or running
- Questions about prevention of hand blisters from sports or tools
Care Advice
Treatment of Normal Friction Blister
-
What You Should Know - Friction Blister:
- A friction blister is a raised pocket of clear fluid, covered by skin.
- Most blisters should not be opened. Reason: It increases the risk of infection.
- However, large or severely painful blisters often need to be drained. This is done by poking a small hole in the blister with a needle. (See #4 below)
- Here is some care advice that should help.
-
Protect the Blister:
- Goal: Protect the blister from any more rubbing.
- Surround it with a "donut" made from moleskin. Ask for this product at your drug store.
- Using scissors, cut a moleskin piece to a shape larger than the blister.
- Next cut a hole the size of the blister in the center. Do this by folding the moleskin in half and cut along the fold.
- Remove the covering from the sticky side. Then, put the moleskin on with the blister in the center.
- If the blister is taller than the moleskin, add one more layer of moleskin.
- Hold the "donut" in place with a large strip of duct tape.
- Other option. If you don't have moleskin, use a bandage (such as Band-Aid). Fold it and cut the center out to the size of the blister.
- For foot blisters, also switch to shoes that don't rub the blister.
-
Pain Medicine:
- To help with the pain, give an acetaminophen product (such as Tylenol).
- Another choice is an ibuprofen product (such as Advil).
- Use as needed.
-
Severe Pain - Drain the Blister:
- Draining a large blister can help make the pain go away.
- Wash the skin with warm water and soap.
- Clean a needle or straight pin with rubbing alcohol.
- Gently press the fluid to one side of the blister to create a bulge.
- Pass the needle sideways through the fluid making 2 puncture holes. Gently wiggle the needle to make the holes larger.
- Remove the needle.
- Press the fluid out through the holes.
- Leave the roof of the blister in place to protect the raw skin underneath.
- Use an antibiotic ointment (such as Polysporin). No prescription is needed. Put it on twice per day after cleansing.
- Cover the drained blister with a bandage (such as Band-Aid).
-
Broken Blister Treatment:
- If the blister breaks open, let it drain.
- Leave the roof of the blister in place to protect the raw skin underneath.
- If there are any loose flaps of skin, trim them with a fine scissors.
- Wash it with warm water and soap.
- Use an antibiotic ointment (such as Polysporin). No prescription is needed. Put it on twice a day.
- Cover it with a bandage (such as Band-Aid).
-
What to Expect:
- Most often, they dry up and peel off without any treatment.
- This may take 1 to 2 weeks.
-
Call Your Doctor If:
- Blister looks infected
- Severe pain and you want your child's doctor to drain the blister
- You think your child needs to be seen
- Your child becomes worse
Treatment of Normal Blood Blister
-
What You Should Know - Blood Blister:
- A blood blister can happen when the skin gets pinched. Examples are a finger caught in a hinge or a closing door.
- It forms a tiny pocket of bloody fluid covered by skin. It is dark red or purple in color.
- A blood blister is not harmful.
- No treatment is needed. You do not need to drain it.
- It will slowly dry up and peel off over 1-2 weeks.
-
Pain Medicine:
- To help with the pain, give an acetaminophen product (such as Tylenol).
- Another choice is an ibuprofen product (such as Advil).
- Use as needed.
-
Call Your Doctor If:
- You think your child needs to be seen
- Your child becomes worse
Prevention of Foot Blisters
-
Prevention - General:
- Shoes. Buy shoes that fit. Do not wear shoes that are too tight or too loose. New hiking boots are often somewhat stiff. It is wise to first wear them around the house and on short walks. Wear them in before wearing them on a long hike.
- Socks. Do not use cotton socks. They tend to stay damp when wearing. Instead use synthetic (acrylic) or wool socks. Some people prefer to wear two socks at a time. You can wear a thin inner liner ('wicking') sock and a thicker outer sock.
- Lubricants. If your child often gets blisters at the same spot, use a lubricant. You can use petroleum jelly (such as Vaseline). Cover the area with a small amount of the lubricant before sports. This will help to reduce friction on the spot.
- Callus. If blisters usually occur under a callus, file the callus down. Then, lubricate it. This way it won't add to the friction.
- Taping Pressure Points. If a lubricant doesn't stop blisters, taping is the next step. Taping is a very good way to treat hot spots for friction blisters. Many hikers and runners use taping. Follow the instructions listed down below.
-
Prevention - Taping:
- Option 1 - Moleskin
- You can get moleskin at your drug store. It is a good way to stop friction blisters. Here are some instructions on how to use moleskin.
- Using scissors, cut the moleskin to a shape slightly larger than the pressure point.
- Remove the backing from the moleskin. Put it on the pressure point. Smooth it from the center outward so that there are no wrinkles.
- Put on a clean and dry sock.
- Option 2 - Taping with Duct Tape
- Duct tape is available at your hardware store. It is also good at stopping friction blisters. Many hikers and runners use it. Here are some instructions on how to use duct tape.
- Using scissors, cut out a piece of duct tape into a shape slightly larger than the pressure point.
- Apply the piece of duct tape to the pressure point. Smooth it from the center outward so that there are no wrinkles.
- Put on a clean and dry sock.
-
Prevention - Toughening the Skin:
- This mainly applies to walkers, hikers, and runners.
- Slowly add to the distance you hike or run over days to weeks. This will increase the toughness of the skin. It will lower the risk of blisters forming.
-
Call Your Doctor If:
- You have other questions or concerns
Prevention of Hand Blisters
-
Prevention:
- Gloves. Wear heavy-duty work gloves when working with the hands. Also, use gloves when working with tools. Examples are shovels, picks, and rakes. Sports gloves can be used for rowing, paddling, weight lifting or cycling.
- Lubricants. Lower friction at pressure points by covering them with a lubricant. You can use petroleum jelly (such as Vaseline).
-
Call Your Doctor If:
- You have other questions or concerns
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.
Bottle-Feeding (Formula) Questions
Is this your child's symptom?
- Formula and bottle-feeding questions
Breastfed, see
Topics Covered for Formula Feeding
If your baby is healthy, skip the "What to Do" section. Go directly to the topic number that relates to your question for advice:
- Types of formulas
- Switching formulas and milk allergies
- Powdered versus liquid formulas
- Whole cow's milk, 2%, 1% and skim milk
- Vitamins and iron
- Water to mix with the formula
- Extra water
- Amounts: how much per feeding?
- Schedules or frequency of feedings
- Length of feedings
- Night feedings: how to eliminate?
- Formula temperature
- Formula storage
- Cereals and other solids
- Burping
- Baby bottle tooth decay
- Traveling
- Nipples and bottles
- Normal stools
- Breast discomfort
When to Call for Bottle-Feeding (Formula) Questions
Call 911 Now
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Self Care at Home
|
Call 911 Now
- Can't wake up
- Not moving or very weak
- You think your child has a life-threatening emergency
Call Doctor or Seek Care Now
- Hard to wake up
- Too weak to suck
- Age less than 1 month old and looks or acts abnormal in any way
- Dehydration suspected. No urine in more than 8 hours, dark urine, very dry mouth and no tears.
- Will not drink or drinks very little for more than 8 hours
- Age less than 12 weeks old with fever. Caution: do NOT give your baby any fever medicine before being seen.
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Call Doctor Within 24 Hours
- Does not seem to be gaining enough weight
- You think your child needs to be seen, but the problem is not urgent
Call Doctor During Office Hours
- You have other questions or concerns
Self Care at Home
- Bottle-feeding question about a healthy baby
Care Advice for Bottle (Formula) Feeding
-
Types of Formulas:
- Milk-protein formulas, soy-protein formulas, and hydrolysate formulas
- Soy formulas don't contain lactose or cow's milk protein. Currently, 20% of infants in the U.S. are fed soy formula. Often, switching to soy is not done with a valid reason.
- Hydrolysate formulas mean the protein is broken down. These are advised when children are sensitive to both soy and milk protein.
-
Switching Formulas and Milk Allergies:
- Switching from one milk-based formula to another is not helpful for any symptom. It is also not harmful.
- Switching from milk formula to soy formula is sometimes helpful for severe diarrhea. This may occur from temporary low lactase levels. It may also be used for those families who are vegetarian.
- Switching from milk formula to soy is sometimes helpful for cow's milk allergy. A cow's milk allergy occurs in 1-2% of infants. Most often, protein hydrolysate formulas (such as Alimentum) are advised. This is because 15% of these infants are also allergic to soy protein.
- Switching formulas for frequent crying, spitting up or gas is rarely helpful.
- Don't switch formulas without talking with your child's doctor.
-
Powdered versus Liquid Formulas:
- Formulas come in 3 forms: powder, concentrated liquid and ready-to-feed liquid.
- Concentrated formulas are mixed 1:1 with water.
- Ready-to-feed formulas do not need any added water.
- Powdered formulas are mixed 2 ounces (60 mL) of water per each level scoop of powder. Never add extra water because dilute formula can cause a seizure.
- Powdered formula costs the least. Ready-to-feed formula costs the most.
- Powdered formula is the easiest to use to supplement breastfeeding.
- Ready-to-feed formula is the easiest to use for traveling.
-
Whole Cow's Milk, 1%, 2% and Skim Milk:
- Cow's milk should not be given to babies before 12 months of age. Reason: Raises risk of iron deficiency anemia.
- Skim milk (fat free milk), 1% low fat milk or 2% milk should not be used before 2 years. Reason: The fat content of whole cow's milk (3.5%) is required. It is needed for rapid brain growth.
-
Vitamins and Iron:
- For all infants, use a formula that has iron in it. This helps to prevent iron deficiency anemia.
- The iron amount in iron-fortified formulas is too small to cause any symptoms. Iron in formulas does not cause constipation or diarrhea.
- Iron-fortified formulas contain all the vitamins and minerals needed.
- Extra vitamins are therefore not needed for infants taking formula.
- Fluoride. Babies no longer need to take fluoride drops. Reason: the fluoride in toothpaste works very well. For children at high risk for tooth decay, your dentist may use fluoride varnish.
-
Water to Mix With the Formula:
- Most city water supplies are safe for making 1 bottle at a time. Run the cold tap water for 1 minute. Don't use warm tap water. (Reason: To avoid potential lead exposure). Heat cold water to desired temperature. Add this to powder or formula concentrate.
- Exceptions:
- Untested well water or
- City water with recent contamination or
- Developing countries with unsafe water supply or
- Your child has decreased immunity.
- For these conditions, use distilled water, bottled water, or filtered tap water.
- Another option is to use city water or well water that has been boiled. Boil for 10 minutes. Add 1 extra minute per each 1,000 feet (305 meters) of elevation.
- Bottled water costs more than distilled water.
- If making a batch of formula, distilled, bottled or boiled water is needed.
-
Extra Water:
- Babies usually do not need extra water. (Reason: regular formula is 85% water)
- Too much water can cause seizures.
- You can offer some water if weather is very hot.
- Don't give more than 4 ounces (120 mL) of extra water per day. Limit extra water during the first 6 months of life. Exception: Don't give any during the first month.
- After starting solid foods, babies need more water.
-
Amounts - How Much Per Feeding:
- The average amount of formula that babies take per feeding is:
- Newborn: 2-3 ounces (60-90 mL) per feeding
- 1 month old: 4 ounces (120 mL) per feeding
- 2 months old: 5 ounces (150 mL) per feeding
- 4 months old: 6 ounces (180 mL) per feeding
- 6 months old: 7-8 ounces (210-240 mL) per feeding
- The amount can vary depending on the baby's weight and if the baby is going through a growth spurt.
- A baby's appetite varies throughout the day. If the infant stops feeding or loses interest, the feeding should be stopped.
- If healthy babies are not hungry at several feedings, increase the feeding interval.
- The most amount of formula advised per day is 32 ounces (1 liter).
- Over-feeding can cause vomiting, diarrhea or too much weight gain.
- If your baby needs over 32 ounces (1 liter), talk to your doctor about starting solids.
- Get rid of any formula left in bottle at end of each feeding. Do not reuse this leftover formula. Reason: Contains germs that can grow.
-
Frequency of Feedings (Schedules): Babies mainly need to be fed when they are hungry. If your baby is fussy and it's been more than 2 hours, feed him. Some guidelines are listed below:
- From birth to 3 months of age, feed every 2 to 3 hours.
- From 3 to 9 months of age, feed every 3 to 4 hours.
- Infants often set their own schedule by 1 to 2 months of age.
-
Length of Feedings:
- Feedings shouldn't take more than 20 minutes.
- If the feeding is prolonged, check the nipple to be sure it isn't clogged.
- A clean nipple should drip about 1 drop per second. Check this when the bottle of formula is turned upside down.
-
Night Feedings - How to Get Rid of Them:
- Most newborns need to be fed at least twice each night.
- Most formula-fed babies give up night feedings by 4 months of age. The tips below can help your baby sleep for longer stretches during the night:
- Keep daytime feeding intervals to at least 2 hours. Slowly stretch them to 3 hours.
- During daytime, your baby shouldn't sleep for more than 3 hours at a time. If your baby naps longer than that, wake him for a feeding.
- Place your baby in the crib drowsy but awake. Don't bottle-feed or rock until asleep.
- Make middle-of-the-night feedings brief and boring compared to daytime feedings. Don't turn on the lights or talk to your child. Feed him rather quickly.
-
Formula Temperature:
- Most babies like formula at body temperature.
- In the summertime, some infants prefer formula that's cooler.
- In the wintertime, some prefer warm formula.
- The best temperature is the one your infant prefers. Either way, there's no health risk involved.
- Just make sure the formula is not too hot. Reason: It can burn your baby's mouth.
-
Formula Storage:
- If you can, make your child's formula fresh for each feed. However, if formula needs to be made ahead of time:
- Prepared formula should be stored in the refrigerator. It must be used within 24 hours.
- Open cans of formula should also be kept in the refrigerator. They should be covered and used within 24 hours.
- Prepared formula left at room temperature for more than 1 hour should be discarded.
- Leftover used formula should always be tossed. Reason: Contains germs that can grow.
-
Cereals and Other Solids:
- Bottle-fed infants should be started on baby foods between 4 and 6 months. First baby foods can be cereals and/or fruit.
- Starting before 4 months is not needed. Starting before 4 months makes feedings messier and longer. Early use of solids can also cause gagging.
- Solids don't increase sleeping through the night for bottle-fed infants.
- Delaying solids past 9 months of age is not advised. The delay runs the risk that your infant will refuse solids.
-
Burping:
- It is not harmful if a baby doesn't burp.
- Burping is an option, but not required.
- It can decrease spitting up, but it doesn't lessen crying.
- Burping can be done twice per feeding, once midway and once at the end.
- If your baby does not burp after 1 minute of patting, it can be stopped.
-
Baby Bottle Tooth Decay:
- Some older infants and toddlers are used to a bottle before sleeping.
- Falling asleep with a bottle of milk or juice can cause severe tooth decay.
- Prevent this bad habit by not using the bottle as a pacifier. Also, do not use the bottle as a security object.
- If you cannot stop the bottles, fill it with water. Use water instead of formula or milk at bedtime.
-
Traveling:
- Use bottles of ready-to-feed formula (most expensive).
- Or mix formula ahead of travel and carry in a cold insulated container.
- Or use powered formula. Put the required number of scoops in a bottle. Carry clean water in a separate bottle. Mix before each feeding.
-
Nipples and Bottles:
- Any nipple/bottle products are fine.
- It is not necessary to sterilize bottles or nipples. Wash them with soap and water. Rinse them thoroughly.
- It is also safe to wash bottles and nipples in the dishwasher.
-
Formula-fed Stools, Normal:
- Meconium Stools are dark greenish-black, thick and sticky. They normally are passed during the first 3 days of life.
- Transitional Stools are a mix of meconium and milk stools. They are greenish-brown and looser. They are passed day 4 to 5 of life.
- Normal Milk Stools without any meconium are seen from day 6 on.
- Formula-fed babies pass 1 to 8 stools per day during the first week. Then it starts to slow down to 1 to 4 per day. This lasts until 2 months of age.
- The stools are yellow in color and thick like peanut butter. Green stools are also normal (usually caused by bile).
- After 2 months of age, most babies pass 1 or 2 stools per day. They can also pass 1 every other day. They are soft and solid.
-
Breast Discomfort in Bottle-feeding Mothers:
- Even though you chose not to breastfeed, your breasts will make milk. Breast milk comes in on day 2 or 3. Swollen breasts can be painful for a few days. Here is what to do:
- Ibuprofen. Take 400 mg of ibuprofen (such as Advil) 3 times per day. This will help to lessen pain and swelling. There's no special prescription medicine for this.
- Cold Pack. Use a cold pack or ice bag wrapped in a wet cloth. Put it on your breasts for 20 minutes. Do this as often as needed. This will decrease milk production. Do not use heat. Heat will increase milk production.
- Pumping. For moderate pain, hand express or pump off a little breast milk. This will help to reduce your pain. Pumping breast milk can increase milk production. But, doing this to take the edge off your discomfort is not harmful.
- Bra. Wear a bra that offers good breast support or a sports bra. Wear it 24 hours a day.
- Binding. Binding the breasts by wearing a tight bra is no longer advised. Binding by using an elastic wrap is also not advised. Binding can increase the risk of breast infections (mastitis).
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.
Breast-Feeding Questions
Is this your child's symptom?
- Breastfeeding questions
Formula fed, see
Topics Covered for Breast-Feeding
If your baby is healthy, skip the "What to Do" section. Go directly to the topic number that relates to your question for advice:
- How often to feed to bring in the milk supply
- Length of feedings to bring in the milk supply
- Length of feedings after milk supply is in
- Signs of adequate milk supply (Do I have enough milk?)
- How to increase milk supply
- Supplemental formula
- When to introduce a bottle
- Extra water
- Severe engorgement (generalized swelling and pain) of both breasts
- Blocked milk ducts (1 or more tender lumps in the breast)
- Sore or cracked nipples
- Mother's medicines
- Mother's smoking or tobacco use
- Mother's diet
- Sick infants
- Sick mother (with illness)
- Normal stools during the first weeks of life
- Normal infrequent breast milk stools after 1 month of age
- Leaking breast milk
- Vitamin D for breastfed baby
- Storage of pumped milk
- Burping
- Milk letdown that causes pulling away, coughing or choking
- Cereals and other solids (baby foods)
- When to Call Your Doctor
Expert Reviewers:
Maya Bunik, M.D., Lisbeth Gabrielski, RN, and Marianne Neifert, M.D., Lactation specialists
When to Call for Breast-Feeding Questions
Call 911 Now
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Self Care at Home
|
Call 911 Now
- Can't wake up
- Not moving or very weak
- You think your child has a life-threatening emergency
Call Doctor or Seek Care Now
- Hard to wake up
- Too weak to suck
- Age less than 1 month old and looks or acts abnormal in any way
- Dehydration suspected. No urine in more than 8 hours, dark urine, no stool for 24 hours, very dry mouth and no tears.
- Will not breastfeed or takes very little for more than 8 hours
- Looks deep yellow or orange
- Age less than 12 weeks old with fever. Caution: do NOT give your baby any fever medicine before being seen.
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Call Doctor Within 24 Hours
- Does not seem to be gaining weight by day 5
- Yellow seedy stools are less than 3 per day. Exception: before 5 days of life while milk is coming in, this can be normal. Also, after 4 weeks of age can be normal.
- Day 2-4 of life and no stool in more than 24 hours
- Wet diapers are less than 6 per day. Exception: Before 5 days of life while milk is coming in.
- Day 2-4 of life and no urine in more than 8 hours
- The mother has signs of breast infection (red, tender lump on breast). Exception: localized engorgement.
- You think your child needs to be seen, but the problem is not urgent
Call Doctor During Office Hours
- Hungry after feedings. Reason: needs a weight check.
- Needs formula during first month. Reason: breastfeeding not going well.
- You have other questions or concerns
Self Care at Home
- Breastfeeding question about healthy baby
Care Advice for Breastfeeding
-
How Often to Feed to Bring in the Milk Supply:
- Every 1½ to 3 hours for the first month (8 to 12 times per day).
- During the day, wake your baby up if more than 3 hours have passed since the last feeding.
- During the night, wake your baby if more than 4 hours pass without a feeding.
- After 1 month of age, allow your baby to sleep longer. If your baby is gaining weight well, feed on demand and do not awaken for feedings.
-
Length of Feedings to Bring in the Milk Supply:
- Offer both breasts with each feeding
- Nurse 10 minutes on the first breast. Then, nurse up to 15 minutes on second breast if your baby is actively sucking.
- For each feeding, switch which breast you start on.
- Needing to stimulate your baby to take the second breast is normal.
-
Length of Feedings After Milk Supply is in: (by day 8 at the latest)
- On the first breast, allow your baby to nurse up to 20 minutes. Reason: To get the high-fat, calorie-rich hind milk.
- You can tell your baby has finished when the sucking slows down. Your breast should feel soft. Then offer the 2nd breast if your baby is interested.
- For each feeding, switch which breast you start on.
-
Signs of Good Milk Supply: (Is your baby getting enough breast milk?)
- Stools: 3 or more yellow seedy stools per day. Exception: 1 or 2 can be normal while the milk is coming in. Stools should start increasing by day 5 of life. See Care Advice #15 on Breastfed Stools for more information. Caution: Once the milk is in, infrequent stools are not normal. However, it can become normal after 4 weeks of age.
- Urine: 6 or more wet diapers per day. Exception: 3 wet diapers per day can be normal while milk is coming in. Wet diapers should start increasing by day 5 of life. Note: If you aren't sure about the diaper being wet, place a tissue in the diaper.
- Satisfied (not hungry) after feedings
- Breasts feel full before feedings and soft after feedings
- It is very important that your baby is latched on right. This way she can get enough milk. Look and listen for regular swallowing. This shows that your milk has letdown. Letdown is the release of breastmilk into the milk ducts just before a feeding. It starts after 2 to 3 weeks of nursing. At first, milk letdown may take 60 to 90 seconds of sucking before it starts.
-
How to Increase Milk Supply:
- Enough sleep (extra naps), reduced stress (ask for help), relaxed environment, good fluid intake
- Drink enough fluids to keep your urine pale yellow in color.
- Usually that means drinking at least 2 quarts (2 liters) of fluid per day.
- Increase how often you nurse. Limit the use of the pacifier.
- Pump the breasts for 10 minutes after each feeding. Do this for a few days (see lactation consultant). Electric breast pumps that are double-sided give the best results.
-
Supplemental Formula:
- Don't offer your baby any bottles of formula before 3 to 4 weeks old. Reason: It will interfere with creating a good milk supply.
- You should be nursing your baby every 2 hours (start to start). Reason: so your baby can get colostrum after birth.
- There are some exceptions. Medical indications to prevent dehydration or severe jaundice include the following:
- The milk is not in (day 3 - 4) and your baby is very hungry (especially preterms)
- Not enough wet or soiled diapers or
- Your baby is quite jaundiced. Reason: Prevents dehydration.
- After every breastfeeding for 1 or 2 days, give expressed breastmilk or formula. Give 1 ounce (30 mL) at a time. Also, see your child's doctor within 24 hours for a weight check.
-
When to Introduce a Bottle:
- When your baby is 4 weeks old, if your baby is nursing well, offer a bottle of pumped breastmilk (1 ounce or 30 mL). Do this once a day. This allows him to get used to a bottle and the nipple.
- If you wait too long (such as 8 weeks), many babies will reject bottle feedings.
- Once your baby accepts bottle feedings, use them at least once every 3 days. This insures that he will continue to accept them.
- Bottle acceptance allows you to leave your baby with a sitter. It's also essential if you plan on going back to work outside the home.
- You can use formula or pumped breast milk that has been refrigerated or frozen.
-
Extra Water:
- Never give extra water to infants younger than 6 months. Reason: Too much water can cause a seizure.
- It's not needed. Reason: Breast milk contains 88% water.
- If your baby gets enough breast milk, extra fluids are not needed. They may decrease your baby's interest and ability to breastfeed.
-
Engorgement (Generalized swelling and pain of both breasts):
- Engorgement usually begins 2 or 3 days after your baby's birth.
- Also, can start at any time when breasts are not emptied regularly.
- Breastfeed your baby more often. Do not use pacifiers.
- Remove a little milk before feeding your baby. Hand express or briefly use a breast pump.
- Gently squeeze the areola with your fingers at the start of each feeding. This will soften the areola and help your baby latch on. Milk release won't occur if your baby only latches on to the nipple.
- Pump your breasts when they hurt or when a feeding doesn't help discomfort. Also, pump when you must miss a feeding.
- Use a cold pack on the breasts between feedings. Cold cabbage leaves or a bag of frozen peas works well.
- Call your doctor or lactation consultant if: not better after 24 hours of this treatment.
-
Blocked Milk Ducts (tender lump in the breast):
- Caused by the breast not being emptied all the way
- Treatment goal: Open up the blocked milk ducts
- Breastfeed your baby more often. Do not use pacifiers.
- Before each breastfeeding session, use heat on the breast lump for 5 minutes. Do this with a hot shower, hot bath or heating pad.
- While feeding or pumping, massage the swollen areas toward the nipple.
- Try different breastfeeding positions which may drain the affected area (ducts) better.
-
Call Your Doctor If:
- Lump becomes red and very painful
- Fever occurs
- Not better after 24 hours of treatment
- Your baby starts acting sick
-
Sore or Cracked Nipples:
- Most often, due to friction from not latching on right. Can also be due to a non-areolar grasp on the breast.
- Clean with warm water once daily. Do not use soap which dries out the skin.
- For sore nipples, coat and lubricate nipple and areola with breast milk.
- For cracked nipples, use 100% lanolin after feedings. No prescription is needed. Exception: mother allergic to wool. Hydrogel pads are also good for healing.
- Help your baby latch on to as much of the areola as possible. Do this by compressing the areola. Proper latching-on should prevent nipple injury.
- Prevent the breast from pulling out of your baby's mouth. Support the breast from below during feedings.
- Start feedings on the side that is least sore.
- Limit feedings to less than 10 minutes on the sore side.
- Don't pull your baby off the nipple until she has released her grip. You can break the seal by placing your finger in the mouth between gums.
- Call your doctor if: not better after 24 hours of treatment.
-
Mother's Medicines:
- It's best to take your medicine at the end of a feeding. Reason: It will be out of your system by the next feeding.
- Most commonly used drugs are safe. Examples are penicillins, erythromycin, cephalosporins, stool softeners, cough drops, nose drops, eyedrops, and skin creams.
- Pain Medicines: Acetaminophen (such as Tylenol) and ibuprofen (such as Advil) are safe. Aspirin (325 mg) should not be used. Reason: risk for bleeding. Baby aspirin (81 mg daily) is safe to use for mothers who need it for health problems.
- Do not use decongestants. They can reduce milk production in some mothers. An example is Sudafed.
- Do not use sulfa drugs (Septra and Bactrim) for the first month. They are okay after the baby is 4 weeks old.
- Allergy medicines for allergy symptoms are OK during breastfeeding. Long-acting allergy medicines (such as Zyrtec) are preferred. They can be given as needed once per day at bedtime. Do not use combination products with decongestants.
- Birth control pills can decrease your milk volume. Make sure that your milk supply is well established (6 weeks or more) before starting. If you decide to use birth control, consult your doctor first.
- For all other drugs, call your doctor or check the LactMed Website (listed below).
- LactMed is a drug/lactation website. It provides information regarding the safety of medicines while nursing. It's on Toxnet. Toxnet is the toxicology data website of the National Library of Medicine.
- Infant Risk Call Center. Provides current information on the use of medications during pregnancy and breastfeeding. They answer calls Monday-Friday 8 am - 5 pm central time. (806)-352-2519. Website at Infant Risk Center.
-
Mother's Smoking or Tobacco Use:
- It is best not to use tobacco. But, if you must smoke, you can also breastfeed. Generally, the benefit of giving your baby your milk outweighs tobacco risks.
- The nicotine and its byproducts pass into the breast milk. This may cause your baby not to sleep well and increase the heart rate. It can also cause loose stools. Heavy tobacco use (over ½ pack per day) can decrease your milk supply. It may also affect letdown.
- Smoking cessation aids pose no more problems for the breastfed baby than smoking. Use as directed.
- If you smoke, do not smoke around your baby.
-
Mother's Diet:
- Foods: Eat a diet that is varied and balanced. No special foods should be eaten or not eaten. The effect on the baby of foods in the mother's diet is overrated. Foods eaten in moderate amounts most often cause no effects.
- Honey: Honey is safe for breastfeeding moms to eat. It is also safe to use to treat coughing in the mother. Botulism isn't transmitted through breast milk.
- Caffeine: Caffeine is found in coffee, tea or soft drinks. Too much caffeine can cause your baby to not sleep well. It can also cause increased crying or even diarrhea. Limit caffeine drinks to two 8 ounce (240 mL) servings per day.
- Alcohol: It is best not to use alcohol during breastfeeding. Too much alcohol can cause your baby to be sleepy. It can also affect your milk letdown. If you must drink, limit to an occasional drink of beer or wine. Max: no more than 1 per day. Nurse your baby before you drink. Wait at least 2 hours before nursing again.
-
Sick Infants:
- Do not stop breastfeeding for vomiting, spitting up, diarrhea, cough, or jaundice. See the care guide for that symptom.
- Keep breastfeeding when possible.
-
The Mother is Sick (has an acute illness):
- Continue breastfeeding, even if you have a fever.
- Reason: Breast milk carries your antibodies. These can protect your baby from the full-blown infection.
- Try to prevent the spread of infection by good hand washing. Do this after blowing your nose (for colds) or after stools (for diarrhea).
- There are few medical conditions in the mother when breastfeeding is not advised. Some of these are AIDS, Herpes simplex rash (fever blisters) on the nipple/areola, drug abuse and tuberculosis. Talk with your doctor.
- Fever Blisters on Mom's Mouth. Fever blisters (cold sores) on the lips are caused by the herpes virus. Herpes can cause serious infections in young babies. It's safe to continue breastfeeding if they are on your (mom's) lips. But avoid kissing or nuzzling your baby until fever blisters are completely dried up.
-
Breastfed Stools During the First Weeks of Life:
- Meconium Stools are dark greenish-black, thick and sticky. They are passed during the first 2 days of life.
- Transitional Stools (a mix of meconium and milk stools) are greenish-brown and loose. They are passed day 3 to 4 of life. While breast milk is coming in, babies have about one stool per day. This is usually from day 1 to 4. By day 5, passing black or dark green stools is not normal. Your baby should be seen to make sure your baby is getting enough milk.
- Normal Breastmilk Stools without any meconium present are seen from day 5 on. The stools are runny, mustard-colored and can contain seedy particles. Normal breastfed stools can also be green (caused by bile) or have a water-ring around them, especially during the first month. Reason: rapid transit. Normal breastfed stools are loose (often runny and seedy). Stools are yellow, but sometimes can be green. The green color is from bile. Runny stools can even be bordered by a water ring. This is normal.
- Normal stool size is about half to 1 tablespoon (8 to 15 mL).
- Number of Stools: The number of stools is the best marker for how much breastmilk the baby is getting. On day of life 2 and 3, the baby should pass 1 or 2 stools per day. By day of life 4 or 5, the baby should be passing 3 or more breastmilk stools per day. Once breast-feeding is established, babies normally pass 4 stools per day to 1 after each feeding during the first month of life.
- If breastfed babies get any formula, their stools become greener. They also become more frequent, more formed and odorous.
-
Diarrhea. Breastfed stools have changed to true diarrhea if:
- They have blood or mucus
- Smell bad or have a sudden increase in number
- Your baby feeds poorly, acts sick, or a fever occurs
-
Normal Infrequent Breastfed Stools After 1 Month of Age:
- Between 4 and 8 weeks of age, some breastfed babies change to normal infrequent stools.
- They can pass 1 large soft stool every 4 to 7 days.
- Reason: Complete absorption of breastmilk.
- The longer they go without a stool, the larger the volume that is passed.
- There is no pain or crying with stool passage.
-
Leaking Breast Milk:
- Leaking milk is a common problem that nursing mothers experience during the first months. Usually, the leaking lessens as supply starts to equal demand. A balance is established between what the baby drinks and what the breasts make. Here's what you can do:
- Keep a regular nursing pattern. Try to not skip or postpone feedings. Reason: More milk leaks from over-full breast.
- Use nursing pads under your bra. You can use pads that can be thrown away or washable pads. Change pads often to keep your nipples dry.
- Shirts with patterns hide milk spots better.
- If this advice doesn't help, ask a lactation consultant for more tips.
-
Vitamin D for the Baby:
- Breast milk contains all the needed vitamins and minerals except Vitamin D.
- Vitamin D. Starting the first week of life, all breastfed babies need Vitamin D. The dose is 400 IU per day. (AAP Committee on Nutrition 2009). You can use separate Vitamin D drops. Or, you can use Vitamin ADC drops in a dose of 1 mL per day. (No prescription is needed).
- Your child needs Vitamin D drops until he drinks enough cow's milk or formula. This is at least 32 ounces (1000 mL) of milk or formula per day. Each 8 ounces (250 mL) contains 100 IU of Vitamin D.
-
Storage of Breast Milk:
- Freshly expressed breast milk can be kept at room temp for 6 hours.
- Freshly pumped breast milk can be stored for 5 days in a refrigerator.
- Frozen breast milk can be kept 6 months in a refrigerator freezer. Do not store milk in the freezer door (side) shelves. Milk can be kept up to 12 months in a deep freezer. If your ice cream is solidly frozen, the temperature is fine.
- To thaw frozen milk, put the bag of breast milk in the refrigerator. It will take a few hours to thaw.
- For quicker thawing, place it in a pan of warm water. Do this until it has warmed up to the temperature your baby likes. Never warm it up in a microwave or boiling water. This would destroy the protective antibodies.
- After thawing, breast milk can be kept safely in the refrigerator for 24 hours. Do not refreeze.
- After feeding your baby, throw out any remaining milk in the bottle. This milk should be discarded after 1 hour.
-
Burping:
- You do not have to burp your baby. Burping is an option, but not needed.
- It is not harmful if a baby doesn't burp.
- Burping can lessen spitting up, but it doesn't decrease crying.
- Burping can be done twice per feeding, once midway and once at the end.
- If the baby does not burp after 1 minute of patting, it can be stopped.
-
Milk Letdown that Causes Pulling Away, Coughing or Choking:
- Sometimes, a milk surge will be more than your baby can keep up with.
- Your baby's reaction will be to pull away from the breast. She may cry, cough or even choke.
- Stop the feeding and let your baby recover.
- Wait until the letdown spray stops before putting her back to the breast.
- Pausing and burping more often may help.
- Prevention: The overactive letdown often occurs in mothers who pump often. So, finish one side all the way. Then only pump the other side enough to get rid of any pain.
-
Cereals and Other Solids (Baby Foods):
- Breast-fed infants should be started on baby foods at 6 months. First baby foods can be cereals and/or fruit.
- Starting before 6 months is not needed. Starting before 6 months makes feedings messier and longer. Early use of solids can also cause gagging.
- Solids don't increase sleeping through the night for breast-fed infants.
- Caution: Delaying solids past 9 months of age is not advised. The delay runs the risk that your infant will refuse solids.
-
Call Your Doctor If:
- Your baby has trouble latching on
- Your baby does not have a strong suck
- Your baby acts hungry after most feeds
- Your baby is not acting normal
- Breastfeeding is painful
- You think your child needs to be seen
- You have other questions about breastfeeding
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.
Burn
Is this your child's symptom?
- Burns to the skin
- A burn is a heat, chemical or electrical injury to the skin
If NOT, try one of these:
Causes of Burns
- Hot Liquids. Hot liquids (such as coffee) are the most common cause of burns. They cause a scald.
- Hot Surfaces. Examples are ovens, stoves, space heaters and curling irons.
- Chemical Burns (Serious). Examples are acids or lye splashed on the skin. They continue to damage the skin until they are removed.
- Electrical Burns (Serious). They can be much deeper than they first appear.
- Flame Burns (Serious). Flammable liquid burns are mainly seen in teen boys.
- Friction Burns. Treadmill burns are a common example.
- Sunburn is not covered here. See the Sunburn care guide.
Degrees of Burns
- 1st degree. Red skin without blisters. These burns don't need to be seen.
- 2nd degree. Red skin with blisters. Heals from the bottom up, not from the edges. Takes 2 to 3 weeks. Small closed blisters decrease pain and act as a natural bandage.
- 3rd degree. Deep burns with white or charred skin. There are no blisters. Skin feeling is lost. Heals in from the edges. Grafts are often needed if it is larger than a quarter in size. These are burns over 1 inch or 2.5 cm. Skin grafts help limit scarring.
When to Call for Burn
Call 911 Now
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Self Care at Home
|
Call 911 Now
- 2nd or 3rd degree burn covers a large area
- Trouble breathing with burn to the face
- Trouble breathing after being near fire, smoke or fumes
- Hard to wake up
- Acts or talks confused
- You think your child has a life-threatening emergency
Call Doctor or Seek Care Now
- Eye or eyelid burn
- Burn goes all the way around an arm or leg
- Center of the burn is white or charred
- Electrical burn
- Explosion or gun powder caused the burn
- Chemical burn (such as acid)
- Coughing after being near fire and smoke
- House fire burn
- Severe pain and not better 2 hours after taking pain medicine
- Burn looks infected (spreading redness, red streaks, swelling, or tender to the touch)
- You think your child has a serious burn
- You think your child needs to be seen, and the problem is urgent
Call Doctor Within 24 Hours
- Blister is present. Exception: small closed blister less than ½ inch or 12 mm size.
- You think your child needs to be seen, but the problem is not urgent
Call Doctor During Office Hours
- Minor burn and last tetanus shot more than 10 years ago
- Burn not healed after 10 days
- You have other questions or concerns
Self Care at Home
- Minor heat or chemical burn
- Blisters less than ½ inch (12 mm) size
Care Advice for 1st Degree Burns or Small Blisters
-
What You Should Know About Burns :
- Minor burns can be treated at home.
- This includes some small blisters.
- Here is some care advice that should help.
-
Cold Pack for Pain:
- For pain, put a cold wet washcloth on the burn.
- Repeat as needed.
-
Pain Medicine:
- To help with the pain, give an acetaminophen product (such as Tylenol).
- Another choice is an ibuprofen product (such as Advil).
- Use as needed.
-
Clean the Burn:
- Wash the burn gently with warm water.
- Do not use soap unless the burn is dirty. Reason: Soaps can slow healing.
-
Closed Blisters - Don't Open:
- Don't open any small closed blisters.
- The outer skin protects the burn from infection.
-
Antibiotic Ointment for Open Blisters:
- For any broken blisters, use an antibiotic ointment (such as Polysporin). No prescription is needed.
- Then cover it with a bandage (such as Band-Aid). Change the dressing every other day.
- Each time, clean the area. Use warm water and 1 or 2 gentle wipes with a wet washcloth.
-
What to Expect:
- Most often, burns hurt for about 2 days.
- It will peel like a sunburn in about a week.
- First- and second-degree burns don't leave scars.
-
Call Your Doctor If:
- Severe pain lasts over 2 hours after taking pain medicine
- Burn starts to look infected (spreading redness, pus)
- Burn not healed after 10 days
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.

The photo shows a 6 inch (15 cm) wide area of mild redness without blistering on the forearm. This thermal burn was caused by spilled hot water.
First Aid Care Advice:
- Immediately put the burned part in cold tap water or pour cold water over it for 10 minutes or cover with a cold wet washcloth.
- Reason: this lessens the depth of the burn and relieves pain.

- Immediately put the burned part in cold tap water or pour cool water over it for 10 minutes (Reason: lessen the depth of the burn and relieve the pain) .
- For burns on the face, apply a cold wet washcloth.
- Do this immediately (don't take time to remove clothing).
Note: A thermal burn is any burn caused by heat.

- Remove any contaminated clothing.
- Brush any dry chemical off the skin.
- Flush the chemical off the skin with warm water for 10 minutes.
- For large areas, use the shower.

This shows a second degree burn that is caused by heat. The burn area is swollen and bulging with blisters.
First Aid Care Advice:
- Immediately put the burned part in cold tap water or pour cold water over it for 10 minutes. Reason: lessens the depth of the burn and relieves pain.
- Cover with a cold wet washcloth and seek emergency care.
Chest Pain
Is this your child's symptom?
- Pain or discomfort in the chest (front or back)
- The chest includes from the top to the bottom of the rib cage
If NOT, try one of these:
Causes of Chest Pain
- Muscle Overuse. Chest pain can follow hard sports (such as throwing a baseball). Lifting (such as weights) or upper body work (such as digging) can also cause it. This type of muscle soreness often increases with movement of the shoulders.
- Muscle Cramps. Most brief chest pain lasting seconds to minutes is from muscle cramps. The ribs are separated by muscles. These fleeting pains can also be caused by a pinched nerve. These chest wall pains are harmless. Brief muscle cramps are also the most common cause of recurrent chest pains. The medical name is precordial catch syndrome.
- Coughing. Chest pain commonly occurs with a hacking cough. Coughing can cause sore muscles in the chest wall, upper abdomen or diaphragm.
- Asthma. Children with asthma often have a tight chest. They may refer to this as chest pain. They also get chest pain when they have lots of coughing.
- Heartburn. Heartburn is due to reflux of stomach contents. It usually causes a burning pain under the lower sternum (breastbone).
- Caffeine. A rapid and pounding heart beat may be reported as chest pain. Too much caffeine as found in energy drinks is a common cause. Drugs prescribed for ADHD also can cause a fast heartbeat. Illegal drugs, such as cocaine, can cause a high heart rate as well.
- Chest Wall Injury. Blunt trauma usually just causes a bruised rib. Sometimes, it causes a rib fracture.
- Heart Disease (Serious). Heart disease is hardly ever the cause of chest pain in children. Chest pain that only occurs with exercise could have a cardiac cause.
- Pleurisy (Serious). Pleurisy is another problem of pneumonia. If the infection involves the lung's surface, that area of the chest will hurt.
Pain Scale
- Mild: your child feels pain and tells you about it. But, the pain does not keep your child from any normal activities. School, play and sleep are not changed.
- Moderate: the pain keeps your child from doing some normal activities. It may wake him or her up from sleep.
- Severe: the pain is very bad. It keeps your child from doing all normal activities.
When to Call for Chest Pain
Call 911 Now
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Self Care at Home
|
Call 911 Now
- Severe trouble breathing (struggling for each breath, can barely speak or cry)
- Passed out (fainted)
- Bluish lips or face
- Not moving or too weak to stand
- You think your child has a life-threatening emergency
Call Doctor or Seek Care Now
- Your child has heart disease
- Trouble breathing, but not severe
- Taking a deep breath makes the pain worse
- Heart is beating very rapidly
- After a direct blow to the chest
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Call Doctor Within 24 Hours
- Fever is present
- Cause of chest pain is not clear. Exception: pain due to coughing, sore muscles, heartburn or other clear cause.
- You think your child needs to be seen, but the problem is not urgent
Call Doctor During Office Hours
- Chest pains only occur with hard exercise (such as running)
- Sore muscles last more than 7 days
- Heartburn lasts more than 2 days on treatment
- Chest pains are a frequent problem
- You have other questions or concerns
Self Care at Home
- Normal chest pain from sore muscles
- Normal chest pain from heartburn
Care Advice
Sore Muscle Pain Treatment
-
What You Should Know About Mild Chest Pain:
- Chest pains in children lasting for a few minutes are usually harmless. The pain can be caused by muscle cramps. They need no treatment.
- Chest pains that last longer can be from hard work or sports. The shoulders are usually involved. Sore muscles can start soon after the event.
- Here is some care advice that should help.
-
Pain Medicine:
- To help with the pain, give an acetaminophen product (such as Tylenol).
- Another choice is an ibuprofen product (such as Advil).
- Use as needed.
- Continue this until 24 hours have passed without pain.
-
Cold Pack for Pain:
- For the first 2 days, use a cold pack to help with the pain.
- You can also use ice wrapped in a wet cloth.
- Put it on the sore muscles for 20 minutes, then as needed.
- Caution: Avoid frostbite.
-
Use Heat After 48 Hours:
- If pain lasts over 2 days, put heat on the sore muscle.
- Use a heat pack, heating pad or warm wet washcloth.
- Do this for 10 minutes, then as needed.
- Reason: Increase blood flow and improve healing.
- Caution: Avoid burns.
- A hot shower may also help.
-
Stretching the Muscles:
- Gentle stretching of the shoulders and chest wall may help.
- Do sets of 10 twice daily.
- This may prevent muscle cramps from coming back.
- Stretching can be continued even during the chest pain. Do not do any exercises that increase the pain.
-
What to Expect:
- For sore muscles, the pain most often peaks on day 2.
- It can last up to 6 or 7 days.
-
Call Your Doctor If:
- Pain becomes severe
- Pain lasts over 7 days on treatment
- You think your child needs to be seen
- Your child becomes worse
Heartburn (Reflux) Pain Treatment
-
What You Should Know About Heartburn:
- Heartburn is common.
- It's due to stomach acid going up into the esophagus. The esophagus is the tube from the mouth to the stomach.
- Heartburn causes a burning pain behind the lower part of the breastbone. It also causes a sour (acid) taste in the mouth and belching.
- Here is some care advice that should help.
-
Antacids:
- Heartburn is usually easily treated. Give a liquid antacid by mouth (such as Mylanta or the store brand). No prescription is needed.
- Dose: Give 1 to 2 tablespoons (15 - 30 mL).
- If you don't have an antacid, use 2 to 3 ounces (60 - 90 mL) of milk.
- For heartburn that keeps coming back, give an antacid 1 hour before meals. Also, give a dose at bedtime. Do this for a few days.
-
Heartburn Prevention:
- Do not eat too much at meals. This overfills the stomach.
- Do not eat foods that make heartburn worse. Examples are chocolate, fatty foods, spicy foods, carbonated soda, and caffeine.
- Do not bend over during the 3 hours after meals.
- Do not wear tight clothing or belts around the waist.
-
What to Expect:
- Most often, heartburn goes away with treatment.
- But, heartburn also tends to come back. So, preventive measures are important.
-
Call Your Doctor If:
- Heartburn doesn't go away after 2 days of treatment
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.
Chickenpox
Is this your child's symptom?
- A rash all over the body caused by the chickenpox virus.
- The chickenpox rash starts as small red bumps. The bumps change to blisters or pimples. The bumps change to open sores, and finally they scab over.
- A doctor has told you that your child has chickenpox.
- Or your child had close contact with another person who has it (or shingles). The contact should be 10-21 days earlier.
Doesn't look like chickenpox, see
Symptoms of Chickenpox
- Chickenpox starts with some small water blisters or pimples on the head and trunk.
- Chickenpox progress within 24 hours through the next 5 stages:
- Small red bumps
- Thin-walled water blisters
- Cloudy blisters
- Open sores, and finally
- Dry brown crusts.
- Rash is all over the body. Most often, starts on the head and back.
- Repeated crops of new chickenpox keep appearing for 4 to 5 days. Therefore, all 5 stages are present at same time.
- Sores (ulcers) can also occur in the mouth, on eyelids, and on genitals.
- Fever is most often present. The more the rash, the higher the fever.
- Known contact to a child with chickenpox or shingles 10 - 21 days earlier
- Main related problems: skin infections from scratching.
Cause of Chickenpox
- Chickenpox is caused by a virus. It is called Varicella.
- Chickenpox can be prevented by getting this vaccine against this virus.
When to Call for Chickenpox
Call 911 Now
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Self Care at Home
|
Call 911 Now
- Not moving or too weak to stand
- You think your child has a life-threatening emergency
Call Doctor or Seek Care Now
- Bright red skin or red streak
- Very painful swelling or very swollen face
- New red rash in addition to chickenpox rash
- Walking is not steady
- Trouble breathing
- Bleeding into the chickenpox
- Fever over 104° F (40° C)
- Age less than 1 month old
- Vomits 3 or more times
- Eye pain or constant blinking
- Took a steroid medicine within past 2 weeks
- Weak immune system. Examples are: sickle cell disease, HIV, cancer, organ transplant, taking oral steroids.
- Chronic skin disease (such as eczema)
- Chronic lung disease (such as cystic fibrosis)
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Call Doctor Within 24 Hours
- Age less than 1 year old
- Teen 13 years or older has chickenpox
- Been near to person with chickenpox or shingles in last 5 days. Also, healthy person who never had a chickenpox vaccine.
- One lymph node gets larger and more tender
- Fever lasts more than 4 days
- Fever returns after being gone more than 24 hours
- Scab or sore drains yellow pus
- One sore gets much larger in size than the others
- Gets new chickenpox after day 6
- You think your child needs to be seen, but the problem is not urgent
Call Doctor During Office Hours
- You have other questions or concerns
Self Care at Home
- Chickenpox with no other problems
Care Advice for Chickenpox
-
What You Should Know About Chickenpox:
- Chickenpox is caused by the varicella virus.
- It's now uncommon because of the chickenpox vaccine.
- Your job is to keep your child comfortable and to limit the itching.
- Here is some care advice that should help.
-
Cool Baths for Itching:
- For itching, give cool or lukewarm baths for 10 minutes as often as needed.
- Caution: Avoid any chill.
- Can add baking soda 2 ounces (60 mL) per tub.
- Baths don't spread the chickenpox.
- Do not use soaps. Reason: Soaps cause dry skin and make the itch worse.
-
Calamine Lotion for Itching:
- Put calamine lotion on the chickenpox that itch the most.
- You can also use an ice cube on the itchy spots for 10 minutes.
- Don't use any lotion containing Benadryl in it. Reason: It can be absorbed across the skin. This can cause side effects in kids.
-
Allergy Medicine for Itching:
- If itching becomes severe or interferes with sleep, give Benadryl by mouth.
-
Try Not to Scratch:
- Try not to let your child pick and scratch at the sores. This can lead to infected sores.
- Trim fingernails.
- Wash hands often with soap.
-
Fever Medicine:
- Give acetaminophen (such as Tylenol) for fever above 102° F (39° C).
- Never use aspirin. Reason: Risk of Reye syndrome.
- Also, don't use ibuprofen products (such as Advil). Reason: May increase risk of bad strep skin infections.
-
Fluids and Soft Diet:
- The mouth and throat ulcers are painful. Try to get your child to drink adequate fluids.
- Goal: Keep your child well hydrated.
- Cold drinks, milk shakes, popsicles, slushes, and sherbet are good choices.
- Solids. Offer a soft diet. Also, avoid foods that need much chewing. Avoid citrus, salty, or spicy foods. Note: Fluid intake is more important than eating any solids.
- For babies, you may need to stop the bottle. Give fluids by cup, spoon or syringe instead. Reason: The nipple can increase the pain.
-
Liquid Antacid for Mouth Pain (Age 1 Year and Older):
- For mouth pain, use a liquid antacid (such as Mylanta or the store brand). Give 4 times per day as needed. After meals often is a good time.
- Age 1 to 6 years. Put a few drops in the mouth. Can also put it on with a cotton swab.
- Age over 6 years. Use 1 teaspoon (5 mL) as a mouth wash. Keep it on the ulcers as long as possible. Then can spit it out or swallow it.
- Caution: Do not use regular mouth washes, because they sting.
-
Ointment For Pain With Passing Urine:
- For girls with painful genital ulcers, use petroleum jelly (such as Vaseline).
- Put on the sores as needed.
- For males with painful pox on the tip of the penis, this also works.
-
Return to School:
- Your child can go back to school after all the sores have crusted over.
- Most often, this is day 6 or 7 of the rash.
-
What to Expect:
- Expect new chickenpox every day for 4 or 5 days.
- Most children get 400 to 500 chickenpox.
- They get less pox if they've had the vaccine.
-
Prevent the Spread of Chickenpox in the Office:
- If your child needs to be seen, call first to the office.
- Try to bring another adult. Have one adult enter the office first for instructions.
- For nonurgent problems, the doctor may do an exam in the car.
-
Call Your Doctor If:
- Chickenpox look infected (draining pus, scabs become larger)
- Gets any new chickenpox after day 6
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.

The Chickenpox rash can occur on all body surfaces.
The rash is no longer contagious when all of the spots are crusted over and no new spots are appearing. This usually takes 7 days from the first appearance of the rash.
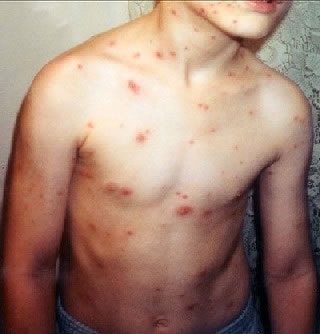
Chickenpox is an infectious disease caused by the varicella-zoster virus resulting in an itchy blister-like rash, tiredness and fever.
It appears first on the trunk and face, but can spread over the entire body causing between 250 and 500 itchy blisters.
Circumcision Problems
Is this your child's symptom?
- Recent circumcision (removal of the male foreskin)
- Mainly circumcision of newborns
Normal Circumcision Healing
- A circumcision is the removal of most of the male foreskin.
- The incision starts off red and tender. The tenderness should be much less by day 3.
- The scab at the incision line comes off in 7 to 10 days.
- If a Plastibell (plastic ring) was used, it should fall off by 14 days. 10 days is the average. While it can't fall off too early, pulling it off can cause bleeding.
Complications of Circumcision
- Wound Infection (Serious). This is the most common complication. It occurs in less than 1 out of 200 circumcised boys. The main finding is spreading redness up the shaft of the penis.
- Bleeding (Serious). Normal bleeding from the incision site should be a few drops. More than that suggests a bleeding problem. Very rare.
- Urine Retention (Serious). Can't pass urine or just dribbles urine. Defined as no urine in 8 hours. Very rare.
When to Call for Circumcision Problems
Call 911 Now
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Self Care at Home
|
Call 911 Now
- Large blood loss and baby is pale or cold
- Not moving or very weak
- You think your child has a life-threatening emergency
Call Doctor or Seek Care Now
- Age less than 1 month old and looks or acts abnormal in any way
- Bleeding is more than a few drops
- Head of penis is dark blue or black
- Severe swelling of penis
- Can't pass urine or can only pass a few drops
- No urine for more than 8 hours
- Crying and your child can't be comforted after trying this advice for more than 2 hours
- Age less than 12 weeks old with fever. Caution: do NOT give your baby any fever medicine before being seen.
- Looks infected (redness is spreading or pimples occur)
- Tiny water blisters occur on skin
- Plastic ring has moved on to shaft of penis
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Call Doctor Within 24 Hours
- Bleeding is a few drops, but happens 3 or more times
- Swelling (without redness) gets larger after day 3
- You think your child needs to be seen, but the problem is not urgent
Call Doctor During Office Hours
- Plastic ring stays on more than 14 days
- Penis looks well-healed but not normal to you. (It looks strange or has an extra tag of skin)
- You have other questions or concerns
Self Care at Home
- Normal circumcision
Care Advice for Circumcisions
-
What You Should Know About Circumcisions:
- The tip (head) of the penis can be red after the foreskin is removed. This is normal.
- The rest of the penis should not be red.
- The penis will be swollen for a few days. There may be some bruises or dried blood on it.
- Most circumcisions heal quickly.
- Infections are rare.
- Here is some care advice that should help.
-
Plastic Ring Type Circ:
- Gently wash the area with warm water twice a day.
- Also, do this if it becomes dirty with poop.
-
Incision (No Plastic Ring is Present) Type Circ:
- The dressing is gauze with petroleum jelly. Take this off 24 hours later. Sometimes, it will fall off on its own. If you need to remove it, use a warm wet washcloth.
- Gently wash the area with warm water twice a day. Also, do this if it becomes dirty with poop.
-
Ointment for Pain:
- Put a layer of ointment on the incision line. This should lessen any pain and crying.
- To prevent pain, use petroleum jelly (such as Vaseline). Put it on the incision line and head of the penis. Do this after each cleansing for the first 4 days. Other option: You can also use an antibiotic ointment (such as Polysporin). No prescription is needed.
- Reason: Helps keep it soft and stops the diaper from sticking during healing.
-
Crying - Don't Give Pain Meds:
- Circumcisions are usually not that painful.
- Covering the wound with an ointment often is all that is needed.
- Do not give pain medicine (such as Tylenol).
- If your baby is crying a lot, he may need to be seen. Call your doctor if you think your baby is in pain.
- Your baby's doctor will decide if pain meds are needed.
-
Bleeding - How to Stop:
- The circumcision wound can normally bleed a few drops. Most often, this is caused by the diaper rubbing on the wound.
- Will stop on its own or with a few minutes of direct pressure.
- Can stop bleeding by keeping the area soft with an ointment.
-
What to Expect For A Plastic Ring:
- The plastic ring will normally fall off between 7 and 14 days (average 10).
- It often hangs by a small piece of tissue for a few days.
- It will come off on its own.
- Pulling it off can cause bleeding.
- It can't fall off too early.
-
Prevent Infections:
- Fasten the diaper loosely to prevent friction against the penis.
- Avoid tub baths for 7 days after the circ. Just clean the penis with a wet cloth.
- If the cord is still on, wait longer. Avoid tub baths until 2 days after cord falls off.
-
Call Your Doctor If:
- Looks infected
- Bleeding occurs
- Plastic ring moves onto shaft of the penis
- Plastic ring does not fall off by day 14
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.
Colds
Is this your child's symptom?
- Runny nose and sore throat caused by a virus
- You think your child has a cold. Reason: Other family members, friends or classmates have same symptoms.
- Also called an Upper Respiratory Infection (URI)
If NOT, try one of these:
Symptoms of a Cold
- Runny or stuffy nose
- The nasal discharge starts clear but changes to grey. It can also be yellow or green.
- Most children have a fever at the start.
- A sore throat can be the first sign
- At times, the child may also have a cough and hoarse voice. Sometimes, watery eyes and swollen lymph nodes in the neck also occur.
Cause of Colds
- Colds are caused by many respiratory viruses. Healthy children get about 6 colds a year.
- Influenza virus causes a bad cold with more fever and muscle aches.
- Colds are not serious. With a cold, about 5 and 10% of children develop another health problem. Most often, this is an ear or sinus infection. These are caused by a bacteria.
Colds: Normal Viral Symptoms
- Colds can cause a runny nose, sore throat, hoarse voice, a cough or croup. They can also cause stuffiness of the nose, sinus or ear. Red watery eyes can also occur. Colds are the most common reason for calls to the doctor. This is because of all the symptoms that occur with colds.
- Cold symptoms are also the number one reason for office and ER visits. Hopefully, this information will save you time and money. It can help you to avoid some needless trips to the doctor. The cold symptoms listed below are normal. These children don't need to be seen:
- Fever up to 3 days (unless it goes above 104° F or 40° C)
- Sore throat up to 5 days (with other cold symptoms)
- Nasal discharge and congestion up to 2 weeks
- Coughs up to 3 weeks
Colds: Symptoms of Secondary Bacterial Infections (other health problems)
Using this guide, you can decide if your child has developed another health problem. This happens in about 5 to 10% of children who have a cold. Many will have an ear infection or sinus infection. Look for these symptoms:
- Earache or ear discharge
- Sinus pain not relieved by nasal washes
- Lots of pus in the eyes (Eyelids stuck together after naps)
- Trouble breathing or rapid breathing (could have pneumonia)
- Fever lasts over 3 days
- Fever that goes away for 24 hours and then returns
- Sore throat lasts over 5 days (may have Strep throat)
- Nasal discharge lasts over 2 weeks
- Cough lasts over 3 weeks
Trouble Breathing: How to Tell
Trouble breathing is a reason to see a doctor right away. Respiratory distress is the medical name for trouble breathing. Here are symptoms to worry about:
- Struggling for each breath or shortness of breath
- Tight breathing so that your child can barely speak or cry
- Ribs are pulling in with each breath (called retractions)
- Breathing has become noisy (such as wheezes)
- Breathing is much faster than normal
- Lips or face turn a blue color
When to Call for Colds
Call 911 Now
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Self Care at Home
|
Call 911 Now
- Severe trouble breathing (struggling for each breath, can barely speak or cry)
- You think your child has a life-threatening emergency
Call Doctor or Seek Care Now
- Not alert when awake ("out of it")
- Trouble breathing not gone after cleaning out the nose
- Wheezing (high-pitched purring or whistling sound when breathing out)
- Breathing is much faster than normal
- Trouble swallowing and new onset drooling
- Ribs are pulling in with each breath (retractions)
- High-risk child (such as cystic fibrosis or other chronic lung disease)
- Weak immune system. Examples are: sickle cell disease, HIV, cancer, organ transplant, taking oral steroids.
- Fever over 104° F (40° C)
- Age less than 12 weeks old with fever. Caution: do NOT give your baby any fever medicine before being seen.
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Call Doctor Within 24 Hours
- Age less than 6 months old
- Earache or ear drainage
- Yellow or green eye discharge
- Sinus pain around cheekbone or eyes (not just congestion)
- Fever lasts more than 3 days
- Fever returns after being gone more than 24 hours
- You think your child needs to be seen, but the problem is not urgent
Call Doctor During Office Hours
- Blocked nose wakes up from sleep
- Yellow scabs around the nasal openings. (Use an antibiotic ointment)
- Sore throat lasts more than 5 days
- Sinus congestion (fullness) lasts more than 14 days
- Nasal discharge lasts more than 2 weeks
- You have other questions or concerns
Self Care at Home
- Mild cold with noother problems
Care Advice for Colds
-
What You Should Know About Colds:
- It's normal for healthy children to get at least 6 colds a year. This is because there are so many viruses that cause colds. With each new cold, your child's body builds up immunity to that virus.
- Most parents know when their child has a cold. Sometimes, they have it too or other children in school have it. Most often, you don't need to call or see your child's doctor. You do need to call your child's doctor if your child develops a complication. Examples are an earache or if the symptoms last too long.
- The normal cold lasts about 2 weeks. There are no drugs to make it go away sooner.
- But, there are good ways to help many of the symptoms. With most colds, the starting symptom is a runny nose. This is followed in 3 or 4 days by a stuffy nose. The treatment for each symptom is different.
- Here is some care advice that should help.
-
For a Runny Nose with Lots of Discharge: Blow or Suction the Nose
- The nasal mucus and discharge is washing germs out of the nose and sinuses.
- Blowing the nose is all that's needed. Teach your child how to blow the nose at age 2 or 3.
- For younger children, gently suction the nose with a suction bulb.
- Put petroleum jelly on the skin under the nose. Wash the skin first with warm water. This will help to protect the nostrils from any redness.
-
Nasal Saline to Open a Blocked Nose:
- Use saline (salt water) nose spray to loosen up the dried mucus. If you don't have saline, you can use a few drops of water. Use distilled water, bottled water or boiled tap water.
- Step 1. Put 3 drops in each nostril. If under 1 year old, use 1 drop.
- Step 2. Blow (or suction) each nostril out while closing off the other nostril. Then, do the other side.
- Step 3. Repeat nose drops and blowing (or suctioning) until the discharge is clear.
- How Often. Do nasal saline rinses when your child can't breathe through the nose.
- Limit. If under 1 year old, no more than 4 times per day or before every feeding.
- Saline nose drops or spray can be bought in any drugstore. No prescription is needed.
- Saline nose drops can also be made at home. Use ½ teaspoon (2 mL) of table salt. Stir the salt into 1 cup (8 ounces or 240 mL) of warm water. Use bottled water or boiled water to make saline nose drops.
- Reason for nose drops: Suction or blowing alone can't remove dried or sticky mucus. Also, babies can't nurse or drink from a bottle unless the nose is open.
- Other option: use a warm shower to loosen mucus. Breathe in the moist air, then blow each nostril.
- For young children, can also use a wet cotton swab to remove sticky mucus.
-
Fluids - Offer More:
- Try to get your child to drink lots of fluids.
- Goal: Keep your child well hydrated.
- It also will thin out the mucus discharge from the nose.
- It also loosens up any phlegm in the lungs. Then it's easier to cough up.
-
Humidifier:
- If the air in your home is dry, use a humidifier.
- Reason: Dry air makes nasal mucus thicker.
-
Medicines for Colds:
- Cold Medicines. Don't give any drugstore cold or cough medicines to young children. They are not approved by the FDA under 6 years. Reasons: not safe and can cause serious side effects. Also, they are not helpful. They can't remove dried mucus from the nose. Nasal saline works best.
- Allergy Medicines. They are not helpful, unless your child also has nasal allergies. They can also help an allergic cough.
- No Antibiotics. Antibiotics are not helpful for colds. Antibiotics may be used if your child gets an ear or sinus infection.
-
Other Symptoms of Colds - Treatment:
- Pain or Fever. Use acetaminophen (such as Tylenol) to treat muscle aches, sore throat or headaches. Another choice is an ibuprofen product (such as Advil). You can also use these medicines for fever above 102° F (39° C).
- Sore Throat. If over 6 years of age, your child can also suck on hard candy. For children over 1 year old, sip warm chicken broth. Some children prefer cold foods, such as popsicles or ice cream.
- Cough. For children over 1 year old, give honey ½ to 1 teaspoon (2 to 5 mL). Caution: Do not use honey until 1 year old. If over 6 years of age, you can also use cough drops. Avoid cough drops before 6 years. Reason: risk of choking.
- Red Eyes. Rinse eyelids often with wet cotton balls.
-
Return to School:
- Your child can go back to school after the fever is gone. Your child should also feel well enough to join in normal activities.
- For practical purposes, the spread of colds can't be prevented.
-
What to Expect:
- Fever can last 2-3 days
- Nasal drainage can last 7-14 days
- Cough can last 2-3 weeks
-
Call Your Doctor If:
- Trouble breathing occurs
- Earache occurs
- Fever lasts more than 3 days or goes above 104° F (40° C)
- Any fever if under 12 weeks old
- Nasal discharge lasts more than 14 days
- Cough lasts more than 3 weeks
- You think your child needs to be seen
- Your child becomes worse
-
Extra Advice - Air Travel with Colds:
- It's safe to fly when your child has a cold.
- He could get some mild ear congestion or even a brief earache while flying. Most often, that can be prevented. (See # 12).
- Flying will not cause an ear infection.
-
Extra Advice - Prevent Ear Congestion During Air Travel:
- Most symptoms happen when the airplane is coming down in altitude. This is the descent of the plane during the 15 minutes before landing.
- Keep your child awake during takeoff and descent.
- Swallow during descent using fluids or a pacifier.
- Children over age 4 can chew gum during descent.
- Yawning during descent also can open the middle ear.
- Drink lots of fluids throughout the flight. This will prevent the nasal secretions from drying out.
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.
Constipation
Is this your child's symptom?
- Can't pass a stool or pain when passing a stool
- Crying when passing a stool (bowel movement or BM) or
- Can't pass a stool after straining or pushing longer than 10 minutes or
- 3 or more days without passing a stool (Exception: Breastfed and over 1 month old)
- Caution: any belly pain from constipation comes and goes. Most often, it is mild. Use the Abdominal Pain (Stomach Pain) care guide if there is constant belly pain.
If NOT, try one of these:
Causes of Constipation
- High Milk Diet. Milk and cheese are the only foods that in high amounts can cause constipation. It causes hard pale stools. This is why you want your child to eat a well-balanced diet.
- Low Fiber Diet. Fiber is found in vegetables, fruits and whole grains. Fiber keeps stools soft, bulky and easy to pass. A low fiber diet causes hard, small stools.
- Low Fluid Intake. This can also cause stools to be dry and harder to pass. It's rarely the only cause of constipation.
- Lack of Exercise. Exercise also keeps the bowel from slowing down. Not a cause in children unless they are confined to bed.
- Holding Back Stools Because of Pain. If passing a stool causes pain, many children will hold back the next one. This can happen with a Strep infection around the anus. It can also occur with a bad diaper rash or anal fissure (tear).
- Holding Back Stools Because of Power Struggles. This is the most common cause of recurrent constipation in children. Most often it's a battle around toilet training. If they are already trained, it may begin with the start of school. Reason: some children refuse to use public toilets. Some children postpone stools because they are too busy to sit down.
- Slow passage of food through the intestines. Most often, this type runs in families. Called slow transit time.
Stools: How Often is Normal?
- Normal Range: 3 per day to 1 every 2 days. Once children are on normal table foods, their stool pattern is like adults.
- Kids who go every 4 or 5 days almost always have pain with passage. They also have a lot of straining.
- Kids who go every 3 days often drift into longer times. Then, they also develop symptoms.
- Passing a stool should be free of pain.
- Any child with pain during stool passage or lots of straining needs treatment. At the very least, the child should be treated with changes in diet.
Imitators of Constipation: Normal Patterns and Stools
- Breastfed and Over 1 Month Old. Stools every 4-7 days that are soft, large and pain-free can be normal. Caution: before 1 month old, not stooling enough can mean not getting enough breast milk.
- Straining in Babies. Grunting or straining while pushing out a stool is normal in young babies. It's hard to pass stool lying on your back with no help from gravity. Babies also become red in the face during straining. This is normal.
- Brief straining under 10 minutes can occur at times at any age.
- Large Stools. Size relates to the amount of food eaten. Large eaters have larger stools.
- Hard or Dry Stools. Also can be normal if passed easily without too much straining. Often, this relates to poor fiber intake. Some children even have small, dry rabbit-pellet-like stools.
When to Call for Constipation
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Self Care at Home
|
Call Doctor or Seek Care Now
- Stomach pain goes on more than 1 hour (includes crying) after using care advice
- Rectal pain goes on more than 1 hour (includes straining) after using care advice
- Vomits 2 or more times and stomach looks more swollen than normal
- Age less than 1 month old and breastfed
- Age less than 12 months with recent onset of weak suck or weak muscles
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Call Doctor Within 24 Hours
- Age less than 2 months. Exception: normal straining and grunting.
- Bleeding from anus
- Needs to pass a stool but afraid to or refuses to let it out
- Child may be "blocked up"
- Suppository or enema was given but did not work
- You think your child needs to be seen, but the problem is not urgent
Call Doctor During Office Hours
- Leaking stool
- Suppository or enema was needed to get the stool out
- Infrequent stools do not get better after changes to diet. Exception: normal if breastfed infant more than 1 month old and stools are not painful.
- Stool softeners are being used and have not been discussed with your doctor
- Toilet training is in progress
- Painful stools occur 3 or more times after changes to diet
- Constipation is a frequent problem
- You have other questions or concerns
Self Care at Home
- Mild constipation
Care Advice for Constipation
-
What You Should Know about Constipation:
- Constipation is common in children.
- Most often, it's from a change in diet. It can also be caused by waiting too long to stool.
- Passing a stool should be pleasant and free of pain.
- Any child with pain during stool passage or lots of straining needs treatment. At the very least, they need changes in diet.
- Here is some care advice that should help.
-
Normal Stools:
- Normal range: 3 per day to 1 every 2 days. Once children are on a regular diet, their stool pattern is like adults.
- Kids who go every 3 days often drift into longer times. Then symptoms start.
- Kids who go every 4 and 5 days almost always have pain with passage. They also have lots of straining.
-
Diet for Infants Under 1 Year Old:
- Age over 1 month old only on breast milk or formula, add fruit juice.
- Amount. Give 1 ounce (30 mL) per month of age per day. Limit amount to 4 ounces (120 mL).
- Pear and apple juice are good choices. After 3 months, can use prune (plum) juice. Reason for fruit juice: approved for babies in treating a symptom.
- Age over 4 months old, also add baby foods with high fiber. Do this twice a day. Examples are peas, beans, apricots, prunes, peaches, pears, or plums.
- Age over 8 months old on finger foods, add cereals and small pieces of fresh fruit.
-
Diet for Children Over 1 Year Old:
- Increase fruit juice (apple, pear, cherry, grape, prune). Note: Citrus fruit juices are not helpful.
- Add fruits and vegetables high in fiber content. Examples are peas, beans, broccoli, bananas, apricots, peaches, pears, figs, prunes, or dates. Offer these foods 3 or more times per day.
- Increase whole grain foods. Examples are bran flakes or muffins, graham crackers, and oatmeal. Brown rice and whole wheat bread are also helpful. Popcorn can be used if over 4 years old.
- Limit milk products (milk, ice cream, cheese, yogurt) to 3 servings per day.
- Fluids. Give enough fluids to stay well-hydrated. Reason: keep the stool soft.
-
Stop Toilet Training:
- Put your child back in diapers or pull-ups for a short time.
- Tell him that the poops won't hurt when they come out.
- Praise him for passing poops into a diaper.
- Holding back stools is harmful. Use rewards to help your child give up this bad habit.
- Avoid any pressure or punishment. Also, never force your child to sit on the potty against his will. Reason: It will cause a power struggle.
- Treats and hugs always work better.
-
Encourage Sitting on the Toilet (if toilet trained):
- Set up a normal stool routine, if your child agrees to sitting.
- Have your child sit on the toilet for 5 minutes after meals.
- This is especially important after breakfast.
- If you see your child holding back a stool, also take to the toilet for a sit (if cooperates).
- During sits, stay with your child and be a coach. Just focus on helping the poop come out.
- Do not distract your child. Do not allow your child to play with video devices, games or books during sits.
- Once he passes a normal size stool, he doesn't need to sit anymore that day.
-
Warm Water to Relax the Anus:
- Warmth helps many children relax the anus and release a stool.
- For straining too long, have your child sit in warm water.
- You can also put a warm wet cotton ball on the anus. Vibrate it side to side for about 10 seconds to help relax the anus.
-
Flexed Position to Help Stool Release:
- Help your baby by holding the knees against the chest. This is like squatting for your baby. This is the natural position for pushing out a stool. It's hard to have a stool lying down.
- Gently pumping the left side of the belly also helps.
-
Stool Softeners (Age Over 1 Year Old):
- If a change in diet doesn't help, you can add a stool softener. Must be over 1 year of age.
- Use a stool softener (such as Miralax). It is available without a prescription. Give 1-3 teaspoons (5-15 mL) powder each day with dinner. Mix the powder in 2 to 6 ounces (60-180 mL) of water.
- Fiber products (such as Benefiber) are also helpful. Give 1 teaspoon (5 mL) twice a day. Mix it in 2 ounces (60 mL) of water or fruit juice.
- Stool softeners and fiber work 8-12 hours after they are given.
- Safe to continue as long as needed.
-
What to Expect:
- Most often, changes in diet helps constipation.
- After your child is better, be sure to keep him on high fiber foods.
- Also, have your child sit on the toilet at the same time each day.
- These tips will help to prevent the symptoms from coming back.
-
Call Your Doctor If:
- Constipation lasts more than 1 week after making changes to diet
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.
Cough
Is this your child's symptom?
- The sound made when the cough reflex clears the airway of irritants
- Most coughs are part of a cold
- A coughing fit or spell is over 5 minutes of nonstop coughing
- Coughs can be dry (no mucus) or wet (with white, yellow or green mucus)
If NOT, try one of these:
Causes of Cough
- Common Cold. Most coughs are part of a cold that includes the lower airway. The medical name is viral bronchitis. The bronchi are the lower part of the airway that go to the lungs. Bronchitis in children is always caused by a virus. This includes cold viruses, influenza and croup. Bacteria do not cause bronchitis in healthy children.
- Sinus Infection. The exact mechanism of the cough is unknown. It may be that post-nasal drip irritates the lower throat. Or pressure within the sinus may trigger the cough reflex.
- Allergic Cough. Some children get a cough from breathing in an allergic substance. Examples are pollens or cats. Allergic coughs can be controlled with allergy medicines, such as Benadryl.
- Asthma. Asthma with wheezing is the most common cause of chronic coughs in children. In adults, it's smoking.
- Cough Variant Asthma. 25% of children with asthma only cough and never wheeze. The coughing spells have the same triggers as asthma attacks.
- Air Pollution Cough. Fumes of any kind can irritate the airway and cause a cough. Tobacco smoke is the most common example. Others are auto exhaust, smog and paint fumes.
- Exercise Induced Cough. Running will make most coughs worse. If the air is cold or polluted, coughing is even more likely.
- Serious Causes. Pneumonia, bronchiolitis, whooping cough and airway foreign object
Trouble Breathing: How to Tell
Trouble breathing is a reason to see a doctor right away. Respiratory distress is the medical name for trouble breathing. Here are symptoms to worry about:
- Struggling for each breath or shortness of breath
- Tight breathing so that your child can barely speak or cry
- Ribs are pulling in with each breath (called retractions)
- Breathing has become noisy (such as wheezes)
- Breathing is much faster than normal
- Lips or face turn a blue color
Phlegm or Sputum: What's Normal?
- Yellow or green phlegm is a normal part of the healing of viral bronchitis.
- This means the lining of the trachea (windpipe) was damaged by the virus. It's part of the phlegm your child coughs up.
- Bacteria do not cause bronchitis in healthy children. Antibiotics are not helpful for the yellow or green phlegm seen with colds.
- The main treatment of a cough with phlegm is to drink lots of fluids. Also, if the air is dry, using a humidifier will help. Sipping warm clear fluids will also help coughing fits.
When to Call for Cough
Call 911 Now
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Self Care at Home
|
Call 911 Now
- Severe trouble breathing (struggling for each breath, can barely speak or cry)
- Passed out or stopped breathing
- Lips or face are bluish when not coughing
- You think your child has a life-threatening emergency
Call Doctor or Seek Care Now
- Trouble breathing. Exception: present only when coughing.
- Lips or face have turned bluish during coughing
- Ribs are pulling in with each breath (retractions)
- Harsh sound with breathing in (called stridor)
- Wheezing (high-pitched purring or whistling sound when breathing out)
- Breathing is much faster than normal
- Can't take a deep breath because of chest pain
- Severe chest pain
- Coughed up blood
- Not alert when awake ("out of it")
- Weak immune system. Examples are: sickle cell disease, HIV, cancer, organ transplant, taking oral steroids.
- High-risk child (such as cystic fibrosis or other chronic lung disease)
- Age less than 12 weeks old with fever. Caution: do NOT give your baby any fever medicine before being seen.
- Fever over 104° F (40° C)
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Call Doctor Within 24 Hours
- Nonstop coughing spells
- Age less than 6 months old
- Earache or ear drainage
- Sinus pain (not just congestion) around cheekbone or eyes
- Fever lasts more than 3 days
- Fever returns after being gone more than 24 hours
- Chest pain even when not coughing
- You think your child needs to be seen, but the problem is not urgent
Call Doctor During Office Hours
- Coughing causes vomiting 3 or more times
- Coughing has kept home from school for 3 or more days
- Allergy symptoms (such as runny nose and itchy eyes) also present
- Runny nose lasts more than 14 days
- Cough lasts more than 3 weeks
- You have other questions or concerns
Self Care at Home
- Cough with no other problems
Care Advice for Cough
-
What You Should Know About Coughs:
- Most coughs are a normal part of a cold.
- Coughing up mucus is very important. It helps protect the lungs from pneumonia.
- A cough can be a good thing. We don't want to fully turn off your child's ability to cough.
- Here is some care advice that should help.
-
Homemade Cough Medicine:
- Goal: Decrease the irritation or tickle in the throat that causes a dry cough.
- Age 3 months to 1 year: Give warm clear fluids to treat the cough. Examples are apple juice and lemonade. Amount: Use a dose of 1-3 teaspoons (5-15 mL). Give 4 times per day when coughing. Caution: Do not use honey until 1 year old.
- Age 1 year and older: Use Honey ½ to 1 teaspoon (2-5 mL) as needed. It works as a homemade cough medicine. It can thin the secretions and loosen the cough. If you don't have any honey, you can use corn syrup.
- Age 6 years and older: Use Cough Drops to decrease the tickle in the throat. If you don't have any, you can use hard candy. Avoid cough drops before 6 years. Reason: risk of choking.
-
Non-Prescription Cough Medicine (DM):
- Non-prescription cough medicines are not advised. Reason: No proven benefit for children and not approved under 6 years old. (FDA)
- Honey has been shown to work better for coughs. Caution: Do not use honey until 1 year old.
- If age 6 years or older, you might decide to use a cough medicine. Choose one with dextromethorphan (DM), such as Robitussin Cough syrup. DM is present in most non-prescription cough syrups.
- When to Use: Give only for severe coughs that interfere with sleep or school.
- DM Dose: Give every 6 to 8 hours as needed.
-
Coughing Fits or Spells - Warm Mist and Fluids:
- Breathe warm mist, such as with shower running in a closed bathroom.
- Give warm clear fluids to drink. Examples are apple juice and lemonade.
- Age under 3 months. Don't use warm fluids.
- Age 3 - 12 months of age. Give 1 ounce (30 mL) each time. Limit to 4 times per day.
- Age over 1 year of age. Give as much as needed.
- Reason: Both relax the airway and loosen up any phlegm.
-
Vomiting from Hard Coughing:
- For vomiting that occurs with hard coughing, give smaller amounts per feeding.
- Also, feed more often.
- Reason: Vomiting from coughing is more common with a full stomach.
-
Encourage Fluids:
- Try to get your child to drink lots of fluids.
- Goal: Keep your child well hydrated.
- It also loosens up any phlegm in the lungs. Then it's easier to cough up.
- It also will thin out the mucus discharge from the nose.
-
Humidifier:
- If the air in your home is dry, use a humidifier. Reason: Dry air makes coughs worse.
-
Fever Medicine:
- For fevers above 102° F (39° C), give an acetaminophen product (such as Tylenol).
- Another choice is an ibuprofen product (such as Advil).
- Note: Fevers less than 102° F (39° C) are important for fighting infections.
- For all fevers: Keep your child well hydrated. Give lots of cold fluids.
-
Avoid Tobacco Smoke:
- Tobacco smoke makes coughs much worse.
-
Return to School:
- Your child can go back to school after the fever is gone.
- Your child should also feel well enough to join in normal activities.
- For practical purposes, the spread of coughs and colds cannot be prevented.
-
Extra Advice- Allergy Medicine for Allergic Cough:
- Allergy medicine can bring an allergic cough under control within 1 hour. The same is true for nasal allergy symptoms.
- A short-acting allergy medicine (such as Benadryl) is helpful. No prescription is needed.
- Give every 6 to 8 hours until the cough is gone.
-
What to Expect:
- Viral bronchitis causes a cough for 2 to 3 weeks.
- Sometimes, your child will cough up lots of phlegm (mucus). The mucus can normally be grey, yellow or green.
- Antibiotics are not helpful.
-
Call Your Doctor If:
- Trouble breathing occurs
- Wheezing occurs
- Cough lasts more than 3 weeks
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.
Coughs: Meds or Home Remedies?
Medicines (OTC)
Over-the-Counter (OTC) cough and cold medicines can cause side effects. These side effects can be serious in young children. The risks of using these medicines outweigh any benefits. In 2008, the Food and Drug Administration (FDA) looked at this issue in children. They recommended these medicines never be used in young children. After age 6, the medicines are safe to use, if you follow the package instructions. But, it's easy to treat coughs and colds without these medicines.
Home Remedies:
A good home remedy is safe, cheap, and as helpful as OTC medicines. They are also found in nearly every home. Here are some simple but helpful home treatments.
1. Runny Nose: Just suction it or blow it. Teach your child how to blow the nose at age 2 or 3. When your child's nose runs like a faucet, it's getting rid of viruses. Allergy medicines (such as Benadryl) do not help the average cold. They are useful only if your child has nasal allergies (hay fever).
2. Blocked Nose: Use nasal saline.
- Use saline (salt water) nose drops or spray to loosen up the dried mucus. If you don't have saline, you can use a few drops of water. Use distilled water, bottled water or boiled tap water.
- Step 1: Put 3 drops in each nostril. If age under 1 year old, use 1 drop.
- Step 2: Blow (or suction) each nostril separately, while closing off the other nostril. Then do other side.
- Step 3: Repeat nose drops and blowing (or suctioning) until the discharge is clear.
- How Often: Do nasal saline rinses when your child can't breathe through the nose. Limit: If under 1 year old, no more than 4 times per day or before every feeding.
- Saline nose drops or spray can be bought in any drugstore. No prescription is needed.
- Saline nose drops can also be made at home. Use ½ teaspoon (2 ml) of table salt. Stir the salt into 1 cup (8 ounces or 240 ml) of warm water. Use bottled water or boiled water to make saline nose drops.
- Reason for nose drops: Suction or blowing alone can't remove dried or sticky mucus. Also, babies can't nurse or drink from a bottle unless the nose is open.
- Other option: use a warm shower to loosen mucus. Breathe in the moist air, then blow (or suction) each nostril.
- For young children, can also use a wet cotton swab to remove sticky mucus.
- Medicines. There are no drugs that can remove dried mucus from the nose.
3. Coughing: Use homemade cough medicines.
- Age 3 months to 1 year. Give warm clear fluids (such as apple juice or lemonade). Dose: 1-3 teaspoons (5-15 ml) four times per day when coughing. Under 3 months, see your child's doctor. Caution: Do not use honey until 1 year old.
- Age 1 year and older. Use Honey ½ to 1 teaspoon (2 to 5 ml) as needed. It thins the secretions and loosens the cough. If you don't have honey, you can use corn syrup. Research shows that honey works better than cough syrups to reduce nighttime coughing.
- Age 6 years and older. Use Cough Drops to decrease the tickle in the throat. If you don't have any, you can use hard candy. Avoid cough drops before 6 years. Reason: risk of choking.
- Coughing fits. The warm mist from a shower can help.
4. Fluids: Help your child drink lots of fluids. Staying well hydrated thins the body's secretions. That makes it easier to cough and blow the nose.
5. Humidity: If the air in your home is dry, use a humidifier. Moist air keeps the nose and airway from drying out. Run a warm shower for a while to help put moisture in the air.
Treatment is Not Always Needed:
- If symptoms aren't bothering your child, they don't need medicine or any treatment. Many children with a cough or cold are happy, play fine and sleep well.
- Only treat symptoms if they cause discomfort or wake your child up. Treat a cough if it's hacking and really bothers your child.
- Fevers are helpful. Only treat them if they slow your child down or cause some discomfort. That does not occur until 102° F (39° C) or higher. Acetaminophen (Tylenol) or ibuprofen (Motrin or Advil) can be given. Use to treat higher fever or pain. See Dose tables.
Summary
If coughs or colds need treatment, home remedies may work better than medicines.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.
Cracked or Dry Skin
Is this your child's symptom?
- Cracked skin or dry, rough skin
- Cracked skin on hands, feet and lips
- Dry, rough skin of entire body surface
If NOT, try one of these:
Causes of Cracks in the Skin
- Most cracked skin is found on the feet, hands or lips.
- Feet. The soles of the feet are most commonly involved. Most often, cracks occur on the heels and big toes. This is called tennis shoe dermatitis. Deep cracks are very painful and can bleed. The main cause is wearing wet or sweaty socks or swimming a lot.
- Hands. Cracks can develop on the hands in children. The main cause is washing the hands too much or washing dishes. Can also occur from working outside in winter weather. The worse cracks of the fingers occur with thumb sucking.
- Lips. The lips can become chapped in children from the sun or wind. If the lips become cracked, it's usually from a "lip-licking" habit. The skin around the lips can also become pink and dry. This occurs especially in children who suck on their lips.
Causes of Dry Skin
- Dry skin is a common condition.
- Soap. Dry skin is mainly caused by too much bathing and soap (soap dermatitis). Soap removes the skin's natural protective oils. Once they are gone, the skin can't hold moisture.
- Climate. Dry climates make dry skin worse, as does winter weather (called winter itch).
- Genetics also plays a role in dry skin.
- Dry skin is less common in teenagers than younger children. This is because the oil glands are more active.
- Keratosis Pilaris - dry, rough, bumpy skin on the back of the upper arms. It's made worse by soaps. Treat with moisturizing creams.
- Pityriasis Alba - dry pale spots on the face. These are more prevalent in the winter time and are also made worse by soaps. Treat with moisturizing creams.
- Eczema. Children with eczema have very dry itchy skin.
Liquid Skin Bandage For Deep, Chronic Cracks
- Liquid plastic skin bandage is a new product that seals wounds. It is a plastic coating that lasts up to 1 week.
- It is the best way to relieve pain and promote healing. As the crack heals from the bottom upward, it pushes the plastic seal up.
- After the wound is washed and dried, put the liquid on. It comes with a small brush or with a swab. It dries in less than a minute. Then apply a second coat. It's waterproof and may last a week.
- You can buy this at any drug store. Many brands of liquid bandage are available. No prescription is needed.
When to Call for Cracked or Dry Skin
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Self Care at Home
|
Call Doctor or Seek Care Now
- Fever and looks infected (spreading redness)
- Cracked red lips and fever lasts 5 days or more
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Call Doctor Within 24 Hours
- Looks infected (pus or spreading redness)
- Bleeding from cracked lips
- Cracks on feet that make it hard to walk
- You think your child needs to be seen, but the problem is not urgent
Call Doctor During Office Hours
- Cracks from thumb-sucking or finger-sucking
- Peeling skin and cause is not clear
- After 2 weeks of treatment, cracked lips are not healed
- After 2 weeks of treatment, cracked skin is not healed
- After 2 weeks of treatment, dry skin is still itchy
- You have other questions or concerns
Self Care at Home
- Cracked skin on the feet
- Cracked skin on the hands
- Chapped lips
- Dry, itchy skin caused by soap or cold/dry weather
Care Advice
Treatment for Cracked Skin on the Feet
-
What You Should Know About Cracks on Feet:
- Most often, cracked skin of the feet is caused by repeated contact with moisture.
- The main cause is often wearing wet (or sweaty) socks. Swimmers also have this problem.
- The soles of the feet are most often involved. Usually, you see cracks on the heels and big toes.
- This is called tennis shoe or sneaker dermatitis.
- Cracked, dry feet usually can be treated at home.
- Here is some care advice that should help.
-
Shallow Cracks - Use Ointment:
- Cracks heal faster if protected from air exposure and drying.
- Keep the cracks constantly covered with petroleum jelly (such as Vaseline). Put it on the cracks 3 times a day.
- If the crack seems mildly infected, use an antibiotic ointment instead (such as Polysporin). No prescription is needed. Put it on the cracks 3 times a day.
- Covering the ointment with a bandage (such as Band-Aid) speeds recovery. You can also cover it with a sock.
- Option: If you have it, a liquid skin bandage works even better. Don't use liquid bandage and ointment together.
-
Deep Cracks - Use Liquid Skin Bandage:
- Deep cracks of the feet or toes usually do not heal with ointments.
- Use a liquid skin bandage that will completely seal the crack. Many brands of liquid bandage are available. No prescription is needed.
- Start with 2 layers. Put on another layer as often as needed.
- As the crack heals, the plastic layer will be pushed up.
-
Prevention of Cracks on Feet:
- Change socks whenever they are wet or sweaty.
- Take an extra pair of socks to school.
- When practical, do not wear shoes. Go barefoot or wear socks only.
- Do not use bubble bath or other soaps in the bath water. Soaps take the natural oils out of the skin.
- Use a moisturizing cream on the feet after baths or showers.
- Wear shoes that allow the skin to "breathe."
-
What to Expect:
- Most cracks heal over in 1 week with treatment.
- Deep cracks heal if you keep them covered all the time with crack sealer. Deep cracks will heal in about 2 weeks with crack sealer.
-
Call Your Doctor If:
- Starts to look infected (redness, red streak, pus)
- Cracks last more than 2 weeks on treatment
- You think your child needs to be seen
- Your child becomes worse
Treatment for Cracked Skin on the Hands
-
What You Should Know About Cracks on Hands:
- Cracked skin of the hands is usually caused by repeated contact with moisture.
- Examples are washing dishes or washing the hands often.
- Soap removes the natural protective oils from the skin.
- Cracked, dry hands usually can be treated at home.
- Here is some care advice that should help.
-
Shallow Cracks - Use Ointment:
- Cracks heal faster if protected from air exposure and drying.
- Keep the cracks constantly covered with petroleum jelly (such as Vaseline). Put it on the cracks 3 times a day.
- If the crack seems mildly infected, use an antibiotic ointment instead (such as Polysporin). No prescription is needed. Put it on the cracks 3 times a day.
- Covering the ointment with a bandage (such as Band-Aid) speeds recovery. You can also cover it with a glove.
- Option: If you have it, a liquid skin bandage works even better. Don't use liquid bandage and ointment together.
-
Deep Cracks - Use Liquid Skin Bandage:
- Deep cracks of the fingers usually do not heal with ointments.
- Use a liquid skin bandage that will completely seal the crack. Many brands of liquid bandage are available. No prescription is needed.
- Start with 2 layers. Put on another layer as often as needed.
- As the crack heals, the plastic layer will be pushed up.
-
Prevention of Cracks on Hands:
- Wash the hands with warm water.
- Use soap only if the hands are very dirty. Also, use soap for anything that won't come off with water.
- Wear gloves when washing dishes.
- During cold weather, wear gloves outside.
- Use a moisturizing cream on the hands after anytime they have been in water.
-
What to Expect:
- Most cracks heal over in 1 week with treatment.
- Deep cracks heal if you keep them covered all the time with crack sealer. Deep cracks will heal in about 2 weeks with crack sealer.
-
Call Your Doctor If:
- Starts to look infected (redness, red streak, pus)
- Cracks last more than 2 weeks on treatment
- You think your child needs to be seen
- Your child becomes worse
Treatment for Chapped Lips
-
What You Should Know About Chapped Lips:
- The lips can become chapped in children from too much sun or wind.
- If the lips become cracked, it's usually from a "lip-licking" habit.
- The skin around the lips can also become pink and dry. This occurs especially when children suck on their lips.
- Here is some care advice that should help.
-
Lip Balm:
- A lip balm should be used often, even hourly.
- Be sure to put it on after eating or drinking.
-
Avoid "Lip-Licking":
- Help your child give up the habit of lip-licking or sucking.
- This habit usually is not seen before age 6.
- This habit will only change if you can gain your child's active participation.
- Appeal to your child's pride. Show your child in a mirror how lip-sucking has affected their appearance.
- Give them a lip lubricant to put on their lips. Tell them to use it when they feel the urge to suck on them. Another option is to replace lip-sucking with chewing gum.
- Offer an incentive for going an entire day without lip-sucking. Examples of rewards are money or points towards a prize.
- Avoid any pressure or punishment. It will backfire, cause a power struggle and make the habit last longer.
-
Call Your Doctor If:
- Starts to look infected (redness, red streak, pus)
- Cracks last more than 2 weeks on treatment
- You think your child needs to be seen
- Your child becomes worse
Treatment for Dry or Itchy Skin
-
What You Should Know About Dry Skin:
- Dry skin is a common condition.
- Mainly caused by too much bathing and soap (soap dermatitis).
- Soap removes the skin's natural protective oils. Once they are gone, the skin can't hold moisture.
- Dry climates make it worse, as does winter weather (called winter itch).
- Genetics also plays a role in dry skin.
- Dry skin is less common in teenagers than younger children. This is because the oil glands are more active in teens.
- Here is some care advice that should help.
-
Bathing - Avoid Soap:
- Young children with dry skin should avoid all soaps. Soaps take the natural protective oils out of the skin. Bubble bath does the most damage.
- For young children, the skin can be cleansed with warm water alone. Keep bathing to 10 minutes or less.
- Most young children only need to bathe twice a week.
- Teenagers can get by with using soap only for the armpits, genitals, and feet. Also, use a mild soap (such as Dove).
- Do not use any soap on itchy areas or rashes.
-
Moisturizing Cream:
- Buy a large bottle of moisturizing cream (such as Eucerin). Avoid those with fragrances.
- Put the cream on any dry or itchy area 3 times per day.
- After warm water baths or showers, trap the moisture in the skin. Do this by putting on the cream everywhere after bathing. Use the cream within 3 minutes of completing the bath.
- During the winter, apply the cream every day to prevent dry skin.
-
Steroid Cream:
- For very itchy spots, use 1% hydrocortisone cream (such as Cortaid). No prescription is needed.
- Use up to 3 times per day as needed until the itching is better.
- Eventually, the moisturizing cream will be all that you need for treating dry skin.
-
Humidifier:
- If your winters are dry, protect your child's skin from the constant drying effect.
- Do this by running a room humidifier full time.
-
Preventing Dry Skin:
- Don't use soaps or bubble bath.
- Wash the hands with warm water. Use soap only if the hands are very dirty. Also, use soap for anything that won't come off with water.
- Don't use swimming pools or hot tubs. Reason: Pool chemicals are very drying.
- Run a humidifier in the winter if the air is dry.
- During cold weather, wear gloves outside. This helps prevent drying of the skin.
- Drink lots of fluids.
-
Call Your Doctor If:
- Dry skin lasts more than 2 weeks on treatment
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.
Cradle Cap
Is this your child's symptom?
- A scaly rash on the scalp that starts in newborns
If NOT, try one of these:
Symptoms of Cradle Cap
- Yellow scales and crusts attached to the scalp
- Occurs in patches
- Scales can be greasy or dry
- Not itchy or painful
- Begins in the first 2 to 6 weeks of life
Cause of Cradle Cap
- Cradle cap is probably caused by hormones from the mother. These hormones cross the placenta before birth. The hormones cause the oil glands in the skin to become overactive. They then release more oil than normal.
- Dead skin cells normally fall off. The extra oil causes these cells to "stick" to the skin. These cells form yellow crusts and scales on the scalp.
When to Call for Cradle Cap
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Self Care at Home
|
Call Doctor or Seek Care Now
- Baby under 1 month old with tiny water blisters or pimples in a cluster
- Your child looks or acts very sick
Call Doctor Within 24 Hours
- Baby under 1 month old with any water blisters or pimples
- You think your child needs to be seen
Call Doctor During Office Hours
- Raw rash behind the ears
- Rash spreads beyond the scalp
- Cradle cap gets worse with treatment
- Cradle cap lasts longer than 12 months
- You have other questions or concerns
Self Care at Home
- Mild cradle cap
Care Advice for Cradle Cap
-
What You Should Know About Cradle Cap:
- Cradle cap is a common skin condition of newborns.
- It's caused by overactive oil glands in the scalp.
- It's harmless and will go away on its own. But it takes time.
- Here is some care advice that should help.
-
Shampoo Daily:
- Wash the hair with an anti-dandruff shampoo (such as Head and Shoulders). Do this twice a week. No prescription is needed. Note: The daily use of anti-dandruff shampoo isn't approved until after 2 years old. But, using it twice a week is fine.
- On the other days, wash the hair with baby shampoo.
-
Scalp Massage:
- While the hair is lathered, massage the scalp with a soft brush. You can also use a rough washcloth or your fingers for 5 minutes. Don't worry about hurting the soft spot.
-
Baby Oil:
- If the scalp has thick crusts (scales), put some baby oil on the scalp. Do this for 15 minutes before shampooing to soften the crusts.
- Wash all the oil off, however, or it may worsen the cradle cap. (Reason: The oil blocks the oil glands on the baby's scalp.)
- Do not use olive oil. (Reason: may increase the growth of yeast)
- Cradle cap lotions for loosening up the scales are also available without a prescription. Apply the lotion 15 minutes before shampooing.
-
Steroid Cream:
- If the rash on the scalp is red and irritated, use 1% hydrocortisone cream. An example is Cortaid. No prescription is needed.
- Put this on once a day.
- After 1 hour, wash it off with soap and water.
- Do this for 7 days or less.
-
Expected Course:
- Cradle cap will eventually go away on its own between 6 and 12 months of age. Usually, it doesn't cause any symptoms (such as pain or itching).
- Therefore, treatment is optional. It is mainly done for cosmetic reasons.
- Shampoos, lotions and brushing will reduce the thickness of the scales. They will usually make them go away sooner.
-
Return to Child Care:
- Cradle cap cannot be spread to others.
- Your child does not need to miss any child care.
-
Call Your Doctor If:
- Gets worse with treatment
- Lasts over 12 months of age
- You think your child needs to be seen
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.
Croup
Is this your child's symptom?
- Barky cough and hoarse voice caused by a virus
- Croup is a viral infection of the voicebox (larynx)
- The croupy cough is tight, low-pitched, and barky (like a barking seal)
- The voice or cry is hoarse (called laryngitis)
- Some children with severe croup get a harsh, tight sound while breathing in. This is called stridor.
If NOT, try one of these:
Stridor: A nother Health Problem of Croup
- Stridor is a harsh, raspy tight sound best heard with breathing in
- Loud or constant stridor means severe croup. So does stridor at rest (when not crying or coughing).
- All stridor needs to be treated with warm mist
- Most children with stridor need treatment with a steroid (such as Decadron)
- For any stridor, see First Aid for treatment
Causes of a Croupy Cough
- Viral Croup. Viruses are the most common cause of croup symptoms. Many respiratory viruses can infect the vocal cord area and cause narrowing. Even influenza (the flu) can do this. A fever is often present with the barky cough.
- Allergic Croup. A croupy cough can occur with exposure to pollens or allergens in a barn. A runny nose, itchy eyes and sneezing are also often present.
- Inhaled Powder. Breathing in any fine substance can trigger 10 minutes of severe coughing. Examples are powdered sugar, flour dust or peanut dust. They can float into the lungs. This is not an allergic reaction.
- Airway Foreign Object (Serious). Suspect when there is a sudden onset of coughing and choking. Common examples are peanut and seeds. Peak age is 1 to 4 years.
- Food Allergy (Serious). Croup symptoms can also be caused by a food allergy. This can be life-threatening (anaphylaxis). Examples are nuts or fish.
When to Call for Croup
Call 911 Now
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Self Care at Home
|
Call 911 Now
- Severe trouble breathing (struggling for each breath, constant severe stridor)
- Passed out or stopped breathing
- Lips or face are bluish when not coughing
- Croup started suddenly after bee sting, taking a new medicine or allergic food
- Drooling, spitting or having great trouble swallowing. Exception: drooling due to teething.
- You think your child has a life-threatening emergency
Call Doctor or Seek Care Now
- Stridor (harsh sound with breathing in) is heard now
- Trouble breathing. Exception: present only when coughing.
- Lips or face have turned bluish during coughing
- Ribs are pulling in with each breath (retractions)
- Breathing is much faster than normal
- Can't bend the neck forward
- Severe chest pain
- Age less than 1 year old with stridor
- Had croup before that needed Decadron
- Weak immune system. Examples are: sickle cell disease, HIV, cancer, organ transplant, taking oral steroids.
- High-risk child (such as cystic fibrosis or other chronic lung disease)
- Fever over 104° F (40° C)
- Age less than 12 weeks old with fever. Caution: do NOT give your baby any fever medicine before being seen.
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Call Doctor Within 24 Hours
- Stridor (harsh sound with breathing in) occurred but not present now
- Nonstop coughing
- Age less than 1 year old with a croupy cough
- Earache or ear drainage
- Fever lasts more than 3 days
- Fever returns after being gone more than 24 hours
- You think your child needs to be seen, but the problem is not urgent
Call Doctor During Office Hours
- Coughing causes vomiting 3 or more times
- Croup is a frequent problem (3 or more times)
- Barky cough lasts more than 14 days
- You have other questions or concerns
Self Care at Home
- Mild croup (barky cough) with no stridor
Care Advice for Croup
-
What You Should Know About Croup:
- Most children with croup just have a barky cough.
- Some have tight breathing (called stridor). Stridor is a loud, harsh sound when breathing in. It comes from the area of the voicebox.
- Coughing up mucus is very important. It helps protect the lungs from pneumonia.
- We want to help a productive cough, not turn it off.
- Here is some care advice that should help.
-
First Aid For Stridor (Harsh sound with breathing in):
- Breathe warm mist in a closed bathroom with the hot shower running. Do this for 20 minutes.
- You could also use a wet washcloth held near the face.
- Caution: Do not use very hot water or steam which could cause burns.
- If warm mist fails, breathe cool air by standing near an open refrigerator. You can also go outside with your child if the weather is cold. Do this for a few minutes.
-
Calm Your Child if He or She has Stridor:
- Crying or fear can make stridor worse.
- Try to keep your child calm and happy.
- Hold and comfort your child.
- Use a soothing, soft voice.
-
Humidifier:
- If the air in your home is dry, use a humidifier.
- Reason: Dry air makes croup worse.
-
Homemade Cough Medicine:
- Goal: Decrease the irritation or tickle in the throat that causes a dry cough.
- Age 3 months to 1 year: Give warm clear fluids to treat the cough. Examples are apple juice and lemonade. Amount: Use a dose of 1-3 teaspoons (5-15 mL). Give 4 times per day when coughing. Caution: Do not use honey until 1 year old.
- Age 1 year and older: Use Honey ½ to 1 teaspoon (2-5 mL) as needed. It works as a homemade cough medicine. It can thin the secretions and loosen the cough. If you don't have any honey, you can use corn syrup.
- Age 6 years and older: Use Cough Drops to decrease the tickle in the throat. If you don't have any, you can use hard candy. Avoid cough drops before 6 years. Reason: risk of choking.
-
Non-Prescription Cough Medicine (DM):
- Non-prescription cough medicines are not advised. Reason: No proven benefit for children and not approved under 6 years old. (FDA)
- Honey has been shown to work better for coughs. Caution: Do not use honey until 1 year old.
- If age 6 years or older, you might decide to use a cough medicine. Choose one with dextromethorphan (DM) such as Robitussin Cough syrup. DM is present in most non-prescription cough syrups.
- When to Use: Give only for severe coughs that interfere with sleep or school.
- DM Dose: Give every 6 to 8 hours as needed.
-
Coughing Fits or Spells - Warm Mist and Fluids:
- Breathe warm mist, such as with shower running in a closed bathroom.
- Give warm clear fluids to drink. Examples are apple juice and lemonade.
- Age under 3 months. Don't use warm fluids.
- Age 3 - 12 months of age. Give 1 ounce (30 mL) each time. Limit to 4 times per day.
- Age over 1 year of age. Give as much warm fluids as needed.
- Reason: Both relax the airway and loosen up any phlegm.
-
Fluids - Offer More:
- Try to get your child to drink lots of fluids.
- Goal: Keep your child well hydrated.
- It also loosens up any phlegm in the lungs. Then it's easier to cough up.
-
Fever Medicine:
- For fevers above 102° F (39° C), give an acetaminophen product (such as Tylenol).
- Another choice is an ibuprofen product (such as Advil).
- Note: Fevers less than 102° F (39° C) are important for fighting infections.
- For all fevers: Keep your child well hydrated. Give lots of cold fluids.
-
Sleep Close By to Your Child:
- Sleep in the same room with your child for a few nights.
- Reason: Stridor can start all of a sudden at night.
-
Avoid Tobacco Smoke:
- Tobacco smoke makes croup much worse.
-
Return to School:
- Your child can go back to school after the fever is gone.
- Your child should also feel well enough to join in normal activities.
- For practical purposes, the spread of croup and colds cannot be prevented.
-
What to Expect:
- Most often, croup lasts 5 to 6 days and becomes worse at night.
- The croupy cough can last up to 2 weeks.
-
Call Your Doctor If:
- Trouble breathing occurs
- Stridor (harsh raspy sound) occurs
- Croupy cough lasts more than 14 days
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.

- Stridor is a harsh, tight sound with breathing in. Stridor means the croup is severe.
- Breathe warm mist in a closed bathroom with the hot shower running. Do this for 20 minutes.
- Other Option: Use a wet washcloth held near the face. Can also use a humidifier containing warm water.
- Caution: Do not use very hot water or steam which could cause burns. Hot steam can also cause high body temperatures.
- If warm mist fails, breathe cool air by standing near an open refrigerator. You can also go outside with your child if the weather is cold. Do this for a few minutes.
Crying Baby - Before 3 Months Old
Is this your child's symptom?
- A baby less than 3 months old is crying and you don't know why
- Crying is the only symptom
- The type of frequent crying called colic is included
- For crying with an illness or other symptom, go to that care guide
Crying from hunger, see
Causes of Unexplained Crying
- Hungry Baby. The most common reason babies cry is because they are hungry. They stop crying at the onset of feeding. By the end of the feeding, they are happy.
- Sleepy Baby. The second reason babies cry is they need sleep. They need their parent to put them in a comfortable position. It may be swaddled and on their back. Then they fuss a little and fall asleep.
- Fed Too Much. Some babies cry because of a bloated stomach from overfeeding. Unlike gas, too much milk can cause discomfort that lasts a short time.
- Caffeine. Caffeine is a stimulant that can cause increased crying and trouble falling asleep. Breastfeeding mothers need to limit their caffeine intake.
- Clothing. Being too hot or too cold can make a baby cry. So can clothing that is too tight.
- Dirty Diaper. Stool is very irritating to the skin. If not cleaned off, it can cause pain and burning.
- Colic. Colic is the main cause of recurrent crying during the early months. All babies have some normal fussy crying every day. When this occurs over 3 hours per day, it's called colic. When they are not crying, they are happy.
- Pain (Serious). Painful causes include an earache, mouth ulcers, or a raw diaper rash. An ulcer on tip of penis may also cause pain and crying. These babies cry a lot and are not happy when they are not crying. They need to see a doctor to make a diagnosis. Fever in this age group is serious until proven otherwise. Shaken baby syndrome is a concern.
Myths About Causes of Crying
- Not Due to Gas. Gas passing through normal intestines does not cause pain or crying. All crying babies pass lots of gas. Their stomachs also make lots of gassy noises. The gas comes from swallowed air. The gas is normal. It does not become trapped nor cause any pains. That's why burping a baby doesn't help the crying. Blaming gas is a myth.
Definition of Colic
- A lot of crying once or twice per day
- Usually consolable when held and comforted
- Acts normal (happy, contented) between bouts of crying
- The baby is getting enough to eat and is not hungry
- The baby is not sick
- Onset most often before 2 weeks of age
- Usually goes away by 3 months of age (sometimes up to 4 months)
When to Call for Crying Baby - Before 3 Months Old
Call 911 Now
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Self Care at Home
|
Call 911 Now
- Not moving or very weak
- You think your child has a life-threatening emergency
Call Doctor or Seek Care Now
- Age less than 1 month old and looks or acts abnormal in any way
- Age less than 12 weeks old with fever. Caution: do NOT give your baby any fever medicine before being seen.
- Bulging or swollen soft spot
- Swollen scrotum or groin
- Vomiting
- Cries when you touch, move or hold your baby
- Could be an injury
- Nonstop crying lasts more than 2 hours. (Your baby can't be consoled using this Care Advice).
- Will not drink or drinks very little for more than 8 hours
- Not alert when awake ("out of it")
- You are afraid someone might hurt or shake your baby
- High-risk child (such as with heart or brain disease)
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Call Doctor Within 24 Hours
- Not gaining weight or seems hungry
- New crying but your baby can be consoled. (Your baby will stop crying, but cause of crying not clear)
- You are worn out from all the crying
- You think your child needs to be seen, but the problem is not urgent
Call Doctor During Office Hours
- Your baby has never been checked for excessive crying
- Crying started after 1 month of age
- Crying occurs 3 or more times per day
- You have other questions or concerns
Self Care at Home
- Normal crying in all babies
- Colic (Excessive crying in a well baby who can be consoled)
Care Advice for Normal Crying or Colic
-
What You Should Know About Crying:
- Normal Crying: All babies cry when they are hungry. Also, the normal baby has 1 to 2 hours of unexplained crying each day. It is scattered throughout the day. As long as they are happy and content when they are not crying, this is normal.
- Colic: Some babies are very hard to comfort. Some babies also cry a lot (over 3 hours per day). If growing normally and have a normal medical exam, the crying is called colic. Remind yourself that colic is due to your baby's temperament. It has nothing to do with your parenting or any medical disease.
- Here is some care advice that should help both types of crying.
-
Feedings:
- For formula-fed babies, feed if more than 2 hours since the last feeding. For breast-fed babies, feed if more than 1½ hours since the last feeding.
- Be careful not to feed your baby every time she cries. Some babies cry because of a bloated stomach from overfeeding. Let your baby decide when she's had enough milk. (For example, she turns her head away.) Don't encourage your baby to finish what's in the bottle.
- Caffeine. If breastfeeding, decrease your caffeine intake. Limit your coffee, tea and energy drinks to 2 servings per day. That's 2 cups or 16 ounces (480 mL).
-
Hold and Comfort for Crying:
- Hold and try to calm your baby whenever he cries without a reason. Hold your baby flat to help them relax and go to sleep.
- Rock your child in a rocking chair, in a cradle or while standing. Many babies calm best with rapid tiny movements like vibrations.
- Place in a windup swing or vibrating chair.
- Take for a stroller ride, outdoors or indoors.
- Do anything else you think may be comforting. Examples are using a pacifier, massage, or warm bath.
-
Swaddle your Baby in a Blanket for Crying:
- Swaddling is the most helpful technique for calming crying babies. It also keeps your baby from waking up with a startle reflex.
- Use a big square blanket and the "burrito-wrap" technique:
- Step 1: Have the arms inside and straight at the sides.
- Step 2: Pull the left side of the blanket over the upper body and tuck.
- Step 3: Fold the bottom up with the knees a little flexed. Safe swaddling keeps the legs in a straddle position.
- Step 4: Pull the right side over the upper body and tuck.
- Caution: Don't cover your baby's head or overheat your baby.
- Caution: Stop swaddling when your baby shows signs of rolling over. Age limit: 4 months.
- Read the book (or view the DVD),"The Happiest Baby on the Block". Both products are authored by Dr. Harvey Karp. It is the best resource on how to calm fussy babies.
-
White Noise for Crying:
- Swaddling works even better when paired with a low-pitched white noise. Examples are a CD, vacuum cleaner, fan or other constant sound.
- Caution: Avoid making white noise too loud. Reason: risk of hearing damage.
- Keep the white noise on any time your baby is crying.
- When your baby is awake and not crying, keep your baby unwrapped. Turn off the white noise. Reason: So she can get used to the normal sounds of your home. (For details, view Dr. Karp's DVD.)
-
Falling Asleep on their Own:
- Often babies cry because they need to sleep. If over 2 hours have passed since the last nap, this probably is the reason.
- You have tried different ways to comfort your baby. You fed him recently. Nothing you do seems to help your baby relax. So, now, it's time to get out of the way.
- Swaddle your baby. Place him on his back in his crib. Turn on some white noise or soothing music. Then, leave the room.
- Let your baby fuss until he falls asleep.
- For some overtired babies, this is the only answer.
-
Encourage Nighttime Sleep (Rather Than Daytime Sleep):
- Try to keep your child from sleeping too much during the daytime.
- If your baby has napped 2 hours or longer, gently wake him up. Play with or feed your baby, depending on his needs. This will lessen the amount of time your baby is awake at night.
-
Warning: Never Shake a Baby
- It can cause bleeding on the brain. Severe brain damage can happen in a few seconds.
- Never leave your baby with someone who is immature or has a bad temper.
- If you are frustrated, put your baby down in a safe place.
- Call or ask a friend or relative for help.
- Take a break until you calm down.
-
What to Expect:
- The right technique should start to reduce the crying. You may have to try several things before finding the best method.
- The crying should start to decrease to about 1 hour per day.
- Colic gets better after 2 months of age. Most often, it is gone by 3 months.
-
Call Your Doctor If:
- Your baby starts to look or act abnormal
- Cries nonstop for more than 2 hours
- Your child can't be consoled using this advice
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.
Crying Child - 3 Months and Older
Is this your child's symptom?
- A child more than 3 months old is crying and you don't know why
- Your child is too young to tell you why
- Age: Most of these children are younger than 2 years old
- Crying is the only symptom
- For crying with an illness or other symptom, go to that care guide
If NOT, try one of these:
Causes of Unexplained Crying
- New Illness. Coming down with an illness is the main physical cause. Young children cry about being sick, even if they don't have any pain.
- Physical Pain. Painful causes include earache, sore throat, mouth ulcers, or a raw diaper rash. A sore on the penis or constipation may also cause pain or crying.
- Behavioral Causes. Most crying means the child is upset about something. Crying can occur when a young child is separated from his parents. Other examples are crying with tantrums or when overtired. This guide detects many babies with sleep problems. Crying always occurs during re-training programs for bad sleep habits. Some preverbal children cry any time they want something.
- Hunger. After the early months, most parents can recognize hunger and feed their child. If they don't, the child may cry.
- Cold Medicines. Drugs like Sudafed can also cause crying. Note: FDA does not advise cough and cold medicines for children under 4 years.
Myths About Causes of Crying
- Not Due to Teething. Teething may cause some babies to be fussy. But, in general, it does not cause crying.
-
Not Due to Gas. Gas passing through normal intestines does not cause pain or crying.
When to Call for Crying Child - 3 Months and Older
Call 911 Now
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Self Care at Home
|
Call 911 Now
- Not moving or very weak
- You think your child has a life-threatening emergency
Call Doctor or Seek Care Now
- Could be an injury
- Nonstop crying lasts more than 2 hours. (Your child can't be consoled using this Care Advice)
- You are afraid someone might hurt or shake your child
- Will not drink or drinks very little for more than 8 hours
- Not alert when awake ("out of it")
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Call Doctor Within 24 Hours
- You think pain (such as an earache) is causing the crying
- New crying but your child can be consoled. Cause of crying is not clear.
- You think your child needs to be seen, but the problem is not urgent
Call Doctor During Office Hours
- Mild, off-and-on fussiness without a cause lasts more than 2 days
- Crying is a frequent problem
- You have other questions or concerns
Self Care at Home
- Mild fussiness without a cause is present less than 2 days
- Normal protest crying
- Temper tantrum crying
- Sleep problem crying
Care Advice
Mild Fussiness of Unknown Cause
-
What You Should Know:
- Your child is crying and fussing more than normal. But, if acting normal when not crying, the cause is probably not serious.
- He could be coming down with an illness. Most often, that will become clear in a day or so.
- He could be reacting to some changes in your home or child care setting. See if you can come up with some ideas.
- At times, children can also go through a "clingy phase" without a reason.
- If the crying stops with comforting, it's not serious.
- Here is some care advice that should help.
-
Comfort Your Child:
- Try to comfort your child by holding, rocking, or massage.
- Talk in a quiet, calm voice.
-
Undress Your Child- Check the Skin:
- Sometimes, part of the clothing is too tight. Loosen it.
- Also, check the skin for redness or swelling (such as an insect bite).
-
Stop Any Over-the-Counter Medicines:
- If your child is taking a cough or cold med, stop it.
- The crying should stop within 4 hours.
- Allergy meds like Benadryl can cause screaming in a small number of children. Also, may cause some children to be more fussy than normal.
- Drugs that lessen congestion like Sudafed can cause crying.
- The FDA does not approve any of these drugs for children under 4 years old.
-
Sleep - Take a Nap:
- If your child is tired, put him to bed.
- If he needs to be held, hold him quietly in your arms. Sometimes, lying next to him will comfort him.
- Some overtired infants need to fuss themselves to sleep.
-
Warning: Never Shake a Baby
- It can cause bleeding on the brain. Severe brain damage can happen in a few seconds.
- Never leave your baby with someone who is immature or has a bad temper.
- If you are frustrated, put your baby down in a safe place.
- Call or ask a friend or relative for help.
- Take a break until you calm down.
-
What To Expect:
- Most fussiness with illnesses goes away when the illness does.
- Fussiness may be due to family stress or change (such as new child care). Fussiness due to this cause lasts less than 1 week.
-
Call Your Doctor If:
- Nonstop crying lasts more than 2 hours
- Crying with an illness gets worse
- Mild crying lasts more than 2 days
- You think your child needs to be seen
- Your child becomes worse
Normal Protest Crying
-
What You Should Know:
- Normal children cry when they don't get their way.
- Normal children cry when you make changes in their routines.
- Crying is how young children communicate in the first years of life.
- Crying can mean, "I don't want to."
- This is called normal protest crying and is not harmful.
- Do not assume that crying means pain.
-
Call Your Doctor If:
- Crying becomes worse
- Your child does not improve with this advice
- You have other questions or concerns
Temper Tantrum Crying
-
What You Should Know:
- Crying is the most common symptom of a temper tantrum.
- Temper tantrums occur when your child is angry or trying to get his way.
- This is likely the cause of the crying if it occurs at these times.
- All kids have some temper tantrums, starting at about 9 months of age.
-
Tips for Dealing with Temper Tantrums:
- Ignore most tantrums (such as wanting something the child doesn't need).
- Don't give your child an audience. Leave the room.
- For tantrums from frustration (such as when something doesn't work), help your child.
- For tantrums that involve hitting or throwing objects, put in timeout. Leave your child there until he calms down.
- Don't give in to tantrums. No means No.
- Be a good role model. Do not yell or scream at others (adult tantrums).
-
Call Your Doctor If:
- Crying becomes worse
- Your child does not improve with this advice
- You have other questions or concerns
Sleep Problem Crying
-
What You Should Know:
- Sleep problems can cause crying. Suspect this if most of your child's crying occurs in his crib or bed. The crying mainly occurs when you put him down for naps and at night. Also, suspect a sleep problem if your child acts normal during the daytime.
- Sleep problems are common in childhood.
-
Tips for Treating the Sleep Problem:
- Re-train your child to be a good sleeper at bedtime and naptime.
- Place your child in the crib "sleepy but awake."
- Once placed in the crib, don't take your child out again.
- If needed, visit your child every 10 minutes or so until asleep.
- For waking at night, it's fine to hold your child until calm.
- Do all of this in a loving way with a calm voice.
- Never feed until asleep. Always stop before asleep.
- Never sleep in the same bed with your child.
-
Call Your Doctor If:
- Crying becomes worse
- Your child does not improve with this advice
- You have other questions or concerns
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.
Cut, Scrape, or Bruise
Is this your child's symptom?
- Injuries to the skin anywhere on the body surface
- Includes cuts, scratches, scrapes, bruises and swelling
If NOT, try one of these:
Types of Skin Injury
- Cuts, lacerations, gashes and tears. These are wounds that go through the skin to the fat tissue. Caused by a sharp object.
- Scrapes, abrasions, scratches and floor burns. These are surface wounds that don't go all the way through the skin. Scrapes are common on the knees, elbows and palms.
- Bruises. These are bleeding into the skin from damaged blood vessels. Caused by a blunt object. They can occur without a cut or scrape.
When Sutures (Stitches) are Needed for Cuts
- Any cut that is split open or gaping needs sutures.
- Cuts longer than ½ inch (12 mm) usually need sutures.
- On the face, cuts longer than ¼ inch (6 mm) usually need to be seen. They usually need closure with sutures or skin glue.
- Any open wound that may need sutures should be seen as soon as possible. Ideally, they should be checked and closed within 6 hours. Reason: to prevent wound infections. There is no cutoff, however, for treating open wounds.
Cuts Versus Scratches: Helping You Decide
- The skin is about 1/8 inch (3 mm) thick.
- A cut (laceration) goes through it.
- A scratch or scrape (wide scratch) doesn't go through the skin.
- Cuts that gape open at rest or with movement need stitches to prevent scarring.
- Scrapes and scratches never need stitches, no matter how long they are.
- So this distinction is important.
When to Call for Cut, Scrape, or Bruise
Call 911 Now
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Self Care at Home
|
Call 911 Now
- Major bleeding that can't be stopped
- Deep cut to chest, stomach, head or neck (such as with a knife)
Call Doctor or Seek Care Now
- Skin is split open or gaping and may need stitches
- Severe pain and not better 2 hours after taking pain medicine
- Age less than 1 year old
- Dirt in the wound is not gone after 15 minutes of scrubbing
- Skin loss from bad scrape goes very deep
- Bad scrape covers large area
- Cut or scrape looks infected (redness, red streak or pus)
- Cut or scrape and no past tetanus shots
- You think your child has a serious injury
- You think your child needs to be seen, and the problem is urgent
Call Doctor Within 24 Hours
- Very large bruise after a minor injury
- Some bruises appear without any known injury
- You think your child needs to be seen, but the problem is not urgent
Call Doctor During Office Hours
- Dirty cut and no tetanus shot in more than 5 years
- Clean cut and no tetanus shot in more than 10 years
- Doesn't heal by 10 days
- You have other questions or concerns
Self Care at Home
- Minor cut, scrape or bruise (minor bleeding that stops)
Care Advice for Minor Cuts, Scrapes or Bruises
-
Cuts, Scratches and Scrapes - Treatment:
- Use direct pressure to stop any bleeding. Do this for 10 minutes or until the bleeding stops.
- Wash the wound with soap and water for 5 minutes. Try to rinse the cut under running water.
- Caution: Never soak a wound that might need sutures. Reason: It may become more swollen and harder to close.
- Gently scrub out any dirt with a washcloth.
- Use an antibiotic ointment (such as Polysporin). No prescription is needed. Then, cover it with a bandage (such as Band-Aid). Change daily.
-
Liquid Skin Bandage for Minor Cuts and Scrapes:
- Liquid skin bandage seals wounds with a plastic coating. It lasts up to 1 week.
- Liquid skin bandage has several benefits compared to other bandages (such as Band-Aid). Liquid bandage only needs to be put on once. It seals the wound and may promote faster healing and lower infection rates. Also, it's water-proof.
- Wash and dry the wound first. Then, put on the liquid. It comes with a brush or swab. It dries in less than a minute.
- You can get this product at a drugstore near you. There are many brands of liquid bandage. No prescription is needed.
-
Bruises - Treatment:
- Use a cold pack or ice bag wrapped in a wet cloth. Put it on the bruise once for 20 minutes. This will help to stop the bleeding.
- After 48 hours, use a warm wet wash cloth. Do this for 10 minutes 3 times per day. This helps to reabsorb the blood.
-
Pain Medicine:
- To help with the pain, give an acetaminophen product (such as Tylenol).
- Another choice is an ibuprofen product (such as Advil).
- Use as needed.
-
Tetanus Shot:
- A tetanus shot update may be needed for cuts and other open wounds.
- Check your vaccine records to see when your child got the last one.
- For Dirty Cuts and Scrapes. If last tetanus shot was given over 5 years ago, need a booster.
- For Clean Cuts. If last tetanus shot was given over 10 years ago, need a booster.
- See your child's doctor for a booster during regular office hours. It's safe to give it within 3 days or less.
-
What to Expect:
- Small cuts and scrapes heal up in less than a week.
-
Call Your Doctor If:
- Bleeding does not stop after using direct pressure to the cut
- Starts to look infected (pus, redness)
- Doesn't heal by 10 days
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.

This bruise is one day old.
Bruises (contusions) result from a direct blow or a crushing injury; there is bleeding into the skin from damaged blood vessels without an overlying cut or abrasion.

This picture shows a shallow abrasion on the left elbow.
First Aid Care Advice for Minor Abrasion:
- Apply direct pressure for 10 minutes to stop any bleeding.
- Wash the abrasion with soap and water.
- Gently scrub out any dirt with a washcloth.
- Apply an antibiotic ointment, covered by a Band-Aid or dressing. Change daily.
- Another option is to use a Liquid Skin Bandage that only needs to be applied once. Avoid ointments with this.

This scalp laceration (cut) is gaping open. It will require closure with sutures or medical staples.
First Aid Care Advice:
- Apply direct pressure for 10 minutes to stop any bleeding.
- Wash the cut with soap and water.

The photo shows 3-4 parallel scratches on the wrist caused by a cat.
First Aid Care Advice:
- Wash the scratches with soap and water.
- Apply an antibiotic ointment twice daily.
- Watch closely for signs of infection, especially the first 1-3 days.

- Wash the wound with soap and water for 5 minutes.
- Gently scrub out any dirt with a washcloth.
- Cover the wound with a sterile gauze or a clean cloth.
- Apply direct pressure for 10 minutes to stop any bleeding.

This abrasion near the elbow occurred 3 days ago. The picture shows an abrasion that is starting to crust over.
There are no signs of infection (e.g., spreading redness, pus).

- Apply direct pressure for 10 minutes to stop any bleeding.
- Wash the wound with soap and water.
- Cover the wound with a sterile gauze or a clean cloth until seen.

This photo shows a gaping laceration (cut) of the chin. It will require closure with either sutures or with skin glue (i.e., Dermabond).
First Aid Care Advice:
- Apply direct pressure for 10 minutes to stop any bleeding.
- Wash the cut with soap and water.
- Cover with a gauze dressing or adhesive bandage (e.g., Band-Aid).

This scalp laceration (cut) is gaping open. It will require closure with sutures or medical staples.
First Aid Care Advice:
- Apply direct pressure for 10 minutes to stop any bleeding.
- Wash the cut with soap and water.

This photo shows a scalp laceration after it has been closed with 4 metal medical staples.

The photograph shows a chin laceration that was closed with skin glue (i.e., Dermabond).
Dermabond (2-octylcyanoacrylate, Ethicon) is a tissue adhesive or "skin glue" which received FDA approval in the United States in 1998. It is used as an alternative to suturing for the repair of simple lacerations. The cosmetic outcome of wounds closed with tissue adhesive is comparable and in some cases superior to suturing.
To apply, the wound edges are held firmly together, and several coats of the glue are painted along the wound margins. The glue dries quickly, within 45-60 seconds. The glue will come off on its own as the wound heals and the top skin layer falls off, usually in about one week.
Diaper Rash
Is this your child's symptom?
- Any rash on the skin covered by a diaper
- Age: Diaper-wearing age group (birth to 3 years)
If NOT, try one of these:
Causes of Diaper Rash
- Irritant Diaper Rash. Mild rashes can be caused by the drying effect of soaps.
- Stool Diaper Rash. Stool left on the skin can be very irritating because it contains bacteria. Urine alone has no germs in it and usually doesn't irritate the skin. This rash is common on the scrotum or anywhere that stool can hide. Small ulcers around the anus are often from prolonged stool contact.
- Ammonia Diaper Rash. Stool and urine left in diaper too long can combine to make ammonia. It can cause a mild chemical burn. The fumes when you change the diaper will smell like ammonia. This is more common with cloth diapers.
- Diarrhea Diaper Rash. Rashes just found around the anus are common during bouts of diarrhea. Diarrhea stools also contain enzymes that digest food and irritate the skin.
- Yeast Diaper Rash. Rashes from irritants can get a secondary infection with yeast. Yeast infections are bright red. They can be raw and weepy. The borders are sharp. Small red bumps or even pimples may occur just beyond the border. If treated correctly, a diaper rash should be cured in 3 days. If not, it has probably been invaded by yeast. Treat with an anti-yeast cream.
- Bacterial Diaper Rash. Bacteria can also cause a secondary infection of irritated skin. This is less common than yeast rashes. Bacteria cause sores, yellow scabs, pimples or draining pus. They look like impetigo, a local skin bacterial infection. Can also become a painful red lump (boil)
- Cellulitis (Serious). The bacterial infection spreads into the skin. Gives redness that spreads out from the sore. The red area is painful to the touch.
- Staph Scalded Skin Syndrome (Serious). SSSS is caused by a Staph bacteria. The main finding is widespread large blisters. The skin is bright red. The baby acts very sick.
Symptoms of Diaper Rash
- Mild rashes just have areas of pink, dry skin.
- Severe rashes have areas of red skin. In some areas, the skin may become raw or even bleed.
- Pink rashes are not painful, but raw ones can be very painful. This can lead crying and poor sleep.
Prevention of Recurrent Diaper Rash
- Change diapers more often. Focus on preventing skin contact with stool.
- Rinse your baby's skin with lots of warm water when cleaning off stool. Don't depend on diaper wipes alone to cleanse the skin.
- Be sure to clean stool off all the skin folds. Cleaning the scrotum can be a challenge.
When to Call for Diaper Rash
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Self Care at Home
|
Call Doctor or Seek Care Now
- Bright red skin that peels off in sheets
- Fever and looks infected (spreading redness)
- Age less than 1 month old with tiny water blisters or pimples in a group
- Age less than 1 month old and looks infected (yellow scabs, spreading redness)
- Age less than 1 month old and looks or acts abnormal in any way
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Call Doctor Within 24 Hours
- Any pimples, blisters, boils, yellow scabs, or open sores
- You think your child needs to be seen, but the problem is not urgent
Call Doctor During Office Hours
- Rash is very raw or bleeds
- Rash has spread outside the diaper area
- Rash is not better after 3 days of using yeast cream
- You have other questions or concerns
Self Care at Home
- Mild diaper rash
Care Advice for Diaper Rash
-
What You Should Know About Diaper Rashes:
- Diaper rashes are very common in babies.
- Often caused by not cleaning stool off the skin soon enough.
- Stool is a strong irritant to the skin.
- Here's some care advice that should help.
-
Change More Often:
- Change diapers more often to prevent skin contact with stool.
- You may want to get up once during the night to change the diaper.
-
Rinse with Warm Water:
- Rinse the baby's skin with lots of warm water during each diaper change.
- Wash with a mild soap (such as Dove) only after stools. Reason: Using soap often can interfere with healing.
- Do not use diaper wipes. Reason: They leave a film of bacteria on the skin.
-
Leave Bottom Open to Air:
- Expose the bottom to air as much as possible.
- Attach the diaper loosely at the waist to help with air exposure.
- When napping, take the diaper off and lay your child on a towel. Reason: Dryness reduces the risk of yeast infections.
-
Anti-Yeast Cream:
- Most diaper rashes respond to 3 days of warm water cleansing and air exposure. If you've tried this or the rash is bright red, suspect a yeast infection.
- Buy an anti-yeast cream (such as Lotrimin.) No prescription is needed.
- Use this cream 3 times per day.
-
Raw Skin - Treatment:
- If the bottom is very raw, soak in warm water for 10 minutes. Add 2 tablespoons (30 mL) of baking soda to the tub of warm water.
- Do this 3 times per day.
- Then, put an anti-yeast ointment (such as Lotrimin) on the rash.
-
Pain Medicine:
- To help with the pain, give an acetaminophen product (such as Tylenol).
- Another choice is an ibuprofen product (such as Advil). Avoid ibuprofen under 6 months of age.
- Use as needed.
- Age less than 3 months. Don't use pain medicines unless your doctor says it's okay. Have your child seen if the rash is causing a lot of pain.
-
Sore or Scab on End of the Penis Treatment:
- Use an antibiotic ointment (such as Polysporin). No prescription is needed.
- Do this 3 times per day.
- Reason: The sore is a bacterial infection that can cause painful urination.
-
Diarrhea Rash - Use Protective Ointment:
- If your child has diarrhea and a rash around the anus, use a protective ointment. Examples are Vaseline or Desitin.
- This forms a barrier between the skin and the stool.
- Otherwise, these generally are not needed.
- Caution: Wash off the skin before putting it on.
-
What to Expect:
- With proper treatment, most diaper rashes are better in 3 days.
- If the rash does not respond, a yeast infection has probably occurred.
-
Call Your Doctor If:
- Rash isn't much better after 3 days of using yeast cream
- It starts to look infected (with sores and scabs)
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.

This photo shows a red diaper rash in the area under the diaper.
Any diaper rash that lasts longer than a couple days can become secondarily infected with Candida (yeast). Note the red spots ("satellite lesions") outside the main area of redness.
If a yeast infection is suspected, clotrimazole cream (e.g., Lotrimin; over-the-counter) should be applied 4 times daily.
Diarrhea
Is this your child's symptom?
- Sudden increase in the number and looseness of stools
- Diarrhea means 2 or more watery or very loose stools. Reason: 1 loose stool can be normal with changes in diet.
If NOT, try one of these:
Causes of Acute Diarrhea
- Virus (such as Rotavirus). An infection of the intestines from a virus is the most common cause.
- Bacteria (such as Salmonella). Less common cause. Diarrhea often contains streaks of blood.
- Food Poisoning. This causes rapid vomiting and diarrhea within hours after eating the bad food. It is caused by toxins from germs growing in foods left out too long. Most often, symptoms go away in less than 24 hours. It often can be treated at home without the need for medical care.
- Giardia (a parasite). More likely in child care center outbreaks.
- Traveler's Diarrhea. Caused by germs in food or drink. Suspect this if it follows recent foreign travel.
- Serious Causes. Most bacterial diarrhea goes away on its own. A few can cause a severe large bowel infection (such as Shigella colitis). C. difficile is a serious cause that can occur after being on strong antibiotics.
- Serious Complication: Dehydration. This is the health problem where the body has lost too much fluid. (See below for more on this).
Causes of Recurrent Diarrhea
- Cow's Milk Allergy. Can cause loose, slimy stools in babies. Can be blood-streaked. Starts within the first 2 months of life. Need to avoid cow's milk formulas.
- Toddler's Diarrhea. Toddlers who pass 3 to 6 sloppy stools per day. Stools may run out of the diaper. Symptoms begin at age 1. Symptoms resolve at age 3 or 4, after toilet trained. Harmless and no impact on growth. Fruit juice makes it worse. The cause is rapid transit time from stomach to anus. May develop irritable bowel syndrome (IBS) in adult years.
- Lactose Intolerance. Lactose is the sugar in milk. Many people cannot absorb lactose. The gut bacteria convert the lactose to gas. The main symptoms are a lot of gas, loose stools and stomach bloating. Onset usually at age 4 or 5. This most often runs in the family (genetic).
Diarrhea Scale
- Mild: 2-5 watery stools per day
- Moderate: 6-9 watery stools per day
- Severe: 10 or more watery stools per day
- The main risk of diarrhea is dehydration.
- Loose or runny stools do not cause dehydration.
- Frequent, watery stools can cause dehydration.
Dehydration: How to Know
- Dehydration means that the body has lost too much fluid. This can happen with vomiting and/or diarrhea. A weight loss of more than 3% is needed. Mild diarrhea or mild vomiting does not cause this. Neither does a small decrease in fluid intake.
- Dehydration is the most important problem caused by diarrhea. Dehydration is a reason to see your doctor right away.
- These are signs of dehydration:
- Decreased urine (no urine in more than 8 hours) happens early in dehydration. So does a dark yellow color. If the urine is light straw colored, your child is not dehydrated.
- Dry tongue and inside of the mouth. Dry lips are not helpful.
- Dry eyes with decreased or absent tears
- In babies, a depressed or sunken soft spot
- Slow blood refill test: longer than 2 seconds. First, press on the thumbnail and make it pale. Then let go. Count the seconds it takes for the nail to turn pink again. Ask your doctor to teach you how to do this test.
- Fussy, tired out or acting ill. If your child is alert, happy and playful, he or she is not dehydrated.
- A child with severe dehydration becomes too weak to stand. They can also be very dizzy when trying to stand.
Diarrhea in Breastfed Babies: How to Tell
- Diarrhea in a breastfed baby is sometimes hard to tell.
- Normal breastfed stools are loose (often runny and seedy). Stools are yellow, but sometimes can be green. The green color is from bile. Runny stools can even be bordered by a water ring. These are all normal stools.
- Breastfed babies often pass more than 6 stools per day. Until 2 months of age, they may pass a stool after each feeding. But, if stools suddenly increase in number and looseness, suspect diarrhea. If it lasts for 3 or more stools, the baby has diarrhea.
- If the stools contain mucus, blood or smell bad, this points to diarrhea.
- Other clues to diarrhea are poor eating, acting sick, or a fever.
Diarrhea in Formula-Fed Infants: How to Tell
- Formula-fed babies pass 1 to 8 stools per day during the first week. Then it starts to slow down to 1 to 4 per day. This lasts until 2 months of age.
- The stools are yellow in color and thick like peanut butter.
- Suspect diarrhea if the stools suddenly increase in number or looseness. If it lasts for 3 or more stools, the baby has diarrhea.
- If the stools contain mucus, blood, or smells bad, this points to diarrhea.
- Other clues to diarrhea are poor eating, acting sick or a fever.
- After 2 months of age, most babies pass 1 or 2 stools per day. They can also pass 1 every other day. They no longer appear to have mild diarrhea.
When to Call for Diarrhea
Call 911 Now
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Self Care at Home
|
Call 911 Now
- Not moving
- Too weak or dizzy to stand
- You think your child has a life-threatening emergency
Call Doctor or Seek Care Now
- Dehydration suspected. No urine in more than 8 hours, dark urine, very dry mouth and no tears.
- Blood in the stool
- Constant stomach pain lasts more than 2 hours
- Vomits clear liquids 3 or more times
- Age less than 1 month with 3 or more diarrhea stools in past 24 hours
- Severe diarrhea. 10 or more watery stools in the last 24 hours.
- Fever over 104° F (40° C)
- Age less than 12 weeks old with fever. Caution: do NOT give your baby any fever medicine before being seen.
- Weak immune system. Examples are: sickle cell disease, HIV, cancer, organ transplant, taking oral steroids.
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Call Doctor Within 24 Hours
- Moderate diarrhea. 6 or more watery stools in the last 24 hours.
- Stomach pain that do not go away after each diarrhea stool
- Loss of bowel control in a toilet trained child occurs 3 or more times
- Fever lasts more than 3 days
- Close contact with person or animal who has bacterial diarrhea
- Contact with reptile (snake, lizard, turtle) in past 14 days
- Travel to country at risk for diarrhea within past month
- You think your child needs to be seen, but the problem is not urgent
Call Doctor During Office Hours
- Diarrhea lasts more than 2 weeks
- Loose stools are a frequent problem
- You have other questions or concerns
Self Care at Home
- Mild diarrhea (probably caused by a virus)
- Diarrhea disease: how to prevent
Care Advice for Diarrhea
Treatment for Mild Diarrhea
-
What You Should Know About Diarrhea:
- Most diarrhea is caused by a virus.
- Bacterial infections as a cause of diarrhea are not common.
- Diarrhea is the body's way of getting rid of the germs.
- The main risk of diarrhea is dehydration. Dehydration means the body has lost too much fluid.
- Most children with diarrhea don't need to see their doctor.
- Here are some tips on how to keep ahead of the fluid losses.
-
Mild Diarrhea:
- Most kids with diarrhea can eat a normal diet.
- Drink more fluids to prevent dehydration. Formula, breastmilk and/or regular milk are good choices for diarrhea.
- Do not use fruit juices or full-strength sports drinks. Reason: they can make diarrhea worse.
- Solid foods: eat more starchy foods (such as cereal, crackers, rice, pasta). Reason: they are easy to digest.
-
Formula-Fed Babies with Frequent, Watery Diarrhea:
- Keep giving formula but feed more often. Offer as much formula as your child will take.
- Mix formula the normal way. Reason: The formula contains plenty of water and doesn't need more.
- Solid foods: If on baby foods, continue them. Cereals are best.
-
Breastfed Babies with Frequent, Watery Diarrhea:
- Give your baby breastmilk more often.
- Also, give extra fluid if breast milk isn't keeping up with the fluid losses. You can use formula or ORS (Pedialyte).
- Solid foods: If on baby foods, continue them. Cereals are best.
-
Older Children (age more than 1 year old) with Frequent, Watery Diarrhea:
- Offer as much fluid as your child will drink. If also eating solid foods, water is fine. So is half-strength Gatorade or half-strength apple juice.
- If won't eat solid foods, give milk or formula as the fluid.
- Caution: do not use most fruit juices, full-strength sports drinks or soft drinks. Reason: they can make diarrhea worse.
- Solid foods: Starchy foods are easy to digest and best. Offer cereals, bread, crackers, rice, pasta or mashed potatoes. Pretzels or salty crackers will help add some salt to meals. Some salt is good.
-
Oral Rehydration Solutions (ORS), such as Pedialyte:
- ORS is a special fluid that can help your child stay hydrated. You can use Pedialyte or the store brand. It can be bought in food stores or drug stores.
- When to use: Start ORS for frequent, watery diarrhea if you think your child is getting dehydrated. That means passing less urine than normal. Increase fluids using ORS. Continue giving breastmilk, formula or regular milk.
- Amount: For babies, give 2-4 ounces (60-120 mL) of ORS after every large watery stool.
- For children over 1 year old, give 4-8 ounces (120-240 mL) of ORS after every large watery stool. Children rarely need ORS after age 3.
- Caution: Do not give ORS as the only fluid for more than 6 hours. Reason: Your child will need calories and cry in hunger.
-
Probiotics:
- Probiotics are healthy bacteria (such as Lactobacilli). They can replace harmful bacteria in the gut (stomach).
- Age over 12 months old: Yogurt is the easiest source of probiotics. Give 2 to 6 ounces (60 to 180 mL) of yogurt. Do this twice daily. (Note: Today, almost all yogurts are "active culture".)
- Probiotic supplements can also be bought in health food stores.
-
Fever Medicine:
- For fevers above 102° F (39° C), give an acetaminophen product (such as Tylenol).
- Another choice is an ibuprofen product (such as Advil).
- Note: Fevers less than 102° F (39° C) are important for fighting infections.
- For all fevers: Keep your child well hydrated. Give lots of cold fluids.
-
Diaper Rash - Prevention:
- Wash buttocks after each stool to prevent a bad diaper rash.
- To protect the skin, use an ointment (such as Vaseline or Desitin). Put it on the skin around the anus.
-
Return to School:
- Your child can go back to school after the stools are formed.
- The fever should also be gone.
- The older child can go back if the diarrhea is mild.
- The toilet trained child also needs to have good control over loose stools.
-
What to Expect:
- Viral diarrhea lasts 5-14 days.
- Severe diarrhea only occurs on the first 1 or 2 days. But, loose stools can last for 1 to 2 weeks.
-
Call Your Doctor If:
- Blood in the diarrhea
- Dehydration suspected (no urine in over 8 hours, dark urine, very dry mouth, and no tears)
- Diarrhea lasts over 2 weeks
- You think your child needs to be seen
- Your child becomes worse
Preventing Diarrhea Disease
-
Safety Tips in All Countries:
- Hand washing is the key to preventing the spread of infections.
- Always wash the hands before eating, feeding or handling young children or cooking.
- Always wash the hands after any contact with vomit or stools.
- Wash the hands after using the toilet or changing diapers. Help young children wash their hands after using the toilet.
- Cook all poultry fully. Never serve chicken that is still pink inside. Reason: Undercooked poultry is a common cause of diarrhea in developed countries.
-
Extra Safety Tips in Developing Countries:
- Drink bottled water or boiled water. Avoid tap water, ice cubes and flavored ices.
- Eat foods that have been fully cooked and that are still hot.
- Dry foods such as bread are usually safe.
- Avoid salads and raw vegetables. Avoid fruits that cannot be peeled. Bananas, oranges and apples are safe. Wash your hands before peeling fruit.
- Avoid all undercooked meat and fish.
- Avoid buying foods and drinks from street vendors. Reason: This is a common cause of traveler's diarrhea.
- Formula for babies: Breastfeed if possible. If not, use premixed formula. If you prepare your own, mix the formula with bottled or boiled water.
- Feeding babies: Wash bottles, nipples, spoons and dishes with soap and water. Then sterilize them in boiling water for 5 minutes if possible.
- Brush your teeth with bottled or boiled water.
-
Call Your Doctor If:
- You have other questions or concerns
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.
Diarrhea Diseases From Travel
Is this your child's symptom?
- Tropical diseases that cause diarrhea
- Includes cholera, typhoid and traveler's diarrhea
- Spread by food or drink made dirty with infected human waste
- Your child has no symptoms of tropical disease. If your child has symptoms, use other guides.
- Tropical diseases occur in people who travel to or live in high-risk countries. These mainly are developing countries near the Equator. You may have traveled to a high-risk country recently.
If NOT, try one of these:
How Tropical Diarrhea Diseases are Detected by this Symptom Checker
- These diseases can't be diagnosed over the phone. But, they can be suspected based on their symptoms. They are then referred to a medical setting where a diagnosis can be made.
- Cholera will be picked up by the Diarrhea or Vomiting guides. Diarrhea that lasts too long or is severe will refer the child to be seen. Dehydration is a health problem where the body has lost too much fluid. It can be a result of diarrhea and/or vomiting. This will also be picked up in these guides.
- Typhoid will be picked up by the Diarrhea guide. Diarrhea that lasts too long or is severe will refer the child to be seen. Bloody stools or fever lasting too long also refer the child to be seen.
- Traveler's diarrhea will be picked up by the Diarrhea or Vomiting guides. Diarrhea that lasts too long or is severe will refer the child to be seen. Dehydration will also refer the child to be seen.
- Travel to a high risk country should raise the concern. However, common diseases such as viral diarrhea also must be ruled out. They occur more commonly in these countries than the serious diseases. But, severe symptoms or symptoms that last too long make us think about these other diseases.
World-wide Causes of Death in Children Under Age 5
- 6.3 million children under the age of 5 died in 2013 worldwide.
- These 5 infections account for over 50% of all early child deaths:
- Pneumonia and other respiratory diseases 19%
- Diarrhea disease 18%
- Malaria 8%
- Measles 4%
- HIV/AIDS 3%
- Poor nutrition is a factor in over half who die older than one month of age.
- Over 80% of deaths occur in Africa and Southern Asia. India accounts for 21% of under-five deaths.
- More than half are due to diseases that we could prevent or treat.
- Resource: WHO report, September 2014
Tropical Countries
- Countries in the tropics are near the Equator. They have hot and humid climates.
- The tropics are also defined as regions without a cold season.
- Many diseases in these countries are spread by an insect bite.
- In the tropics, insects never hibernate. They are present in large numbers year round.
- Other diseases here are spread by germs that multiply in warm water. The water in the tropics usually stays warm.
- Tropical diseases occur in people who live in or travel to high-risk countries.
- Climate change is a factor that has allowed these diseases to spread.
When to Call for Diarrhea Diseases From Travel
Call 911 Now
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Self Care at Home
|
Call 911 Now
- You think your child has a life-threatening emergency
Call Doctor or Seek Care Now
- Tropical disease suspected and fever present
- Tropical disease has been diagnosed and getting worse
- Tropical disease has been diagnosed and fever returns after gone for several days
- Tropical disease has been diagnosed and shaking chills return
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Call Doctor Within 24 Hours
- Tropical disease suspected, but no fever
- You think your child needs to be seen, but the problem is not urgent
Call Doctor During Office Hours
- You have other questions or concerns
Self Care at Home
- Questions about cholera
- Questions about typhoid fever
- Question about traveler's diarrhea (TD)
- Questions about preventing diarrhea during travel
Care Advice
Cholera Questions
-
What You Should Know About Cholera:
- It is a severe diarrhea disease caused by a bacteria.
- World Impact: There are over 4 million new cases per year. It causes over 100,000 deaths per year.
-
Symptoms:
- Mild to severe diarrhea. About 5% develop severe watery diarrhea.
- Without treatment, it can progress to severe dehydration and shock within 12 hours.
- Other symptoms are vomiting, leg cramps and fever.
-
Cause:
- Cholera is caused by the Vibrio cholera bacteria found in stool.
- You get sick by swallowing food or drink made dirty with germs from stools.
-
Time Period to Get Sick:
- The time from contact to symptoms is 1-5 days.
-
Contagious Period:
- The disease can be spread to others for 1-2 weeks if not treated with antibiotics.
-
Tests and Treatment:
- Stool tests are needed to diagnose it.
- It is treated with special electrolyte fluids by mouth or IV fluids. These fluids are life-saving.
- Antibiotics may also be helpful.
-
What to Expect:
- Good outcome if diarrhea losses are replaced promptly with fluid.
-
How to Prevent:
- Vaccine: New cholera vaccines taken by mouth are very protective.
- Good hand washing.
- Avoid unsafe food and drink.
- Drink only bottled or boiled water.
- Eat only well-cooked food.
-
Countries with Cholera:
- It is seen in Africa and other tropical countries.
- Rarely is seen in US in Florida and other Gulf states. Cause in US: Shellfish that isn't cooked fully.
- For more info and current high-risk countries, see the CDC website: Cholera.
-
Call Your Doctor If:
- You have other questions or concerns
Typhoid Fever Questions
-
What You Should Know About Typhoid Fever:
- It is a severe diarrhea disease caused by a bacteria.
- World Impact: There are 20 million new cases each year. It causes over 200,000 deaths each year.
-
Symptoms:
- Starts with fever, stomach pain and diarrhea.
- The fever lasts for weeks.
- The diarrhea worsens and can become bloody.
- Feeling tired, weakness and loss of appetite are common.
- A rash of small rose-colored spots may occur on the chest and stomach.
-
Cause:
- Typhoid is caused by the Salmonella typhi bacteria found in stool.
- You get sick by swallowing food or drink made dirty with germs from stools.
-
Time Period to Get Sick:
- The time from contact to symptoms is 6 to 30 days.
-
Contagious Period:
- Can be prolonged if not treated with antibiotics.
- Even those who are treated can become carriers.
-
Tests and Treatment:
- Stool tests and blood tests are needed to diagnose it.
- It is treated with special electrolyte fluids by mouth or IV fluids.
- Antibiotics are given to kill the bacteria.
-
What to Expect:
- With treatment, symptoms improve in 2 to 4 weeks.
- Without treatment, the symptoms may last for months.
- The disease may come back after treatment.
-
How to Prevent:
- Vaccine: There is a typhoid vaccine.
- Use good hand washing.
- Avoid unsafe food and drink.
- Drink only bottled or boiled water.
- Eat only well-cooked food.
-
Countries with Typhoid:
- It is common in Africa, Asia and Latin America.
- It does occur in the US in low numbers. Mainly in travelers coming back to the US.
- For more info and current high risk countries, see the CDC website.
- Resource: Typhoid Travel Alert.
-
Call Your Doctor If:
- You have other questions or concerns
Traveler's Diarrhea (TD) Questions
-
What You Should Know About Traveler's Diarrhea (TD):
- It is a disease seen in travelers to developing countries in the tropics.
- World Impact: In high-risk countries, TD affects up to 40% of travelers. There are about 20 million new cases each year. Mainly, it disrupts vacations. About 30% of people can't pursue planned activities. Deaths are very rare.
-
Symptoms:
- Sudden onset of loose stools, twice or more the normal number.
- Nausea is often present, but only 20% have vomiting.
- May also include stomach cramps and an urgent need to pass a stool.
- Fever occurs in 10%.
- Blood in the stools occurs in 5% of cases. This means the infection has become more severe.
-
Cause:
- Caused by germs from stools present in the water, food or drinks.
- Over 80% is caused by E. coli bacteria. These bacteria are not harmful ones. But, they are new to the traveler's body and gut.
- Sometimes, more serious bacteria such as Shigella are the cause.
- Parasites cause 5-10%. Diarrhea from parasites has a more gradual onset.
-
Time Period to Get Sick:
- The time from contact to symptoms is 1-3 days for bacteria.
- Diarrhea from parasites takes 2-4 weeks to start.
-
Contagious Period:
- TD can be passed to others until the stools are formed.
-
Tests and Treatment:
- Most often, the diagnosis is based upon symptoms and recent travel history. Lab tests are not needed.
- If the stools become bloody, stool tests may be done. If it lasts more than 2 weeks, parasite tests may be done.
- It is treated with special electrolyte fluids by mouth. Less than 1% of people need IV fluids.
- Probiotics (such as yogurt) may also be helpful.
- Antibiotics are sometimes given to kill the bacteria. They are mainly used if fever, bloody stools, severe diarrhea or stomach cramps occur.
-
What to Expect:
- TD is a self-limited illness.
- Most people that aren't treated have diarrhea that lasts 3 to 5 days.
- About 5% develop blood in the stools.
- It is more severe and lasts longer in young children.
-
How to Prevent:
- Wash Hands: Use good hand washing.
- Diet: Avoid unsafe food and drink. Drink only bottled or boiled water. Eat only well-cooked food.
- Medicines: In some cases, Pepto-Bismol 4 times a day is advised. Antibiotics to prevent TD are not advised for healthy people. Check with your doctor before you travel out of the country.
- Vaccine: There is no vaccine for TD.
-
Countries at Risk:
- High-risk countries are in Latin America, Africa and Southern Asia. About 40% of travelers there get diarrhea.
- Moderate-risk countries are in Southern Europe, Middle East, China and Russia. About 15% of travelers will get it.
- Low-risk countries are the US, Western Europe, Canada and Japan.
- For more info and for current high risk countries, see the CDC website: Travelers' Diarrhea.
-
Call Your Doctor If:
- You have other questions or concerns
Diarrhea Disease: How to Prevent
-
Safety Tips in All Countries:
- Hand washing is the key to prevent the spread of infections.
- Always wash the hands before eating, feeding or handling young children or cooking.
- Always wash the hands after any contact with vomit or stools.
- Wash the hands after using the toilet or changing diapers. Help young children wash their hands after using the toilet.
- Cook all poultry fully. Never serve chicken that is still pink inside. Reason: Poultry that isn't cooked all the way is a common cause of diarrhea.
-
Extra Safety Tips in Developing Countries:
- Drink bottled water or boiled water. Avoid tap water, ice cubes and flavored ices.
- Eat foods that have been fully cooked and that are still hot.
- Dry foods such as bread are usually safe.
- Avoid salads and raw veggies. Avoid fruits that cannot be peeled. Bananas, oranges and apples are safe. Wash your hands before peeling fruit.
- Avoid all meat and fish that isn't cooked all the way.
- Avoid buying foods and drinks from street vendors. Reason: This is a common cause of traveler's diarrhea.
- Formula for babies: Breastfeed if possible. If not, use premixed formula. If you prepare your own, mix the formula with bottled or boiled water.
- Feeding babies: Wash bottles, nipples, spoons and dishes with soap and water. Then sterilize them in boiling water for 5 minutes if possible.
- Brush your teeth with bottled or boiled water.
-
Call Your Doctor If:
- You have other questions or concerns
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.
Dizziness
Is this your child's symptom?
- Sensation of light-headedness or feeling faint
If NOT, try one of these:
Causes of Dizziness
- Main Cause. Usually due to reduced blood flow to the brain for a short time. It can be triggered by many normal events:
- Standing too long in one place. Reason: This causes pooling of blood in the legs.
- Standing up suddenly. Reason: This causes sudden drop in blood pressure.
- Dehydration. This can be from losing fluids and/or from not drinking enough fluid.
- Low Oxygen (such as when running and out of breath). Reason: Lower than normal oxygen levels can't meet body's needs for a short time.
- Too Much Sun or Hot Tub Use. Reason: Increased sweating causes fluid loss.
- Sweating from Sports or Hard Work. Reason: Sweating causes fluid loss.
- Fasting. Skipping a meal causes low blood sugar.
- Fever
- Motion Sickness. Main symptoms are dizziness and nausea.
- Viral Syndrome. Patients with viral illnesses (e.g., colds, flu) often say they are a bit dizzy. This is never the only symptom. It may relate to weakness from being sick.
- Vertigo (Serious). In addition to dizziness, the child complains that the room is spinning. They can't walk if they have vertigo. True vertigo is very rare in children. It's usually caused by middle ear disease.
Symptoms of Dizziness
- Feeling dizzy or light headed
- Feeling unsteady with slight loss of balance
- Feeling "woozy" or not thinking clearly
- May also have brief blurring of vision
Dizziness Scale
- Mild: walks normal
- Moderate: interferes with normal activities such as playing, school or sports
- Severe: can't stand, needs support to walk, feels like passing out now
When to Call for Dizziness
Call 911 Now
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Self Care at Home
|
Call 911 Now
- You think your child has a life-threatening emergency
Call Doctor or Seek Care Now
- Dehydration suspected. No urine in more than 8 hours, dark urine, very dry mouth and no tears.
- Dizziness caused by heat exposure, prolonged standing, or poor fluid intake. It's not gone after 2 hours of rest and fluids.
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Call Doctor Within 24 Hours
- Passed out (fainted) and caused by sudden or prolonged standing
- Moderate dizziness (interferes with normal activities) present now. Exception: dizziness caused by heat exposure, prolonged standing, or poor fluid intake.
- Fever lasts more than 3 days
- Ear pain or congestion
- You think your child needs to be seen, but the problem is not urgent
Call Doctor During Office Hours
- Mild dizziness (normal walking) lasts more than 3 days
- Dizziness is a frequent problem
- You have other questions or concerns
Self Care at Home
- Sudden or prolonged standing caused the dizziness
- Poor fluid intake caused the dizziness
- Mild dizziness from unknown cause present less than 3 days
Care Advice
Dizziness from Sudden or Prolonged Standing
-
What You Should Know:
- Standing up quickly is the most common cause of dizziness. This type of dizziness only lasts a short time. Getting out of bed is when it usually happens.
- Prolonged standing in one place is another common cause.
- Not drinking enough fluids or eating enough salt always makes it worse.
- Here is some care advice that should help.
-
Standing - Pump Legs:
- In the mornings, sit up for a few minutes before you stand up.
- This will help your blood flow stay steady and adjust before you stand up.
- With prolonged standing, contract and relax your leg muscles. Reason: This helps pump the blood back to the heart.
- Sit down or lie down if you feel dizzy.
-
Salt - Increase Intake:
- Most people with this type of dizziness (due to standing) don't get enough salt.
- Try to eat some salty foods (potato chips or pretzels) every day.
-
Fluids - Drink More:
- Drink several glasses of fruit juice, other clear fluids or water.
- This will improve your child's fluid status and blood sugar.
- If the weather is hot, make sure the fluids are cold.
-
Lie Down:
- Lie down with feet up for 1 hour.
- Reason: This will increase blood flow to the brain.
-
Prevention:
- Extra water and salty foods during sports or hot weather
- Regular mealtimes and snacks
- Enough sleep and rest
-
What to Expect:
- With treatment, the dizziness usually goes away in 1 to 2 hours.
-
Call Your Doctor If:
- After 2 hours of rest and fluids, still feels dizzy
- Your child passes out (faints)
- You think your child needs to be seen
- Your child becomes worse
Dizziness from Poor Fluid Intake
-
What You Should Know:
- Not drinking enough fluids and being a little dehydrated probably caused the dizziness.
- It should go away with drinking fluids and resting in a cool place.
- This is always made worse during hot weather. Too much sun exposure can also increase the body's need for fluid.
- Here is some care advice that should help.
-
Fluids - Drink More:
- Drink several glasses of fruit juice, other clear fluids or water.
- This will improve your child's fluid status and blood sugar.
- If the weather is hot, make sure the fluids are cold.
-
Cool Off:
- If the weather is hot, use a cold pack or washcloth to the forehead.
- Taking a cool shower or bath will help even more.
-
Lie Down:
- Lie down with feet up for 1 hour.
- Reason: This will increase blood flow to the brain.
-
Prevention:
- Extra water and salty foods during sports or hot weather
- Regular mealtimes and snacks
- Enough sleep and rest
-
What to Expect:
- With treatment, the dizziness usually goes away in 1 to 2 hours.
-
Call Your Doctor If:
- After 2 hours of rest and fluids, still feels dizzy
- Your child passes out (faints)
- You think your child needs to be seen
- Your child becomes worse
Dizziness from Unknown Cause
-
What You Should Know:
- Dizziness that goes away is a harmless symptom.
- It's usually due to not drinking enough water during sports or hot weather.
- It can also be caused by skipping a meal or too much sun.
- Sometimes, it's part of a viral illness.
- Here is some care advice that should help.
-
Lie Down:
- Lie down with feet up for 1 hour.
- Reason: This will increase blood flow to the brain.
-
Fluids - Drink More:
- Drink several glasses of fruit juice, other clear fluids or water.
- This will improve your child's fluid status and blood sugar.
- If the weather is hot, make sure the fluids are cold.
-
Cool Off:
- If the weather is hot, use a cold pack or washcloth to the forehead.
- Taking a cool shower or bath will help even more.
-
Prevention:
- Extra water and salty foods during sports or hot weather
- Regular mealtimes and snacks
- Enough sleep and rest
-
What to Expect:
- With treatment, the dizziness usually goes away in 1 to 2 hours.
- Mild dizziness with a viral illness may last 1 or 2 days.
-
Call Your Doctor If:
- After 2 hours of rest and fluids, still feeling dizzy
- Mild dizziness lasts over 3 days
- Your child passes out (faints)
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.
Drinking Fluids - Decreased
Is this your child's symptom?
- Drinking less than normal amounts of fluid
Age under 12 weeks and formula feeding, see
Causes For Drinking Less Fluid Than Normal
- Sore Throat. A sore throat is the most common cause. The pain is made worse by swallowing. Most sore throats are caused by a virus. Strep bacteria cause 20% of sore throats with fever.
- Mouth Ulcers. Mouth ulcers are another common cause of a painful mouth. The pain is made worse by swallowing. Most mouth ulcers are caused by a virus (such as Coxsackie virus).
- Nausea. Nausea means a sick stomach feeling and loss of appetite. Also called an upset stomach, but without vomiting. Usually from a viral infection of the stomach or liver.
- Blocked Nose. A common cause in bottle or breastfed infant. Reason: if nose is clogged, the baby can't breathe while sucking.
- Trouble Breathing (Serious). Shortness of breath from any lung disease can reduce fluid intake. Examples are pneumonia, wheezing or severe croup. Reason: the baby quickly gets tired from sucking and breathing at the same time.
- Foreign Object in the Esophagus (Serious). The esophagus is the tube from the mouth to the stomach. A swallowed foreign object can become stuck here. Examples are coins or small toy parts. The main symptoms are gagging, refusal of fluids or drooling. The peak age is 1 to 3 years.
- Abscess of Tonsil (Serious). A bacterial infection of the tonsil can spread to the surrounding tissues. The main symptoms are severe trouble swallowing, fever and one-sided throat pain. It's also hard to fully open the mouth. The peak age is teens.
Dehydration: How to Tell
The main risk of not drinking enough fluids is dehydration. This means the body has lost too much water. It is a reason to see a doctor right away. Your child may have dehydration if not drinking much fluid and:
- The urine is dark yellow and has not passed any in more than 8 hours.
- Inside of the mouth and tongue are dry.
- There are no tears if your child cries.
- Slow blood refill test: longer than 2 seconds. First, press on the thumbnail and make it pale. Then let go. Count the seconds it takes for the nail to turn pink again. Ask your doctor to teach you how to do this test.
- A child with severe dehydration becomes too weak to stand. They can also be very dizzy when trying to stand.
When to Call for Drinking Fluids - Decreased
Call 911 Now
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Self Care at Home
|
Call 911 Now
- Not moving or very weak
- You think your child has a life-threatening emergency
Call Doctor or Seek Care Now
- Too weak to suck or drink
- Signs of dehydration, such as:
- Has not passed urine in more than 8 hours
- Crying does not cause tears
- Very dry mouth
- Sunken soft spot
- Sleepy child
- Will not drink or drinks very little for more than 8 hours
- Will not drink and new onset of drooling
- Trouble breathing
- Can't move neck normally
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Call Doctor Within 24 Hours
- Poor drinking and also has fever
- Poor drinking lasts more than 3 days
- You think your child needs to be seen, but the problem is not urgent
Call Doctor During Office Hours
- You have other questions or concerns
Self Care at Home
- Drinking adequate amount of fluids and no signs of dehydration
Care Advice for Decreased Fluid Intake
-
What You Should Know About A Decreased Fluid Intake:
- Eating less solids during an illness is normal.
- Drinking less fluids is not.
- So far, your child does not have any signs of dehydration.
- Here are some tips to help increase fluid intake.
-
Fluids - Offer More:
- Give your child lots of their favorite liquid.
- Use fluids like chocolate milk, fruit drinks, water or even soft drinks. The type doesn't matter. The type only matters if your child has diarrhea or starts throwing up.
-
Solid Foods - Less Important:
- Don't worry about solid food intake.
- It's normal not to feel hungry or want to eat when sick.
- Preventing dehydration is the only thing that is important.
-
Sore Mouth Treatment:
- If the mouth is sore, give cold drinks.
- Do not use citrus juices.
- For babies, offer fluids in a cup, spoon or syringe rather than a bottle. Reason: The nipple may increase pain.
- To help with the pain, give an acetaminophen product (such as Tylenol). Another choice is an ibuprofen product (such as Advil). Use as needed.
-
Liquid Antacid for Mouth Pain (Age 1 Year and Older):
- For mouth pain, use a liquid antacid (such as Mylanta or the store brand). Give 4 times per day as needed. After meals often is a good time.
- Age 1 to 6 years. Put a few drops in the mouth. Can also put it on with a cotton swab.
- Age over 6 years. Use 1 teaspoon (5 mL) as a mouth wash. Keep it on the ulcers as long as possible. Then can spit it out or swallow it.
- Caution: Do not use regular mouth washes, because they sting.
-
Nasal Saline To Open a Blocked Nose:
- Use saline (salt water) nose spray to loosen up the dried mucus. If you don't have saline, you can use a few drops of water. Use distilled water, bottled water or boiled tap water.
- Step 1. Put 3 drops in each nostril. If under 1 year old, use 1 drop.
- Step 2. Blow (or suction) each nostril out while closing off the other nostril. Then, do the other side.
- Step 3. Repeat nose drops and blowing (or suctioning) until the discharge is clear.
- How Often. Do nasal saline rinses when your child can't breathe through the nose.
- Limit. If under 1 year old, no more than 4 times per day or before every feeding.
- Saline nose drops or spray can be bought in any drugstore. No prescription is needed.
- Saline nose drops can also be made at home. Use ½ teaspoon (2 mL) of table salt. Stir the salt into 1 cup (8 ounces or 240 mL) of warm water. Use bottled water or boiled water to make saline nose drops.
- Reason for nose drops: Suction or blowing alone can't remove dried or sticky mucus. Also, babies can't nurse or drink from a bottle unless the nose is open.
- Other option: use a warm shower to loosen mucus. Breathe in the moist air, then blow each nostril.
- For young children, can also use a wet cotton swab to remove sticky mucus.
-
For Shortness of Breath - Give Smaller Feedings:
- For trouble breathing, feed more often. Feed every ½ hour.
- Offer smaller amounts per feeding.
- Reason: This allows your baby to rest in between feedings.
-
Call Your Doctor If:
- Trouble swallowing gets worse
- Signs of dehydration occur
- Poor drinking lasts more than 3 days
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.
Dry Skin
Is this your child's symptom?
- Cracked skin or dry, rough skin
- Cracked skin on hands, feet and lips
- Dry, rough skin of entire body surface
If NOT, try one of these:
Causes of Cracks in the Skin
- Most cracked skin is found on the feet, hands or lips.
- Feet. The soles of the feet are most commonly involved. Most often, cracks occur on the heels and big toes. This is called tennis shoe dermatitis. Deep cracks are very painful and can bleed. The main cause is wearing wet or sweaty socks or swimming a lot.
- Hands. Cracks can develop on the hands in children. The main cause is washing the hands too much or washing dishes. Can also occur from working outside in winter weather. The worse cracks of the fingers occur with thumb sucking.
- Lips. The lips can become chapped in children from the sun or wind. If the lips become cracked, it's usually from a "lip-licking" habit. The skin around the lips can also become pink and dry. This occurs especially in children who suck on their lips.
Causes of Dry Skin
- Dry skin is a common condition.
- Soap. Dry skin is mainly caused by too much bathing and soap (soap dermatitis). Soap removes the skin's natural protective oils. Once they are gone, the skin can't hold moisture.
- Climate. Dry climates make dry skin worse, as does winter weather (called winter itch).
- Genetics also plays a role in dry skin.
- Dry skin is less common in teenagers than younger children. This is because the oil glands are more active.
- Keratosis Pilaris - dry, rough, bumpy skin on the back of the upper arms. It's made worse by soaps. Treat with moisturizing creams.
- Pityriasis Alba - dry pale spots on the face. These are more prevalent in the winter time and are also made worse by soaps. Treat with moisturizing creams.
- Eczema. Children with eczema have very dry itchy skin.
Liquid Skin Bandage For Deep, Chronic Cracks
- Liquid plastic skin bandage is a new product that seals wounds. It is a plastic coating that lasts up to 1 week.
- It is the best way to relieve pain and promote healing. As the crack heals from the bottom upward, it pushes the plastic seal up.
- After the wound is washed and dried, put the liquid on. It comes with a small brush or with a swab. It dries in less than a minute. Then apply a second coat. It's waterproof and may last a week.
- You can buy this at any drug store. Many brands of liquid bandage are available. No prescription is needed.
When to Call for Dry Skin
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Self Care at Home
|
Call Doctor or Seek Care Now
- Fever and looks infected (spreading redness)
- Cracked red lips and fever lasts 5 days or more
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Call Doctor Within 24 Hours
- Looks infected (pus or spreading redness)
- Bleeding from cracked lips
- Cracks on feet that make it hard to walk
- You think your child needs to be seen, but the problem is not urgent
Call Doctor During Office Hours
- Cracks from thumb-sucking or finger-sucking
- Peeling skin and cause is not clear
- After 2 weeks of treatment, cracked lips are not healed
- After 2 weeks of treatment, cracked skin is not healed
- After 2 weeks of treatment, dry skin is still itchy
- You have other questions or concerns
Self Care at Home
- Cracked skin on the feet
- Cracked skin on the hands
- Chapped lips
- Dry, itchy skin caused by soap or cold/dry weather
Care Advice
Treatment for Cracked Skin on the Feet
-
What You Should Know About Cracks on Feet:
- Most often, cracked skin of the feet is caused by repeated contact with moisture.
- The main cause is often wearing wet (or sweaty) socks. Swimmers also have this problem.
- The soles of the feet are most often involved. Usually, you see cracks on the heels and big toes.
- This is called tennis shoe or sneaker dermatitis.
- Cracked, dry feet usually can be treated at home.
- Here is some care advice that should help.
-
Shallow Cracks - Use Ointment:
- Cracks heal faster if protected from air exposure and drying.
- Keep the cracks constantly covered with petroleum jelly (such as Vaseline). Put it on the cracks 3 times a day.
- If the crack seems mildly infected, use an antibiotic ointment instead (such as Polysporin). No prescription is needed. Put it on the cracks 3 times a day.
- Covering the ointment with a bandage (such as Band-Aid) speeds recovery. You can also cover it with a sock.
- Option: If you have it, a liquid skin bandage works even better. Don't use liquid bandage and ointment together.
-
Deep Cracks - Use Liquid Skin Bandage:
- Deep cracks of the feet or toes usually do not heal with ointments.
- Use a liquid skin bandage that will completely seal the crack. Many brands of liquid bandage are available. No prescription is needed.
- Start with 2 layers. Put on another layer as often as needed.
- As the crack heals, the plastic layer will be pushed up.
-
Prevention of Cracks on Feet:
- Change socks whenever they are wet or sweaty.
- Take an extra pair of socks to school.
- When practical, do not wear shoes. Go barefoot or wear socks only.
- Do not use bubble bath or other soaps in the bath water. Soaps take the natural oils out of the skin.
- Use a moisturizing cream on the feet after baths or showers.
- Wear shoes that allow the skin to "breathe."
-
What to Expect:
- Most cracks heal over in 1 week with treatment.
- Deep cracks heal if you keep them covered all the time with crack sealer. Deep cracks will heal in about 2 weeks with crack sealer.
-
Call Your Doctor If:
- Starts to look infected (redness, red streak, pus)
- Cracks last more than 2 weeks on treatment
- You think your child needs to be seen
- Your child becomes worse
Treatment for Cracked Skin on the Hands
-
What You Should Know About Cracks on Hands:
- Cracked skin of the hands is usually caused by repeated contact with moisture.
- Examples are washing dishes or washing the hands often.
- Soap removes the natural protective oils from the skin.
- Cracked, dry hands usually can be treated at home.
- Here is some care advice that should help.
-
Shallow Cracks - Use Ointment:
- Cracks heal faster if protected from air exposure and drying.
- Keep the cracks constantly covered with petroleum jelly (such as Vaseline). Put it on the cracks 3 times a day.
- If the crack seems mildly infected, use an antibiotic ointment instead (such as Polysporin). No prescription is needed. Put it on the cracks 3 times a day.
- Covering the ointment with a bandage (such as Band-Aid) speeds recovery. You can also cover it with a glove.
- Option: If you have it, a liquid skin bandage works even better. Don't use liquid bandage and ointment together.
-
Deep Cracks - Use Liquid Skin Bandage:
- Deep cracks of the fingers usually do not heal with ointments.
- Use a liquid skin bandage that will completely seal the crack. Many brands of liquid bandage are available. No prescription is needed.
- Start with 2 layers. Put on another layer as often as needed.
- As the crack heals, the plastic layer will be pushed up.
-
Prevention of Cracks on Hands:
- Wash the hands with warm water.
- Use soap only if the hands are very dirty. Also, use soap for anything that won't come off with water.
- Wear gloves when washing dishes.
- During cold weather, wear gloves outside.
- Use a moisturizing cream on the hands after anytime they have been in water.
-
What to Expect:
- Most cracks heal over in 1 week with treatment.
- Deep cracks heal if you keep them covered all the time with crack sealer. Deep cracks will heal in about 2 weeks with crack sealer.
-
Call Your Doctor If:
- Starts to look infected (redness, red streak, pus)
- Cracks last more than 2 weeks on treatment
- You think your child needs to be seen
- Your child becomes worse
Treatment for Chapped Lips
-
What You Should Know About Chapped Lips:
- The lips can become chapped in children from too much sun or wind.
- If the lips become cracked, it's usually from a "lip-licking" habit.
- The skin around the lips can also become pink and dry. This occurs especially when children suck on their lips.
- Here is some care advice that should help.
-
Lip Balm:
- A lip balm should be used often, even hourly.
- Be sure to put it on after eating or drinking.
-
Avoid "Lip-Licking":
- Help your child give up the habit of lip-licking or sucking.
- This habit usually is not seen before age 6.
- This habit will only change if you can gain your child's active participation.
- Appeal to your child's pride. Show your child in a mirror how lip-sucking has affected their appearance.
- Give them a lip lubricant to put on their lips. Tell them to use it when they feel the urge to suck on them. Another option is to replace lip-sucking with chewing gum.
- Offer an incentive for going an entire day without lip-sucking. Examples of rewards are money or points towards a prize.
- Avoid any pressure or punishment. It will backfire, cause a power struggle and make the habit last longer.
-
Call Your Doctor If:
- Starts to look infected (redness, red streak, pus)
- Cracks last more than 2 weeks on treatment
- You think your child needs to be seen
- Your child becomes worse
Treatment for Dry or Itchy Skin
-
What You Should Know About Dry Skin:
- Dry skin is a common condition.
- Mainly caused by too much bathing and soap (soap dermatitis).
- Soap removes the skin's natural protective oils. Once they are gone, the skin can't hold moisture.
- Dry climates make it worse, as does winter weather (called winter itch).
- Genetics also plays a role in dry skin.
- Dry skin is less common in teenagers than younger children. This is because the oil glands are more active in teens.
- Here is some care advice that should help.
-
Bathing - Avoid Soap:
- Young children with dry skin should avoid all soaps. Soaps take the natural protective oils out of the skin. Bubble bath does the most damage.
- For young children, the skin can be cleansed with warm water alone. Keep bathing to 10 minutes or less.
- Most young children only need to bathe twice a week.
- Teenagers can get by with using soap only for the armpits, genitals, and feet. Also, use a mild soap (such as Dove).
- Do not use any soap on itchy areas or rashes.
-
Moisturizing Cream:
- Buy a large bottle of moisturizing cream (such as Eucerin). Avoid those with fragrances.
- Put the cream on any dry or itchy area 3 times per day.
- After warm water baths or showers, trap the moisture in the skin. Do this by putting on the cream everywhere after bathing. Use the cream within 3 minutes of completing the bath.
- During the winter, apply the cream every day to prevent dry skin.
-
Steroid Cream:
- For very itchy spots, use 1% hydrocortisone cream (such as Cortaid). No prescription is needed.
- Use up to 3 times per day as needed until the itching is better.
- Eventually, the moisturizing cream will be all that you need for treating dry skin.
-
Humidifier:
- If your winters are dry, protect your child's skin from the constant drying effect.
- Do this by running a room humidifier full time.
-
Preventing Dry Skin:
- Don't use soaps or bubble bath.
- Wash the hands with warm water. Use soap only if the hands are very dirty. Also, use soap for anything that won't come off with water.
- Don't use swimming pools or hot tubs. Reason: Pool chemicals are very drying.
- Run a humidifier in the winter if the air is dry.
- During cold weather, wear gloves outside. This helps prevent drying of the skin.
- Drink lots of fluids.
-
Call Your Doctor If:
- Dry skin lasts more than 2 weeks on treatment
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.
Ear - Congestion
Is this your child's symptom?
- Stuffy or plugged up feeling in the ear
- Crackling or popping noise in the ear
- Hearing is often muffled
- No ear pain, except with air-travel type
- Rare complaint before age 4 or 5 years
If NOT, try one of these:
Causes of Ear Congestion
- Common Cold. A viral infection of the nose is the most common cause. The nasal congestion also blocks the ear tube (eustachian tube). The ear tube normally keeps air in the middle ear.
- Ear Infection. Middle ear pus can also cause muffled hearing on that side. This commonly happens with an ear infection.
- Middle Ear Fluid. Fluid may remain in the middle ear after the infection is cleared up. It can last for months. The main symptoms are popping and crackling noises in the ear.
- Blowing the Nose. Blowing too hard can force secretions into the ear tube.
- Allergic Rhinitis. Hay fever is an allergic reaction to pollens. It causes nasal congestion, clear drainage and sneezing. It also can block the ear tube and back up secretions in the ear.
- Airplane Ear. If the ear tube is blocked, sudden increases in air pressure can cause the eardrum to stretch. The main symptom is ear pain. Sometimes, it just causes congestion. It usually starts when coming down for a landing. It can also occur during mountain driving.
When to Call for Ear - Congestion
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Self Care at Home
|
Call Doctor Within 24 Hours
- You think your child needs to be seen
- Earache
- Could be a foreign object in the ear canal
- Ear congestion lasts more than 48 hours
Call Doctor During Office Hours
- Could be blocked with ear wax
- You have other questions or concerns
Self Care at Home
- Ear congestion most likely from blocked ear tube
Care Advice for Ear Congestion
-
What You Should Know About Ear Congestion:
- Most often, this is from a blocked ear tube (eustachian tube). This tube normally drains the space behind the eardrum.
- It is usually not caused by an ear infection.
- Here is some care advice that should help.
-
Swallow and Chew More:
- Swallow water or other fluid while the nose is pinched closed. Reason: Makes a vacuum in the nose that helps the ear tube open up.
- After age 6, can also use chewing gum.
-
Decongestant Nose Spray (Age 12 years or Older):
- If chewing doesn't help after 1 or 2 hours, use a long-acting decongestant nose spray. An example is Afrin.
- Dose: 1 spay per side, 2 times per day as needed.
- Don't use for more than 3 days. Reason: Can cause rebound swelling in the nose.
- Decongestants given by mouth (such as Sudafed) are another choice. They can also open a stuffy nose and ears. Side effects: They may make a person feel nervous or dizzy. Follow the package directions.
-
Allergy Medicines:
- Nose allergies can cause ear stuffiness.
- If your child has hay fever or other allergies, give an allergy medicine. An example is Benadryl.
- See the Nose Allergy care guide for other advice.
-
What to Expect:
- The symptoms most often clear within 2 days (48 hours) with treatment.
- It's safe for your child to swim or fly.
-
Prevention During Air or Mountain Travel:
- It's safe to fly when your child has a cold.
- Most symptoms happen when the airplane is coming down in altitude. This is the descent of the plane during the 15 minutes before landing.
- Keep your child awake during takeoff and descent.
- Swallow during descent using fluids or a pacifier.
- Age over 6: Can chew gum during descent.
- Yawning during descent also can open the middle ear.
- Drink lots of fluids throughout the flight. This will prevent the nasal secretions from drying out.
-
Call Your Doctor If:
- Ear pain occurs
- Ear congestion lasts more than 48 hours
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.
Ear - Discharge
Is this your child's symptom?
- Drainage of substance or liquid from the ear canal
- Drainage through an ear tube is included
If NOT, try one of these:
Types of Ear Discharge
- Pus or Cloudy Fluid. This is the most common type of ear discharge. The main cause is an ear infection. The drainage is from a torn eardrum. The eardrum ruptures in about 10% of bacterial ear infections.
- Ear Tube Fluid Release. Children with frequent ear infections may get ventilation tubes put in. These help the middle ear drain its fluids and become dry. Sometimes, the ear tube gets plugged up. Normal fluids build up in the middle ear until the ear tube opens up again. This can cause some clear fluid drainage from the ear canal for a day.
- Earwax. Earwax is light brown, dark brown, or orange brown in color. If it gets wet, it can look like a discharge.
- Blood. This follows an injury to the ear. Usually, it's just a minor scratch of the lining of the ear canal.
- Water. Bath water or tears can get in the ear canal. Seeing a clear "discharge" that happens once is likely this.
- Ear Drops. The person who sees the discharge may not know someone else put in drops.
- Swimmer's Ear Discharge. Early symptoms are an itchy ear canal. Later symptoms include a whitish, watery discharge. Mainly occurs in swimmers and in the summer time.
- Ear Canal Foreign Object. Young children may put small objects in their ear canal. It can cause a low grade infection and pus colored discharge. If the object was sharp, the discharge may have streaks of blood.
When to Call for Ear - Discharge
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Self Care at Home
|
Call Doctor or Seek Care Now
- Pink or red swelling behind the ear
- Clear or bloody fluid after a head injury
- Bleeding from the ear canal. Exception: few drops and after an ear exam.
- Age less than 12 weeks old with fever. Caution: do NOT give your baby any fever medicine before being seen.
- Fever over 104° F (40° C)
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Call Doctor Within 24 Hours
- Age less than 6 months old
- Ear pain or crying like in pain
- Discharge is yellow or green, cloudy white or smells bad
- Clear drainage (not from a head injury) lasts more than 24 hours
- You think your child needs to be seen, but the problem is not urgent
Call Doctor During Office Hours
- You have other questions or concerns
Self Care at Home
- Normal earwax or other harmless discharge
Care Advice for Ear Discharge
-
Earwax:
- Ear wax protects the lining of the ear canal and has germ-killing properties.
- If the earwax is removed, the ear canals become itchy.
- Do not use cotton swabs (Q-tips) in your child's ear.
- Call Your Doctor If: Begins to look like pus (yellow or green discharge).
-
Clear Discharge (without head injury):
- Most likely, this is from tears or water that entered the ear canal. This can happen during a bath, shower, swimming or water fight.
- Don't overlook eardrops your child or someone else used without telling you.
- In children with ventilation tubes, some clear or slightly cloudy fluid can occur. This happens when a tube blockage opens up and drains.
- Call Your Doctor If: Clear drainage lasts for more than 24 hours.
-
Blood After Ear Exam:
- Sometimes, ear wax needs to be removed by your doctor to see the eardrum. If ear wax was removed, it can cause a small scratch inside the ear canal. This happens about 10% of the time. The scratch oozes 1 or 2 drops of blood and then clots.
- This should heal up in a few days.
- It shouldn't affect the hearing.
- Don't put anything in the ear canal. This may start the bleeding again.
- Call Your Doctor If: Bleeding starts again.
-
Cloudy Discharge - Ear Infection:
- Cloudy fluid or pus draining from the ear canal usually means there's an ear infection.
- The pus drains because there's a small tear in the eardrum.
- To help with the pain, give an acetaminophen product (such as Tylenol). Another choice is an ibuprofen product (such as Advil). Use as needed.
- See Earache care guide for more advice.
- Call Your Doctor If: Your child becomes worse.
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.
Ear - Pulling At or Rubbing
Is this your child's symptom?
- A child who pulls, tugs, pokes, rubs or itches the ear
- No crying or report of ear pain
If NOT, try one of these:
Causes of Ear Pulling
- Habit. Main cause in infants. Normal touching and pulling with discovery of ears. This is usually not seen before 4 months of age. Usually not seen after 12 months old. By then, they have more interesting things to do.
- Earwax. The main cause in older children is a piece of earwax. This earwax buildup is usually caused by putting cotton swabs in the ear canal. Until the teen years, cotton swabs are wider than the ear canal. Therefore, they just push the earwax back in.
- Soap. Another cause of an itchy ear canal is soap or other irritants. Soap or shampoo can get trapped in the ear canal after showers.
- Ear Infection. Children with ear infections act sick. They present with an earache or unexplained crying.
- Rubbing the ear is common in younger children (under age 2 or 3). Simple ear pulling without other symptoms such as fever or crying is harmless. These children rarely have an ear infection.
When to Call for Ear - Pulling At or Rubbing
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Self Care at Home
|
Call Doctor or Seek Care Now
- Fever over 104° F (40° C)
- Age less than 12 weeks old with fever. Caution: do NOT give your baby any fever medicine before being seen.
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Call Doctor Within 24 Hours
- Seems to be in pain (or is crying)
- Starts to wake up from sleep
- Fever or symptoms of a cold are present
- Drainage from the ear canal
- Frequent digging inside 1 ear canal
- You think your child needs to be seen, but the problem is not urgent
Call Doctor During Office Hours
- Pulling at or rubbing the ear lasts more than 3 days
- Itching lasts more than 1 week
- You have other questions or concerns
Self Care at Home
- Normal ear touching or pulling
- Itchy ear canal
Care Advice for Ear Rubbing or Itchy Ear Canal
-
What You Should Know About Ear Rubbing:
- Most infants have discovered their ears and are playing with them.
- Some have an itchy ear canal.
- Earwax buildup is the most common cause. Most wax problems are caused by putting cotton swabs in the ear canal.
- Ear pulling can start when your child has a cold. It can be caused by fluid in the middle ear. Less often, it's caused by an ear infection. If this is the case, your child will develop other symptoms. Look for fever or increased crying.
- Ear pulling without other symptoms is not a sign of an ear infection.
- Here is some care advice that should help.
-
Habit Type of Ear Rubbing:
- If touching the ear is a new habit, ignore it.
- This helps prevent your child from doing it for attention.
-
Cotton Swabs - Do Not Use:
- Cotton swabs can push earwax back and cause a plug.
- Earwax has a purpose. It protects the lining of the ear canal.
- Earwax also comes out on its own.
- Q-tips should never be used before the teen years. Reason: They are wider than the ear canal.
-
Keep Soap Out of the Ears:
- Keep soap and shampoo out of the ear canal.
- Reason: Makes the ears itchy.
-
White Vinegar Eardrops:
- For an itchy ear canal, you can use half-strength white vinegar. Make this by mixing the vinegar with equal parts warm water.
- Place 2 drops in each ear canal once daily.
- Do this for three days.
- Reason: Restores the normal acid pH.
- Caution: Do not use eardrops if your child has ear drainage or ear tubes. Also, do not use if your child has a hole in eardrum.
-
What to Expect:
- With this treatment, most itching is gone in 2 or 3 days.
-
Call Your Doctor If:
- Rubbing the ear lasts more than 3 days
- Itching of ear lasts more than 1 week
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.
Ear Infection Questions
Is this your child's symptom?
- Your child was diagnosed with an ear infection
- Your child's ears were recently looked at by a doctor
- You are worried that the fever or ear pain is not getting better fast enough
- Your child is still taking an antibiotic for the ear infection
If NOT, try one of these:
Symptoms of Ear Infections
- The main symptom is an earache.
- Younger children will cry, act fussy or have trouble sleeping because of pain.
- About 50% of children with an ear infection will have a fever.
- Complication: In 5% to 10% of children, the eardrum will develop a small tear. This is from the pressure in the middle ear. The ear then drains cloudy fluid or pus. This small hole most often heals over in 2 or 3 days.
Cause of Ear Infections
- A bacterial infection of the middle ear (the space behind the eardrum)
- Blocked eustachian tube, usually as part of a common cold. The eustachian tube joins the middle ear to the back of the throat.
- Blockage results in middle ear fluid (called viral otitis).
- If the fluid becomes infected (bacterial otitis), the fluid turns to pus. This causes the eardrum to bulge out and can cause a lot of pain.
- Ear infections peak at age 6 months to 2 years. They are a common problem until age 8.
- The onset of ear infections is often on day 3 of a cold.
- How often do kids get ear infections? 90% of children have at least 1 ear infection. Frequent ear infections occur in 20% of children. Ear infections are the most common bacterial infection of young children.
When to Call for Ear Infection Questions
Call 911 Now
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Self Care at Home
|
Call 911 Now
- Not moving or too weak to stand
- You think your child has a life-threatening emergency
Call Doctor or Seek Care Now
- Stiff neck (can't touch chin to the chest)
- Walking is not steady
- Fever over 104° F (40° C)
- Ear pain is severe and not better 2 hours after taking ibuprofen
- Crying is bad and not better 2 hours after taking ibuprofen
- Pink or red swelling behind the ear
- Crooked smile (weakness of 1 side of the face)
- New vomiting
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Call Doctor Within 24 Hours
- Taking antibiotic more than 48 hours and fever still there or comes back
- Taking antibiotic more than 3 days and ear pain not better
- Taking antibiotic more than 3 days and ear discharge still there or comes back
- You think your child needs to be seen, but the problem is not urgent
Call Doctor During Office Hours
- You have other questions or concerns
Self Care at Home
- Ear infection on antibiotic with no other problems
- Normal hearing loss with an ear infection
- Prevention of ear infections
- Ear tube (ventilation tube) surgery questions
Care Advice
Treatment for an Ear Infection
-
What You Should Know About Ear Infections:
- Ear infections are very common in young children.
- Most ear infections are not cured after the first dose of antibiotic.
- Often, children don't get better the first day.
- Most children get better slowly over 2 to 3 days.
- Note: For mild ear infections in older children, antibiotics may not be needed. This is an option if over 2 years old and infection looks viral.
- Here is some care advice that should help.
-
Keep Giving the Antibiotic:
- The antibiotic will kill the bacteria that are causing the ear infection.
- Try not to forget any of the doses.
- Give the antibiotic until it is gone. Reason: To stop the ear infection from flaring up again.
-
Fever Medicine:
- For fevers above 102° F (39° C), give an acetaminophen product (such as Tylenol).
- Another choice is an ibuprofen product (such as Advil).
- Note: Fevers less than 102° F (39° C) are important for fighting infections.
- For all fevers: Keep your child well hydrated. Give lots of cold fluids.
-
Pain Medicine:
- To help with the pain, give an acetaminophen product (such as Tylenol).
- Another choice is an ibuprofen product (such as Advil).
- Use as needed.
-
Cold Pack for Pain:
- Put a cold wet washcloth on the outer ear for 20 minutes. This should help the pain until the pain medicine starts to work.
- Note: Some children prefer heat for 20 minutes.
- Caution: Heat or cold kept on too long could cause a burn or frostbite.
-
Limits on Activity:
- Your child can go outside and does not need to cover the ears.
- Swimming is fine as long as there is no drainage from the ear. Also, do not swim if there is a tear in the eardrum.
- Air Travel. Children with ear infections can travel safely by aircraft if they are taking antibiotics. For most, flying will not make their ear pain worse.
- Give your child a dose of ibuprofen 1 hour before take-off. This will help with any pain they might have. Also, during descent (coming down for landing) have your child swallow fluids. Sucking on a pacifier may help as well. Children over age 6 can chew gum.
-
Return to School:
- Your child can go back to school when any fever is gone.
- Your child should feel well enough to join in normal activities.
- Ear infections cannot be spread to others.
-
What to Expect:
- Once on antibiotics, your child will get better in 2 or 3 days.
- Make sure you give your child the antibiotic as directed.
- The fever should be gone by 2 days (48 hours).
- The ear pain should be better by 2 days. It should be gone by 3 days (72 hours).
-
Ear Infection Discharge:
- If pus is draining from the ear, the eardrum probably has a small tear. This can be normal with an ear infection. Discharge can also occur if your child has ear tubes.
- The pus may be blood-tinged.
- Most often, this heals well after the ear infection is treated.
- Wipe the discharge away as you see it.
- Do not plug the ear canal with cotton. (Reason: Retained pus can cause an infection of the lining of the ear canal)
-
Call Your Doctor If:
- Fever lasts more than 2 days on antibiotics
- Ear pain becomes severe or crying becomes nonstop
- Ear pain lasts more than 3 days on antibiotics
- Ear discharge is not better after 3 days on antibiotics
- You think your child needs to be seen
- Your child becomes worse
Treatment for Hearing Loss with an Ear Infection
-
Brief Hearing Loss:
- During an ear infection, fluid builds up in the middle ear space.
- The fluid can cause a mild hearing loss for a short time.
- It will slowly get better and go away with the antibiotic.
- The fluid is no longer infected, but sometimes, may take weeks to go away. In 90% of children, it clears up by itself over 1 to 2 months.
- Permanent harm to the hearing is very rare.
-
Talking With Your Child:
- Get close to your child and get eye contact.
- Speak in a louder voice than you usually use.
- Decrease any background noise from radio or TV while talking with your child.
-
Call Your Doctor If:
- Hearing loss not better after the antibiotic is done.
Prevention of Recurrent Ear Infections
-
What You Should Know:
- Some children have ear infections that keep coming back.
- If this is your child's case, here are some ways to prevent future ones.
-
Avoid Tobacco Smoke:
- Contact with tobacco smoke can lead to ear infections.
- It also makes them harder to treat.
- No one should smoke around your child. This includes in your home, your car or at child care.
-
Avoid Colds:
- Most ear infections start with a cold. During the first year of life, try to reduce contact with other sick children.
- Try to put off using a large child care center during the first year. Instead, try using a sitter in your home. Another option might be a small home-based child care.
-
Breastfeed:
- Breastfeed your baby during the first 6 to 12 months of life.
- Antibodies in breast milk lower the rate of ear infections.
- If you breastfeed, continue it.
- If you do not, think about it with your next child.
-
Do Not Prop the Bottle:
- During feedings, hold your baby with the head higher than the stomach.
- Feeding while lying down flat can lead to ear infections. It causes formula to flow back into the middle ear.
- Having babies hold their own bottle also causes milk to drain into the middle ear.
-
Get All Suggested Vaccines:
- Vaccines protect your child from serious infections.
- The pneumococcal and flu shots also help to prevent some ear infections.
-
Control Allergies:
- Allergies may lead to some ear infections.
- If your baby has a constant runny or blocked nose, suspect an allergy.
- If your child has other allergies like eczema, ask your child's doctor about this. The doctor can check for a milk protein or soy protein allergy.
-
Check Any Snoring:
- Large adenoids can cause snoring or mouth breathing. Suspect this if your toddler snores every night or breathes through his mouth.
- Large adenoids can contribute to ear infections.
- Talk to your child's doctor about this.
Ear Tube Surgery Questions
-
Ear Tubes:
- Ear tubes are tiny plastic tubes that are put through the eardrum. They are placed by an ENT doctor.
- The tubes allow fluid to drain out of the middle ear space. They also allow air to re-enter the space.
- This lowers the risk of repeated ear infections and returns the hearing to normal.
-
Ear Tubes - When Are They Needed?
- Fluid has been present in the middle ear nonstop for over 4 months. Both ears have fluid.
- Also, the fluid has caused a hearing loss greater than 20 decibels.
- Hearing should be tested first. Some children have nearly normal hearing and tubes are not needed.
- Ear infections that do not clear up after trying many antibiotics may need tubes.
- Prevention should be tried before turning to surgery.
- Talk to your child's doctor about when ear tubes are needed.
-
What to Expect:
- In most cases, the tubes come out after about a year. They fall out of the ear on their own. This happens with the normal movement of earwax.
- If the tubes stay in over 2 years, talk with your child's doctor. The surgeon may need to take them out.
-
Risks of Ear Tubes:
- After the tubes come out, they may leave scars on the eardrum. They may also leave a small hole that doesn't heal. Both of these problems can cause a small hearing loss.
- Because of these possible problems, there is a small risk with ear tubes. There is also a small risk when giving anesthesia to young children.
- Therefore, doctors suggest ear tubes only for children who really need them.
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.
Ear Injury
Is this your child's symptom?
- Injuries to the outer ear, ear canal or eardrum
Types of Ear Injuries
- Cut or Scratch. Most cuts of the outer ear do not need sutures.
- Bruise. Most bruises of the outer ear just leave a purple mark. They heal on their own.
- Blood Clot (Serious). Most of the outer ear is made of cartilage. A large blood clot (hematoma) can cut off the blood supply to the cartilage. It needs to be drained. If not, the ear may become deformed (boxer's ear).
- Ear Canal Bleeding. Most are due to a scratch of ear canal. This can be caused by cotton swab, fingernail, or ear exam. Most stop bleeding on their own. Persistent bleeding needs to be seen.
- Punctured Eardrum. Most are due to long-pointed objects put in the ear canal. Examples are cotton swabs, pencils, sticks, straws, or wires.
- Loss of Hearing (Serious). Caused by blunt trauma, such as a slap to the ear. Also, caused by explosions.
When to Call for Ear Injury
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Self Care at Home
|
Call Doctor or Seek Care Now
- Skin is split open or gaping and may need stitches
- Upper part of the ear is very swollen
- Pointed object was put into the ear canal (such as a pencil, stick, or wire)
- Clear fluid is draining from the ear canal
- Walking is not steady
- Severe pain and not better 2 hours after taking pain medicine
- Age less than 1 year old
- You think your child has a serious injury
- You think your child needs to be seen, and the problem is urgent
Call Doctor Within 24 Hours
- Few drops of blood in the ear canal. Caused by a minor injury, cotton swab (Q-tip) or ear exam.
- Injury causes an earache or crying lasts more than 30 minutes
- Hearing is less on injured side
- You think your child needs to be seen, but the problem is not urgent
Call Doctor During Office Hours
- Dirty cut and no tetanus shot in more than 5 years
- Clean cut and no tetanus shot in more than 10 years
- You have other questions or concerns
Self Care at Home
- Minor ear injury
Care Advice for Minor Ear Injuries
-
Bleeding - How To Stop:
- For any bleeding, put direct pressure on the wound.
- Use a gauze pad or clean cloth.
- Press for 10 minutes or until the bleeding has stopped.
-
Clean the Wound:
- Wash the wound with soap and water for 5 minutes.
-
Antibiotic Ointment:
- For cuts and scrapes, use an antibiotic ointment (such as Polysporin). No prescription is needed.
- Put it on the cut 3 times a day.
- Do this for 3 days.
- Cover large scrapes with a bandage (such as Band-Aid). Change daily.
-
Pain Medicine:
- To help with the pain, give an acetaminophen product (such as Tylenol).
- Another choice is an ibuprofen product (such as Advil).
- Use as needed.
-
What to Expect:
- Minor ear wounds heal quickly.
- Most often, cuts and scrapes heal in 2 or 3 days.
-
Call Your Doctor If:
- Pain gets severe
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.
Earache
Is this your child's symptom?
- Pain in or around the ear
- The older child complains about ear pain
- Younger child acts like he did with last ear infection or cries a lot
- Not caused by an ear injury
If NOT, try one of these:
Causes of Earaches
- Ear Infection. An infection of the middle ear (space behind the eardrum) is the most common cause. Ear infections can be caused by viruses or bacteria. Usually, a doctor can tell the difference by looking at the eardrum.
- Swimmer's Ear. An infection or irritation of the skin that lines the ear canal. Main symptom is itchy ear canal. If the canal becomes infected, it also becomes painful. Mainly occurs in swimmers and in the summer time.
- Ear Canal Injury. A cotton swab or fingernail can cause a scrape in the canal.
- Ear Canal Abscess. An infection of a hair follicle in the ear canal can be very painful. It looks like a small red bump. Sometimes, it turns into a pimple. It needs to be drained.
- Earwax. A big piece of hard earwax can cause mild ear pain. If the wax has been pushed in by cotton swabs, the ear canal can become blocked. This pain will be worse.
- Ear Canal Foreign Object. Young children may put small objects in their ear canal. It will cause pain if object is sharp or pushed in very far.
- Airplane Ear. If the ear tube is blocked, sudden increases in air pressure can cause the eardrum to stretch. The main symptom is severe ear pain. It usually starts when coming down for a landing. It can also occur during mountain driving.
- Pierced Ear Infections. These are common. If not treated early, they can become very painful.
- Referred Pain. Ear pain can also be referred from diseases not in the ear. Tonsil infections are a common example. Tooth decay in a back molar can seem like ear pain. Mumps can be reported as ear pain. Reason: the mumps parotid gland is in front of the ear. Jaw pain (TMJ syndrome) can masquerade as ear pain.
Ear Infections: Most Common Cause
- Definition. An infection of the middle ear (the space behind the eardrum). Viral ear infections are more common that bacterial ones.
- Symptoms. The main symptom is an earache. Younger children will cry, act fussy or have trouble sleeping because of pain. About 50% of children with an ear infection will have a fever.
- Diagnosis. A doctor can diagnose a bacterial ear infection by looking at the eardrum. It will be bulging and have pus behind it. For viral ear infections, the eardrum will be red but not bulging.
- Age Range. Ear infections peak at age 6 months to 2 years. They are a common problem until age 8. The onset of ear infections is often on day 3 of a cold.
- Frequency. 90% of children have at least 1 ear infection. Frequent ear infections occur in 20% of children. Ear infections are the most common bacterial infection of young children.
- Complication of Bacterial Ear Infections. In 5% to 10% of children, the eardrum will develop a small tear. This is from the pressure in the middle ear. The ear then drains cloudy fluid or pus. This small hole most often heals over in 2 or 3 days.
- Treatment. Bacterial ear infections need an oral antibiotic. Viral ear infections get better on their own. They need pain medicine and supportive care.
When to Call for Earache
Call 911 Now
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
|
Call 911 Now
- Not moving or too weak to stand
- You think your child has a life-threatening emergency
Call Doctor or Seek Care Now
- Severe earache and not improved 2 hours after taking ibuprofen
- Pink or red swelling behind the ear
- Outer ear is red, swollen and painful
- Stiff neck (can't touch chin to the chest)
- Walking is not steady
- Pointed object was put into the ear canal (such as a pencil, stick, or wire)
- Not alert when awake ("out of it")
- Weak immune system. Examples are: sickle cell disease, HIV, cancer, organ transplant, taking oral steroids.
- Fever over 104° F (40° C)
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Call Doctor Within 24 Hours
- Earache, but none of the symptoms above. Reason: could be an ear infection.
- Pus or cloudy discharge from ear canal
Care Advice for Earache
-
What You Should Know About Earaches:
- Your child may have an ear infection. The only way to be sure is to look at the eardrum.
- It is safe to wait until your doctor's office is open to call. It is not harmful to wait if the pain starts at night.
- Ear pain can usually be controlled with pain medicine.
- Many earaches are caused by a virus and don't need an antibiotic.
- Here is some care advice that should help until you talk with your doctor.
-
Pain Medicine:
- To help with the pain, give an acetaminophen product (such as Tylenol).
- Another choice is an ibuprofen product (such as Advil).
- Use as needed.
-
Cold Pack for Pain:
- Put a cold wet washcloth on the outer ear for 20 minutes. This should help the pain until the pain medicine starts to work.
- Note: Some children prefer heat for 20 minutes.
- Caution: Heat or cold kept on too long could cause a burn or frostbite.
-
Ear Infection Discharge:
- If pus is draining from the ear, the eardrum probably has a small tear. Usually, this is from an ear infection. Discharge can also occur if your child has ear tubes.
- The pus may be blood-tinged.
- Most often, this heals well after the ear infection is treated.
- Wipe the discharge away as you see it.
- Do not plug the ear canal with cotton. (Reason: Retained pus can cause an infection of the lining of the ear canal)
-
Fever Medicine:
- For fevers above 102° F (39° C), give an acetaminophen product (such as Tylenol).
- Another choice is an ibuprofen product (such as Advil).
- Note: fevers less than 102° F (39° C) are important for fighting infections.
- For all fevers: Keep your child well hydrated. Give lots of cold fluids.
-
Return to School:
- Ear infections cannot be spread to others.
- Can return to school or child care when the fever is gone.
-
Call Your Doctor If:
- Pain becomes severe
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.
Earwax Buildup
Is this your child's symptom?
- Earwax (cerumen) buildup or blockage
- Questions about earwax removal
If NOT, try one of these:
Symptoms of Earwax Buildup
- Too much earwax can cause rubbing of the ear or poking in the canal.
- A piece of ear wax can become dry and hard in the ear canal. This creates a feeling that an object is in the ear.
- Complete blockage (plugging) of the ear canal by wax causes more symptoms. These include decreased or muffled hearing.
- A large piece of earwax may be seen inside the ear canal.
Causes of Earwax Buildup
- Cotton Swabs. Earwax buildup is usually from using cotton swabs. They push the wax back in and pack it down.
- Fingers. A few children (perhaps 5%) normally produce more wax than others. It usually will come out if it's not pushed back by fingers.
- Ear Plugs. Wearing ear plugs of any type can also push wax back.
Earwax is Normal
- Everyone has earwax. Earwax is normal and healthy. Earwax is not dirty or a sign of poor hygiene.
- Earwax is also called cerumen.
- Earwax is made by special glands in the outer third of the ear canal.
- Earwax has a purpose. It protects the skin lining the ear canal. It is a natural water-proofing agent.
- Earwax also has germ-killing properties.
- New earwax is soft and a golden-yellow color.
- Older earwax becomes dryer and turns to a brown or black color.
Ear Canals are Self-Cleaning
- Ear canals are designed to clean themselves.
- The ear canal skin slowly moves out of the ear canal. It carries the earwax along with it. The wax dries up and becomes flaky. It falls out of the ear on its own.
- There are some people who produce much more earwax than others. For such people periodic ear cleaning may be needed.
- Earwax only needs to be removed from inside the ear if it causes symptoms. Examples of symptoms are decreased hearing, discomfort, fullness or blockage.
Problems From Using Cotton-Tipped Swabs
- The cotton-tipped swab pushes the wax back in. The earwax builds up and causes symptoms.
- Decreased or muffled hearing.
- Blocked or full ear canal sensation.
- Trapped water behind the wax (can lead to Swimmer's Ear).
- Itchy or painful canals, especially in teens who often use Q-tips. A dry ear canal is always itchy.
- Sometimes, bleeding or damage to the eardrum.
Prevention of Blocked Ear Canals
- Never put cotton swabs (cotton buds or Q-tips) into the ear canal.
- Cotton swabs just push the earwax deeper into the ear canal. Reason: Cotton swabs are usually wider than a child's ear canal.
- Earwax doesn't need any help getting out. You can't hurry the process.
- Never try to dig out pieces of earwax with toothpicks, match sticks or other devices. Usually, doing this just pushes the wax back in.
- These objects can also scratch the ear canal and cause an infection.
- If all of the ear wax is removed (as with cotton swabs), the ear canals become itchy. They also become more prone to swimmer's ear. This can occur in teens when cotton swabs are smaller than the ear canal.
- Limit the use of ear plugs.
When to Call for Earwax Buildup
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Self Care at Home
|
Call Doctor or Seek Care Now
- Ear pain or bleeding after object (such as cotton swab) was inserted into ear canal
- Ear pain after ear canal flushing to remove wax and it's severe
- Walking is very unsteady
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Call Doctor Within 24 Hours
- Ear pain after ear canal flushing and it lasts more than 1 hour
- Pus (yellow or green discharge) from the ear canal
- You think your child needs to be seen, but the problem is not urgent
Call Doctor During Office Hours
- History of ear drum perforation, tubes or ear surgery. Reason: don't remove wax at home.
- Complete hearing loss in either ear
- Age less than 6 years with earwax problems
- Earwax problems not better after using Care Advice
- You don't want to try to remove earwax at home
- You have other questions or concerns
Self Care at Home
- Questions about earwax removal
Care Advice for Earwax Buildup
-
What You Should Know About Earwax Buildup:
- Earwax is good.
- In general, leave earwax alone.
- It will come out and fall away on its own.
- If you see some wax right at the opening, you can flick it away. Use something that won't push it back in, such as a paper clip.
-
Reasons to Flush out the Ear Canal:
- Earwax is completely blocking an ear canal and can't hear on that side.
- If the hearing seems normal on that side, the blockage is only partial. You can leave it alone.
-
Age 6 Years and Older - Ear Canal Flushing with Water:
- Under age 6, use only if advised by your child's doctor.
- Buy a soft rubber ear syringe or bulb from the pharmacy. No prescription is needed.
- Have your child lean over the sink. Reason: To catch the water.
- Use lukewarm water (body temperature). Reason: To prevent dizziness.
- Gently squirt the water into the ear canal. Then tilt your child's head and let the water run out. You may need to do this several (3-4) times.
- If the earwax does not seem to be coming out, tilt the head. Then, flush it with the head tilted. Have the ear with the wax in it facing downward. Gravity will help the water wash it out (the waterfall effect).
- Endpoint: Flush until the water that comes out is clear of wax. Also, the ear canal should be open when you look in with a light.
- Afterwards dry the ear thoroughly. You can do this by putting a drop of rubbing alcohol in the ear canal. Or you can set a hair dryer on low. Hold it a foot away from the ear for 10 seconds.
-
Caution - Ear Canal Flushing:
- Do not perform flushing if your child has a hole in the eardrum or ear tubes.
- Stop flushing if it causes pain or dizziness.
- Do not use a water jet tooth cleaner (such as a WaterPik) for ear flushing. Reason: The force of the jet can cause pain.
-
Ear Drops - Use for 4 Days to Soften the Earwax:
- If the earwax is hard, soften it before flushing the ear canal. Use ear drops to break up the earwax.
- Homemade ear drops: 15% baking soda solution. Make it by adding ¼ teaspoon (1.25 mL) of baking soda to 2 teaspoons (10 mL) of water.
- Other option for homemade ear drops: hydrogen peroxide and water solution. Mix equal parts of each.
- Drug store option: Earwax removal ear drops (such as Debrox). No prescription is needed.
- Use 5 drops in affected ear, 2 times daily, for 4 days.
-
How to Put in Ear Drops:
- Lie on the side with blocked ear upward.
- Place 5 drops into ear canal.
- Keep drops in ear for 10 minutes by continuing to lie down.
- Then lie with the blocked side down. Let the ear drops run out onto some tissue.
- Use twice daily for up to four days.
- Then flushing should be able to get everything out.
-
Cautions for Ear Drops:
- Do not use ear drops if your child has a hole in the eardrum. Also do not use them for children with ear tubes.
- Stop using ear drops if pain occurs.
-
Earwax Removal Before 6 Years Old:
- Earwax removal in this age group can be hard.
- Removal may not be needed. The ear wax should come out on its own. Don't use cotton swabs.
- Do not use eardrops or ear flushes unless it is advised by your child's doctor. This also can be done in your doctor's office.
-
Call Your Doctor If:
- Flushing out the ear canal doesn't return the hearing to normal
- Earache occurs
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.
Ebola Exposure
Is this your child's symptom?
- You or your child were exposed to someone diagnosed with Ebola
- You traveled to or are living in an area with recent cases of Ebola. In 2014, a large Ebola outbreak occurred in West Africa.
- You have questions about Ebola
- Ebola Exposure means:
- Touching a person diagnosed with Ebola. Examples include kissing, hugging, or holding hands. Another example is sharing eating or drinking utensils.
- Contact with blood or body fluids of a person with suspected or proven Ebola.
- Handling bats, monkeys or other wild animals from areas where Ebola occurs.
If NOT, try one of these:
Ebola Facts
- Ebola is an infection caused by the Ebola virus.
- The infection is spread human-to-human. The first cases may have come from contact with infected bats or monkeys.
- It is a rare disease, but the death rate can be 50% in poor countries. The death rate in US hospitals is about 10%.
- There have been small outbreaks in Africa since 1976.
- In 2014, a major outbreak of Ebola started in Guinea in West Africa.
- On September 30, 2014, the CDC reported the first case of Ebola in the United States. The patient caught Ebola in Liberia. He came down with his first symptoms in Dallas, Texas.
Symptoms of Ebola
Symptoms show up 2 to 21 days after being exposed to Ebola. The average is 8-10 days. Symptoms are:
- Fever. Fever is usually the first symptom.
- Stomach pain, vomiting or diarrhea.
- Severe headache, weakness or muscle pain.
- Bleeding and bruising are late symptoms.
How Ebola is Spread
- People with Ebola do not spread the disease until they become sick. Infected people are safe to be with during the incubation period. This is the time between exposure and the time a person gets symptoms.
- Ebola patients who have a fever and feel sick can spread the disease. During the first few days of symptoms, it is not very contagious. Most people living in the same home do not catch Ebola. The attack rate for adults is 30%. The attack rate for children is 5%.
- The Ebola virus can be spread in several ways:
- Blood or body fluids of a person sick with Ebola can spread this illness. Body fluids include spit, urine, vomit, stool, sweat, semen and breast milk. Touching a dead body of an Ebola victim can also transmit the disease.
- Dirty objects with blood or body fluids on them can spread the disease. Examples are dirty clothing, bedding or needles.
- Infected animals (e.g., bats and monkeys) can also spread the disease.
- Mucous membrane contact. Ebola can start if infected fluid gets into the eyes, nose or mouth. This mainly happens if infected fluid gets on the hands. Then, the healthy person then touches their face with dirty hands. Washing the hands often is helpful.
- Skin contact. The virus in blood or body fluids may pass through an open cut. Normal skin is safe if the body fluid is carefully washed off.
- Ebola is not spread in the food supply, tap water or the air. It also is not spread by mosquitoes or other insects.
Countries with Ebola Outbreaks
- Most Ebola patients have been linked to countries in West Africa. These patients have either lived in or traveled to countries there. These countries include Guinea, Liberia, and Sierra Leone. The risk of getting the illness is highest in countries that have outbreaks now.
- Caregivers and close contacts of Ebola patients can also get the disease.
- But, for most people, your risk of getting Ebola remains very low.
When to Call for Ebola Exposure
Call 911 Now
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Self Care at Home
|
Call 911 Now
- You think your child has a life-threatening emergency
Call Doctor or Seek Care Now
- Any unusual symptoms within 21 days of Ebola Exposure
- You think your child needs to be seen, and the problem is urgent
Call Doctor Within 24 Hours
- Exposure to Ebola in the past 21 days and NO fever or other symptoms
- You think your child needs to be seen, but the problem is not urgent
Call Doctor During Office Hours
- You have other questions or concerns
Self Care at Home
- Exposure to Ebola more than 21 days ago and NO fever or other symptoms
- Questions about Ebola
Care Advice
Ebola Exposure within Last 21 Days and Symptoms
-
What You Should Know About Ebola Infection:
- Your child was exposed to Ebola in the last 21 days and now has symptoms.
- Your child needs to be checked to see if they have Ebola.
-
Call the Nearest Emergency Room (ER) Now:
- Your child needs to be seen. Call the nearest ER or the Ebola hot line. Tell them your child's symptoms and that they were exposed to Ebola. This is a very important step! This way the ER will be ready to care for you and protect others.
- Not all hospitals are prepared to see possible Ebola patients. The ER will give you instructions on the best place to go. They may also send a special ambulance out to get your child.
- The ER is the best place to get testing and treatment.
- The ER is most prepared to prevent the spread of this infection to others.
-
Isolation Is Needed:
- Stay in your home until you talk with the ER or Ebola hot line.
- Do Not go to school or work.
- Do Not go to church, child care centers, shopping, or other public places.
- Avoid close contact with others (hugging, kissing). Do Not shake hands.
-
Protect Others from Body Fluids:
- Protect others from blood and other body fluids!
- Body fluids include spit, urine, vomit, stool, sweat, semen and breast milk.
- Cover any bleeding area with a towel or cloth.
- Other people should avoid contact with blood or body fluids. They should not touch you or your child. They should not handle your child's bedding or dirty clothes.
-
Fever Medicine:
- For fever above 102° F (39° C), can give an acetaminophen product (such as Tylenol).
- Vomiting: Avoid medicine until seen.
Ebola Exposure within Last 21 Days and No Symptoms
-
What You Should Know About Ebola Exposure:
- Your child was exposed to Ebola but doesn't have any symptoms.
- Since it's been less than 21 days, he is still at risk for getting Ebola. The infection starts within 21 days after the last exposure.
- You will need to watch for symptoms until 21 days have passed.
-
Call the Local Public Health Department (PHD) Right Away:
- Call the local PHD right away. Some cities may have an Ebola hot line for reporting.
- If you cannot contact the PHD, call your doctor.
- This is very important. This must be done to stop the spread of the disease.
-
Stay at Home:
- Stay at home until you talk with the public health department or your doctor.
- They will tell you how much isolation is needed during the 21 days.
- Check your temperature two times a day.
- Report any fever or symptoms to the health care provider following you.
-
Call the Nearest Emergency Room (ER) Later If:
- Fever occurs within 21 days of Ebola exposure
- Stomach pain, diarrhea, or vomiting occurs within 21 days of Ebola exposure
- Headache or cough occurs within 21 days of Ebola exposure
- Unexplained bruising or bleeding occurs within 21 days of Ebola exposure
- Important Note: You must phone the ER first before you go there. Tell them your child's symptoms and that they were exposed to Ebola. This is a very important step! This way the ER will be ready to care for you and protect others. Also, the ER may send a special ambulance out to get you.
-
Call Your Doctor If:
- Any unexplained symptoms occur within 21 days of Ebola exposure
- You have other questions or concerns
Ebola Exposure Over 21 Days Ago and No Symptoms
-
Reassurance:
- Symptoms should appear 2 to 21 days after being exposed to Ebola. The average is 8-10 days.
- Over 21 days have passed since your child was last exposed.
- Your child did not develop fever or other symptoms of Ebola.
- Therefore, your child should be safe from getting it.
-
Call Your Doctor If:
- Fever occurs
- You think your child needs to be seen
Ebola Questions
-
What You Should Know About Ebola:
- Ebola is an infection caused by the Ebola virus.
- It is a rare disease, but the death rate can be 50%. The death rate in US hospitals is about 10%.
- There have been small outbreaks in Africa since 1976.
- In 2014, a major outbreak of Ebola started in West Africa.
- On September 30, 2014, the CDC reported the first case of Ebola in the United States. The patient caught Ebola in Liberia. He came down with his first symptoms in Dallas, Texas.
-
Symptoms of Ebola:
- Symptoms show up 2 to 21 days after being exposed to Ebola. The average is 8-10 days. Symptoms are:
- Fever. Fever is usually the first symptom.
- Stomach pain, vomiting or diarrhea
- Severe headache, weakness or muscle pain
- Bleeding and bruising are late symptoms.
-
How Ebola is Spread:
- People with Ebola do not spread the disease until they become sick. Infected people are safe to be with during the incubation period. This is the time between exposure and the time a person gets symptoms.
- Ebola patients who have a fever and feel sick can spread the disease. During the first few days of symptoms, it is not very contagious. Most people living in the same home do not catch Ebola. The attack rate for adults is 30%. The attack rate for children is 5%.
- The virus can be spread in several ways:
- Blood or body fluids of a person sick with Ebola can spread this illness. Body fluids include spit, urine, vomit, stool, sweat, semen and breast milk. Touching a dead body of an Ebola victim can also transmit the disease.
- Dirty objects with blood or body fluids on them can spread the disease. Examples are dirty clothing, bedding or needles.
- Infected animals (e.g., bats and monkeys) can also spread the disease.
- Mucous membrane contact. Ebola can start if infected fluid gets into the eyes, nose or mouth. This mainly happens if infected fluid gets on the hands. Then, the healthy person then touches their face with dirty hands. Washing the hands often is helpful.
- Skin contact. The virus in blood or body fluids may pass through an open cut. Normal skin is safe if the body fluid is carefully washed off.
- Ebola is not spread in the food supply, tap water or the air. It also is not spread by mosquitoes or other insects.
-
Countries with Ebola Outbreaks:
- Most Ebola patients have been linked to countries in West Africa. These patients have either lived in or traveled to countries there. These countries include Guinea, Liberia, and Sierra Leone. The risk of getting the illness is highest in countries that have outbreaks now.
- Caregivers and close contacts of Ebola patients can also get the disease.
- But, for most people, your risk of getting Ebola remains very low.
- Countries where Ebola is occurring can change. The most current list of countries with Ebola outbreaks is on the CDC website. (www.cdc.gov)
-
Internet Resources:
- Look for Ebola pages on this website for more info: Centers for Disease Control (CDC): Ebola Virus Disease.
-
Call Your Doctor If:
- You have other questions
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.
Eczema
Is this your child's symptom?
- An itchy rash that your doctor told you was eczema
- Eczema is a chronic skin disease
- Recurrent flare-ups of severe itching occur
- The medical name for eczema is atopic dermatitis
If NOT, try one of these:
Symptoms of Eczema
- The main symptom is itching. If it doesn't itch, it's not eczema.
- With flare-ups (itching attacks), the rash becomes red or even raw and weepy.
- Onset: Average onset at 3 months old. Range: 1-6 months old. Usually begins by 2 years old.
- Location: Classic eczema starts on the cheeks at 1 to 6 months of age. It can spread to the rest of the face. In infants, the outer surfaces of the arms and legs also become involved.
- In older children, eczema is found in the joint creases. The elbows, wrists, and knees are the most common places.
- The rash is usually the same on both sides of the body.
Cause of Eczema
- A type of dry, sensitive skin that children inherit.
- Flare-ups are from skin contact with soap, shampoo, pollen or other irritating substances.
- About 30% of babies with severe eczema also have food allergies. The most common is cow's milk.
- Over 10% of children have eczema. It's the most common skin condition of the first 10 years.
Triggers of Eczema Flare-Ups
- Soaps. Never use bubble bath. It can cause a major flare-up.
- Pollens. Keep your child from lying on the grass during grass pollen season.
- Animals. Avoid any animals that make the rash worse.
- Foods. If certain foods cause severe itching (flares), avoid them.
- Wool. Avoid wool fibers and clothes made of other scratchy, rough materials.
- Dry Air. Use a humidifier if the air in your home is dry.
- Herpes Virus Infection (Serious). Keep your child away from anyone with fever blisters (cold sores). The herpes virus can cause a serious skin infection in children with eczema.
- Eczema is not caused by laundry soap you use to wash clothing.
Itching Scale
- Mild: doesn't interfere with normal activities
- Moderate: interferes with child care or school, sleep, or other normal activities
- Severe: constant itching that can't be controlled
Food Allergy and Eczema Flare-Ups
- Food allergies are a factor in 30% of young children with severe eczema. This factor is mainly seen in babies.
- The main allergic foods are cow's milk and eggs.
- The main symptoms are increased skin redness and itching. Some parents report these symptoms start during or soon after the feeding.
- The eczema becomes easier to control if you avoid the allergic food.
Diagnosing Food Allergy and Eczema Flare-Ups
- Your child's doctor may suggest the steps listed below:
- Remove the suspected food or foods from your child's diet for 2 weeks. The eczema should greatly improve.
- Then give your child that food when the eczema is under good control. This is called a "challenge."
- If the food is causing flare-ups, the eczema should become itchy and red. The flare-up should occur quickly within 2 hours of eating the food.
- If this occurs, avoid giving this food to your child. Talk to your child's doctor about the need for any food substitutes.
- If the eczema does not flare-up, your child isn't allergic to that food.
When to Call for Eczema
Call 911 Now
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Self Care at Home
|
Call 911 Now
- You think your child has a life-threatening emergency
Call Doctor or Seek Care Now
- Age less than 12 weeks old with fever. Caution: do NOT give your baby any fever medicine before being seen.
- Looks infected (spreading redness, pus, soft oozing scabs) and fever
- Many small blisters or punched-out sores occur
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Call Doctor Within 24 Hours
- Eczema is very painful to touch
- Looks infected but no fever
- Itching is severe after using steroid cream for more than 48 hours
- You think your child needs to be seen, but the problem is not urgent
Call Doctor During Office Hours
- Itching flare-ups occur often
- Eczema diagnosis was never confirmed by a doctor
- You have other questions or concerns
Self Care at Home
- Eczema with no other problems
- Questions about prevention of eczema flare-ups
Care Advice
Treatment for Eczema
-
What You Should Know About Eczema:
- Eczema is a chronic skin disease. So, you need to learn how to control it.
- Itching attacks (flare-ups) are to be expected.
- The goal is to treat all flare-ups quickly. Reason: To prevent skin damage.
- Here is some care advice that should help.
-
Treatment is Based on Severity of Eczema:
- Mild Eczema. Just need to use a moisturizing cream and to avoid flare-up triggers.
- Moderate Eczema. Also need to use a steroid cream and bedtime allergy medicine.
- Severe Eczema. Also may need antibiotics for a skin infection caused by Staph bacteria. This infection starts in open skin from severe itching.
-
Moisturizing Cream or Ointment for Dry Skin:
- All children with eczema have dry sensitive skin.
- The skin needs a moisturizing cream (such as Eucerin) Apply once or twice daily.
- Apply the cream after a 5 or 10-minute bath. To trap moisture in the skin, apply the cream while skin is still damp. Do this within 3 minutes of leaving the bath or shower.
- The steroid cream should be applied to any itchy spots first. Then use the moisturizing cream as the top layer.
- While most parents prefer creams, moisturizing ointments are sometimes needed in the winter. An example is Vaseline.
- Caution: Never stop the moisturizing cream. Reason: The rash will come back.
-
Steroid Cream or Ointment for Itching:
- Itchy skin is the main symptom of eczema.
- Steroid creams or ointments are essential for controlling red, itchy skin.
- Apply steroid creams only to itchy or red spots (not to the normal skin).
- Most children have 2 types of steroid creams. (1) A mild steroid cream is used to treat any pink spots or mild itching. This is often 1% hydrocortisone cream (such as Cortaid). No prescription is needed. (2) Another stronger steroid cream is needed to treat any spots with severe itching. This is a prescription steroid cream such as Synalar. Never apply this stronger cream to the face.
- Apply these creams as directed or 2 times per day.
- After the rash quiets down, apply it once per day. After 1 good week just use moisturizing cream.
-
Bathing - Avoid Soaps:
- Give one bath a day for 10 minutes in lukewarm water. Reason: Water-soaked skin feels less itchy. Follow the bath with a moisturizing cream (such as Eucerin) to all the skin.
- Avoid all soaps. Reason: Eczema is very sensitive to soaps, especially bubble bath. There is no safe soap for young children with eczema. They can be cleaned using warm water.
-
Allergy Medicine for Itching at Bedtime:
- Many children with eczema need an allergy medicine by mouth at bedtime.
- Reason: Scratching in bed can cause severe skin breakdown. It may also interfere with falling sleep.
- Give the med your child's doctor wanted you to use for itching.
- If none was suggested, you can try Benadryl at bedtime. No prescription is needed.
- Caution: Do not use if age is under 1 year. Reason: Benadryl is a sedative. Give your doctor a call for advice.
-
Itching Attack - Shower to Remove Irritants:
- Playing in the grass, being around animals, or swimming can cause increased itching.
- For itching from these causes, give your child a quick shampoo and shower.
-
Itching Attack - Treatment:
- At the first sign of any itching, use the steroid cream. Put it on the areas that itch. If unsure, apply 1% hydrocortisone cream (such as Cortaid). No prescription is needed.
- Keep your child's fingernails cut short and smooth.
- Ask older children to try not to itch, but never punish for itching.
- For constant itching in young children, cover the hands with socks or gloves. Use for a day or until the itching is brought under control. Provide extra cuddling during this time.
-
Return to School:
- Eczema cannot be spread to others.
- Children with eczema do not need to miss any child care or school.
-
What to Expect:
- Eczema is a chronic condition. Around the teen years, about half get over their eczema.
- Many children who have severe eczema as babies develop asthma and nasal allergies.
-
Call Your Doctor If:
- Itching is not under control after 2 days of steroid cream
- Rash looks infected (spreading redness, yellow scabs or pus)
- You think your child needs to be seen
- Your child becomes worse
Prevention of Eczema Flare-Ups
-
Tips to Help Prevent Flare-Ups:
- Some flare-ups of eczema cannot be explained. But others are triggered by things that can be avoided.
- Avoid chlorine in swimming pools and spas, harsh chemicals, and soaps.
- Never use bubble bath. It can cause a major flare.
- Keep your child off the grass during grass pollen season.
- Avoid any animals that make the rash worse.
- If certain foods cause severe itching (flares), avoid them.
- Wear clothes made of cotton or cotton blends as much as possible. Avoid wool fibers and clothes made of other scratchy, rough materials. They make eczema worse.
- Try to avoid excess heat, excess cold and dry air (use a humidifier). Avoid over-dressing. Heat can make the rash worse.
- Caution: Keep your child away from anyone with fever blisters (cold sores). The herpes virus can cause a serious skin infection in children with eczema.
-
Call Your Doctor If:
- You have other questions or concerns
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.

This is how eczema can appear on the cheeks of a child. The skin is red, dry, cracked and swollen. Your child may find it itchy.

This shows eczema in the elbow crease of a teen. The skin is dry, cracked and swollen. It may be itchy.

This shows eczema in the elbow crease of a teen. The skin is dry and may be itchy. It also shows loss of skin pigment (color), which may happen in people with dark skin. Eczema can cause the skin color to be darker or lighter.
Emergency Symptoms Not to Miss
Most life-threatening emergencies are easy to recognize. You would not overlook major bleeding, breathing that stops, a seizure or a coma. You would call 911 for help.
- If you suspected poisoning, you would call the Poison Helpline at 1-800-222-1222.
- Some emergency symptoms, however, can be missed or ignored. Here's that important list.
- If your child has any of these symptoms, call your child's doctor now. If you can't reach them, go to the nearest ER. For a few of these symptoms, call 911.
Sick Newborn
- Your baby is less than 1 month old and has a fever or looks sick. This includes vomiting, cough, or even poor color. Your baby may start to act abnormal if they are getting sick. Examples are poor feeding or sleeping too much. At this age, these symptoms are serious until proven otherwise. During the first month of life, infections can progress very fast.
Lethargy
- Your young child is lethargic if she stares into space or won't smile. She won't play at all or hardly responds to you. Your child is too weak to cry or hard to wake up. These are serious symptoms.
- Note: Sleeping more when sick is normal. When awake, your child should be alert.
Confusion
- The sudden onset of confusion is serious. Your child is awake but says strange things. She sees things that aren't there. She doesn't recognize you.
- Note: Brief confusion for 5 minutes or so can be seen with high fevers. This can be normal. But, if not brief, confusion can have some serious causes.
Severe Pain
- Severe pain keeps your child from doing all normal activities. Your child won't play or even watch a favorite TV show. They just want to be left alone. Your child may cry when you try to hold or move them. Children with severe pain also can't sleep or can only fall asleep briefly.
Inconsolable Crying
- Constant nonstop crying is caused by severe pain until proven otherwise. Suspect this in children who can't sleep or can only fall asleep briefly. When awake, they will not join in any normal activities. They won't play or be distracted. They may be very hard to console. Caution: Instead of crying, severe pain may cause your child to moan or whimper.
Can't Walk
- If your child has learned to walk and then suddenly won't, call your doctor. He may have a serious injury to the legs or a problem with balance. If your child walks bent over holding his stomach, he may have appendicitis.
Vomits Bile
- Vomiting that is bright green is most often bile. Unless your child drank a green liquid, this is not normal. It can mean the intestines are blocked up. This is a surgical emergency.
- Note: Vomiting some yellow fluid is normal. The yellow color is from stomach acid.
Tender Belly
- Press on your child's belly while she is distracted by a toy or book. You should be able to press in an inch or so without a problem. If your child winces or screams, it suggests a serious cause. If the belly is also bloated and hard, it's more urgent.
- Note: If your child just pushes your hand away, you haven't distracted her enough.
Pain in Testicle or Scrotum
- Sudden pain in the scrotum can be from twisting (torsion) of the testicle. This needs surgery within 8 hours to save the testicle.
Trouble Breathing
- Breathing is essential for life. Most childhood deaths are caused by severe breathing problems. Breathing problems can be caused by throat or lung infections. Parents need to learn to recognize trouble breathing. If your child has tight croup or wheezing, they need to be seen now. Other bad signs are fast breathing, grunting with each breath, bluish lips, or retractions. This means the skin pulls in between the ribs with each breath. It is a sign of trouble breathing in younger children. Children with severe breathing problems can't drink, talk or cry. If your child is struggling to breathe, call 911.
Bluish or Gray Lips
- Bluish lips, tongue, or gums can mean not enough oxygen in the bloodstream. Call 911.
- Note: Bluish skin only around the mouth (not the lips) can be normal. It can be caused by being cold or being afraid.
Trouble Swallowing with Drooling
- The sudden onset of drooling or spitting means your child is having trouble swallowing. Most often, this is from severe swelling in the throat. The cause can be a serious throat infection. A serious allergic reaction can also cause trouble swallowing. Swelling in the throat could close off the airway.
Dehydration
- Dehydration means that your child's body fluids are low. Dehydration often is caused by severe vomiting and/or diarrhea. Suspect dehydration if your child has not urinated in 8 hours. Crying no tears and a dry inside of the mouth (tongue) are also signs. In young babies, the soft spot in the head is sunken. Dehydrated children are also tired and weak.
- Note: If your child is alert, playful and active, he is not yet dehydrated. Children with severe dehydration become dizzy when they stand. Dehydration needs extra fluids by mouth or vein.
Bulging Soft Spot
- The soft spot in your baby's head is tense and bulging. This means the brain is under pressure.
Stiff Neck
- A stiff neck means your child can't touch the chin to the chest. To test for a stiff neck, lay your child down. Then lift his head until the chin touches the chest. If he fights you, place a toy or coin on the belly. This makes him have to look down to see it. Older children can simply be asked to look at their belly button. A stiff neck can be an early sign of meningitis.
- Note: Without fever, a stiff neck is often from sore neck muscles.
Neck Injury
- Talk to your child's doctor about any neck injury, regardless of the symptoms. Neck injuries carry a risk of damage to the spinal cord.
Purple or Blood-Red Spots or Dots
- Purple or blood-red spots or dots on the skin need to be seen. When present with fever, they could be a sign of a serious bloodstream infection. The color of these serious rashes will not change when you press on them. The color of normal viral rashes will fade with skin pressure.
- Note: Bumps and bruises on the shins from active play are different.
Fever (over 100.4°F or 38 °C) in the First 3 Months
- Fevers in newborns and young babies are treated differently than fevers in older children. Bacterial infections are more common at this age and can get worse quickly. A fever is a rectal or forehead temp of 100.4 F° (38.0° C) or higher. All babies under 3 months of age with a fever need to be seen now. They need tests to decide if the cause is viral or bacterial.
Fever over 105° F (40.6° C)
- A fever tells you that your child has an infection. Serious infections can occur with low-grade fevers as well as higher fevers. All the above symptoms are stronger signs of serious illness than the level of fever. Research shows fevers alone are a risk factor only when very high. That means levels above 105°F (40.6°C). So, call your doctor if your child's fever goes above 104° F (40° C). This is a safe rule.
Chronic Diseases
- Most active chronic diseases can have some serious complications. If your child has a chronic disease, learn what those complications are. Find out how to recognize the early changes. Diseases at highest risk for serious infections are those that weaken the immune system. These include sickle cell disease, HIV, cancer, organ transplant, or taking oral steroids. If you are talking with health workers who don't know your child, speak up. Always tell them about your child's chronic disease (such as asthma). Never assume the doctors and nurses already know this.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.
Eye - Allergy
Is this your child's symptom?
- An allergic reaction of the eyes, usually from pollen
- The eyes are itchy and watery
If NOT, try one of these:
Symptoms of Eye Allergies
- Itchy eyes (sometimes feels like burning or stinging)
- Increased tearing (watery eyes)
- Red or pink eyes
- Mild swelling of the eyelids
- No discharge or a sticky, stringy, mucus discharge
- No pain or fever
Triggers of Eye Allergies
- Cause. An allergic reaction of the eyes to allergic substance. The medical name for this is allergic conjunctivitis. The allergic substance is called an allergen. Most allergens float in the air. That's how they get in the eyes. Here are the common ones:
- Pollens. Trees, grass, weeds and molds are the most common pollens. Tree pollens come in the spring. Grass pollens come in the summer. Weed pollens come in the fall. Pollens cause seasonal allergies. You can't avoid pollens because they are in the air. Most eye allergies continue through the pollen season. They can last 4 to 8 weeks. Pollens cause seasonal eye allergies.
- Pets. Allergens can also be from cats, dogs, horses, rabbits and other animals. Pet allergens are in the air. They can also get in the eyes from the hands. Most people don't keep a pet that they are allergic to. They only have sporadic allergy symptoms when they are exposed to a pet. These symptoms usually last a few hours. If you own the pet, your child will have symptoms all the time.
- House Dust. House dust contains many allergens. It always contains dust mites. If your humidity is high, it will contain mold. If someone with a cat visits you, they will bring cat dander with them. House dust causes year round, daily symptoms. The medical name for this is perennial eye allergies.
When to Call for Eye - Allergy
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Self Care at Home
|
Call Doctor Within 24 Hours
- You think your child needs to be seen
- Sacs of clear fluid (blisters) on whites of eyes
- Eyelids are swollen shut (or almost shut)
- Discharge on eyelids that does not go away with allergy medicines
Call Doctor During Office Hours
- Eyes are very itchy after taking allergy medicines for more than 2 days
- Diagnosis of eye allergy never made by a doctor
- You have other questions or concerns
Self Care at Home
- Mild eye allergy
Care Advice for Eye Allergy
-
What You Should Know About Eye Allergies:
- An eye allergy most often is caused by pollen that gets in the eye.
- The eyes can itch, burn or sting.
- All of these symptoms can go away with allergy eye drops.
- Eye allergies are common. They occur in 10% of children.
- Here is some care advice that should help.
-
Wash Allergens Off the Face:
- Use a wet washcloth to clean off the eyelids and face.
- Rinse the eyes with a small amount of warm water. Tears will do the rest.
- Then put a cold wet washcloth on the itchy eye.
- Prevention: Wash the hair every night because it collects lots of pollen.
-
Oral Allergy Medicines:
- If the nose is also itchy and runny, your child probably has hay fever. Hay fever is allergic symptoms of both the nose and eyes.
- Give your child an allergy medicine by mouth. This should get rid of the nose and the eye symptoms. Most often, eye drops will not be needed.
- A short-acting allergy medicine (such as Benadryl) may be helpful. No prescription is needed. They need to be given every 6 to 8 hours. The bedtime dosage is especially helpful for healing the lining of the nose.
- Long-acting allergy medicines (such as Zyrtec) can also be used. Again, no prescription is needed. This kind of medicine has 2 advantages over Benadryl. They cause less sedation and last up to 24 hours.
- Give allergy medicine every day. Do this until pollen season is over (about 2 months for each pollen).
-
Antihistamine Eye Drops (Ketotifen) for Pollen Allergies - 1st Choice:
- Usually, an oral allergy medicine will control the allergic symptoms of the eye.
- If the eyes remain itchy and poorly controlled, buy some Ketotifen antihistamine eye drops. Ask your pharmacist to suggest a brand (such as Zaditor). No prescription is needed.
- Age: Approved for 3 years and older.
- Dose: 1 drop every 12 hours in both eyes.
- For severe allergies, the use of ketotifen eye drops every day will help the most. Use these eye drops until pollen season is over.
-
Older Antihistamine/Vasoconstrictor Eye Drops - 2nd Choice:
- Often, the eyes will feel much better after the allergic substance is washed out. Also, putting a cold wet washcloth on them usually makes the eyes feel better.
- If not, this type of eye drop can be used for added relief. Ask your pharmacist to suggest a brand (such as Visine-A). The A stands for antihistamine. No prescription is needed.
- Avoid vasoconstrictor eyedrops without an allergy medicine in them. These are eye drops without an A in the name, such as plain Visine. Reason: They only treat the redness, not the cause.
- Dose: 1 drop every 8 hours as needed.
- Do not use for over 5 days. (Reason: Will cause red eyes from rebound effect)
- Downside: Doesn't work as well as Ketotifen eye drops.
-
Eye Drops: How to Use
- For a cooperative child, gently pull down on the lower lid. Put 1 drop inside the lower lid. Then ask your child to close the eye for 2 minutes. Reason: So the medicine will get into the tissues.
- For a child who won't open his eye, have him lie down. Put 1 drop over the inner corner of the eye. If your child opens the eye or blinks, the eye drop will flow in. If he doesn't open the eye, the drop will slowly seep into the eye.
-
Contact Lenses:
- Children who wear contact lenses need to switch to glasses for a while.
- This will help the eye heal faster.
-
What to Expect:
- If you know the cause of the allergy symptoms, try to avoid it. This is the case with animal allergies. The symptoms will not come back if there is no contact.
- But, you can't avoid pollens because they are in the air. Most eye allergies continue through the pollen season. They can last 4 to 8 weeks.
-
Call Your Doctor If:
- Itchy eyes aren't better in 2 days with allergy treatment
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.
Eye - Pus or Discharge
Is this your child's symptom?
- Yellow or green discharge (pus) in the eye
- The eyelids are stuck (matted) together with pus after sleep
- After being wiped away, the pus comes back during the day
- Often caused by a bacterial eye infection
If NOT, try one of these:
Causes of Eye with Pus
- Bacterial Conjunctivitis. This is a bacterial infection of the eye. The main symptom is eyelids stuck together with pus after sleep. Can be present in 1 or both eyes. A few viruses can cause pus in the eyes, but most don't.
- Viral Conjunctivitis. This is a viral infection of the eyes. Main symptom is pinkness of the white parts of the eyes. The eyes are also watery. Most often, there is no pus. Usually on both sides.
- Normal Discharge. A small amount of dried mucus only in the corner of the eye. It may not even be pus. A collection of mucus can be cream colored. Often due to an irritant that got in the eye from dirty hands. Needs no treatment except wiping it away with warm water.
- Blocked Tear Duct. Present in 10% of newborns. Main symptom is a constant watery eye. Tears fill the eye and run down the face. This happens even when not crying. The eye is not red and the eyelid is not swollen. The wet eye may get secondary infections. This will cause the eyelids to become matted with pus.
- Foreign Object in Eye (Serious). Small particles such as sand, dirt or sawdust can be blown into the eyes. The grit often gets stuck under the upper eyelid. If not removed, the eye reacts by producing pus. The main clue is an eye infection that does not respond to antibiotic eyedrops. Older children complain of feeling something in the eye.
- Eyelid Cellulitis (Serious). This is a deep infection of the eyelid and tissues around it. The main symptom is a red, swollen, very tender eyelid. The eye can be swollen shut. Usually only on one side. This can be a problem caused by bacterial conjunctivitis. The eye infection spreads inward. More commonly this is caused by an ethmoid sinus infection. That type occurs without any pus in the eye.
Symptoms of Bacterial Eye Infection
- Yellow or green discharge or pus in the eye
- Dried pus on the eyelids and eyelashes
- The eyelashes are more likely to be stuck together after sleep
- The whites of the eye may or may not be red or pink
- The eyelids are often puffy
When to Call for Eye - Pus or Discharge
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
|
Call Doctor or Seek Care Now
- Eyelid is very red or very swollen
- Vision is blurred
- Eye pain or discomfort is more than mild
- Fever over 104° F (40° C)
- Age less than 12 weeks old with fever. Caution: do NOT give your baby any fever medicine before being seen.
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Call Doctor Within 24 Hours
- Pus in the eye, but none of the symptoms above. Reason: you may need antibiotic eyedrops to treat it.
- Using antibiotic eye drops more than 3 days and pus is still there
Care Advice for Pus In the Eye
-
What You Should Know About Bacterial Eye Infections:
- Bacterial eye infections are common with colds.
- They respond to home treatment with antibiotic eye drops which need a prescription.
- They are not harmful to vision.
- Until you get some antibiotic eye drops, here is some advice that should help.
-
Remove Pus:
- Remove all the dried and liquid pus from the eyelids. Use warm water and wet cotton balls to do this.
- Do this whenever pus is seen on the eyelids.
- Also, remove the pus before the antibiotic eye drops are put in. Reason: They will not work if you don't.
- The pus can spread infection to others. So, dispose of it carefully.
- Wash your hands well after any contact with the pus.
-
Antibiotic Eye Drops: How to Use
- For a cooperative child, gently pull down on the lower lid. Put 1 drop inside the lower lid. Then ask your child to close the eye for 2 minutes. Reason: So the medicine will get into the tissues.
- For a child who won't open his eye, have him lie down. Put 1 drop over the inner corner of the eye. If your child opens the eye or blinks, the eye drop will flow in. If he doesn't open the eye, the drop will slowly seep into the eye.
-
Contact Lenses:
- Children who wear contact lenses need to switch to glasses until the infection is gone.
- Reason: To prevent damage to the cornea.
- Disinfect the contacts before wearing them again.
- Discard them if they are disposable.
-
Return to School:
- Your child can return to school when the pus is a small amount.
- Antibiotic eye drops should be used for 24 hours before going back.
- The antibiotic eye drops can be used for other family members. Use only if they develop the same symptoms.
-
What to Expect:
- With treatment, the yellow discharge should clear up in 3 days.
- The red eyes may last up to a week.
-
Call Your Doctor If:
- Eyelid gets red or swollen
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.
Eye - Red Without Pus
Is this your child's symptom?
- Red or pink color of the white of the eye without any pus
- The eye looks irritated
- May have increased tears (a watery eye)
- Eyelid may be puffy (mildly swollen)
- No pus or yellow discharge
- Not caused by an eye injury
If NOT, try one of these:
Causes of Pinkeye (Red Eye)
- Pinkeye Defined. When the white of the eye becomes pink or red, it's called pinkeye. Conjunctivitis is the medical name for pinkeye. The conjunctiva is the membrane that covers the white of the eye. It becomes pink or red when it is infected or irritated. Pinkeye (conjunctivitis) has many causes.
- Viral Conjunctivitis is the main cause of pink or red eyes without pus. Most often, it is part of a cold.
- Bacterial Conjunctivitis. Pinkeye plus the eyelids are stuck together with pus. Most likely, this is a secondary infection of a viral conjunctivitis.
- Allergic Conjunctivitis from pollens. Most children with eye allergies also have nasal allergies (hay fever). Symptoms include sneezing and clear nasal discharge.
- Irritant Conjunctivitis from sunscreen, soap, chlorine in pool water, smoke, or smog. Irritants can also be transferred by touching the eye with dirty fingers. Irritants can be food or plant resins.
- Contact Lens Conjunctivitis is caused by poor use of disinfectant solution or lenses kept in overnight.
- Rebound Conjunctivitis from Vasoconstrictor Eye Drop Abuse. Usually occurs in teens who use daily OTC eye drops to remove mild redness. After the medicine wears off, the blood vessels become larger than they were to begin with. Similar to the rebound nasal congestion seen in chronic nose drop abuse.
- Foreign Object. If only one side has pinkeye, an object in the eye must be considered.
- Palpebral Cellulitis (Serious). A bacterial infection of the eyelids and skin around them. Causes the lids to be very red and swollen.
When to Call for Eye - Red Without Pus
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Self Care at Home
|
Call Doctor or Seek Care Now
- Eyelid is very red or very swollen
- Nonstop tears or blinking
- Vision is blurred
- Eye pain or discomfort is more than mild
- Turns away from any light
- Age less than 12 weeks old with fever. Caution: do NOT give your baby any fever medicine before being seen.
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Call Doctor Within 24 Hours
- Only 1 eye is red and lasts more than 24 hours
- Fever lasts more than 3 days
- Fever returns after being gone more than 24 hours
- You think your child needs to be seen, but the problem is not urgent
Call Doctor During Office Hours
- Age less than 1 month old
- Redness lasts more than 7 days
- You have other questions or concerns
Self Care at Home
- Red eye is part of a cold
- Red eye is caused by mild irritant (such as soap, sunscreen, food, smoke, chlorine)
Care Advice
Treatment for Viral Eye Infections
-
What You Should Know About Viral Eye Infections:
- Some viruses cause watery eyes (viral conjunctivitis).
- It may be the first symptom of a cold.
- It isn't serious. You can treat this at home.
- Colds can cause a small amount of mucus in the corner of the eye.
- Here is some care advice that should help.
-
Eyelid Rinse:
- Cleanse eyelids with warm water and a clean cotton ball.
- Try to do this 3 times a day.
- This usually will keep a bacterial infection from occurring.
-
Artificial Tears:
- Artificial tears often make red eyes feel better. No prescription is needed. They can be used at any age.
- Use 1 drop per eye 3 times a day as needed. Use them after cleansing the eyelids.
- Antibiotic and vasoconstrictor eye drops do not help viral eye infections.
-
Eye Drops: How to Use
- For a cooperative child, gently pull down on the lower lid. Put 1 drop inside the lower lid. Then ask your child to close the eye for 2 minutes. Reason: So the medicine will get into the tissues.
- For a child who won't open his eye, have him lie down. Put 1 drop over the inner corner of the eye. If your child opens the eye or blinks, the eye drop will flow in. If he doesn't open the eye, the drop will slowly seep into the eye.
-
Contact Lenses:
- Children who wear contact lenses need to switch to glasses until the infection is gone.
- Reason: To prevent damage to the cornea.
-
Return To School:
- Pinkeye with watery discharge is harmless. There is a slight risk it could be passed to others.
- Children with pink eyes from a cold do not need to miss any school.
- Pinkeye is not a public health risk. Keeping these children home is over-reacting. If asked, tell the school your child is on eye drops (artificial tears).
-
What to Expect:
- Pinkeye with a cold usually lasts about 7 days.
- Sometimes, it turns into a bacterial eye infection. You can tell because the eyelids will become
stuck together with pus. - Pinkeye from an irritant usually goes away within 2 hours after it's removed.
-
Call Your Doctor If:
- Your child gets pus in the eye
- Redness lasts more than 1 week
- You think your child needs to be seen
- Your child becomes worse
Treatment for Mild Eye Irritants
-
What You Should Know About Pinkeye from Irritants:
- Most eye irritants cause redness of the eyes.
- It that will go away on its own.
- You can treat that at home.
-
Face Wash:
- Wash the face with mild soap and water.
- This will remove any irritants still on the face.
-
Eyelid Rinse:
- Rinse the eyelids with warm water for 5 minutes.
-
Eye Drops:
- Red eyes from irritants usually feel much better after being washed out.
- At any age, if eyes remain bloodshot, you can use some artificial tears.
- Dose: 1 drop, 3 times per day, as needed.
- If more than 6 years old, switch to a vasoconstrictor eye drop (such as Visine). No prescription is needed.
- Dose: Use 1 drop. May repeat once in 8 to 12 hours. Never use for more than 3 days.
-
What to Expect:
- After the irritant is removed, the eyes usually return to normal color.
- This may take 1 to 2 hours.
-
Prevention:
- Try to avoid future contact with the irritant.
-
Call Your Doctor If:
- Pus in the eye occurs
- Redness lasts more than 7 days
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.
Eye Injury
Is this your child's symptom?
- Injuries to the eye, eyelid, and area around the eye
If NOT, try one of these:
Types of Eye Injuries
- Cut or Scratch of Eyelid. Small cuts heal on their own. Deep cuts or ones that go through the edge of the eyelid need sutures.
- Bruise of the Eyelids. Also called a "black eye". The swelling and bruise get worse for a few days. Then it will go away on its own over 2 -3 weeks. It's normal for the bruise to change colors as it heals.
- Subconjunctival Hemorrhage. This is a flame-shaped bruise of the white part (sclera) of the eyeball. It's bright red. It's caused by a scratch to the sclera. It's a mild injury that will go away on its own over 2 weeks.
- Corneal Abrasion. A scratch of the clear part (cornea) of the eye. The cornea is the window in front of the iris. The main symptoms are severe eye pain, tearing and constant blinking. Some children will just hold their eye closed. Caused by a scratch from a branch of a tree or bush. Can also be caused by a foreign object stuck under the upper eyelid. Most are minor and heal in 2 days. This is the most common eye injury that needs to see a doctor.
- Acute Hyphema (Serious). It means bleeding in the space between the cornea and the iris. The blood often layers out at the bottom of the cornea. It's caused by blunt trauma.
- Punctured Eyeball (Serious). It means a sharp object has completely torn the cornea or sclera. Can happen with tiny objects thrown by a lawnmower.
Vision
- The main concern is whether the vision is damaged.
- Older children can tell us if their vision is blurred or out of focus. You can test this at home. Cover each eye in turn and having them look at a distant object.
- Children less than 5 years old usually need to be examined. This is also true even if the injury seems minor. Having an exam is the only way to know the child's vision is okay.
When to Call for Eye Injury
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Self Care at Home
|
Call Doctor or Seek Care Now
- Pupils not equal in size
- Sharp object hit the eye (such as a metal chip or flying glass)
- Skin is split open or gaping and may need stitches
- Any cut on the eyelid or eyeball
- Age less than 1 year old
- You think your child has a serious injury
- You think your child needs to be seen, and the problem is urgent
Call Doctor Within 24 Hours
- Bruises near the eye
- You think your child needs to be seen, but the problem is not urgent
Call Doctor During Office Hours
- Dirty cut and no tetanus shot in more than 5 years
- Clean cut and no tetanus shot in more than 10 years
- You have other questions or concerns
Self Care at Home
- Minor eye injury
Care Advice for Minor Eye Injuries
-
Small Cuts, Scratches or Scrapes Treatment:
- For any bleeding, put direct pressure on the wound. Use a gauze pad or clean cloth. Press for 10 minutes or until the bleeding has stopped.
- Wash the wound with soap and water for 5 minutes. Protect the eye with a clean cloth.
- For cuts or scrapes, use an antibiotic ointment (such as Polysporin). No prescription is needed.
Put it on the cut 3 times a day. Do this for 3 days. - Cover large scrapes with a bandage (such as Band-Aid). Change daily.
-
Swelling or Bruises with Intact Skin (including a Black Eye) Treatment:
- Put a cold pack or ice wrapped in a wet cloth on the eye. Do this for 20 minutes. This will help stop the bleeding and swelling. Repeat as needed.
- A black eye usually takes 1 to 2 days to occur.
- A flame-shaped bruise of the white of the eyeball is also common.
- After 48 hours, use a warm wet cloth for 10 minutes. Do this 3 times per day. Reason: To help reabsorb the blood.
-
Pain Medicine:
- To help with the pain, give an acetaminophen product (such as Tylenol).
- Another choice is an ibuprofen product (such as Advil).
- Use as needed.
-
What to Expect:
- Minor cuts and scratches, as well as bruises, are harmless.
- They last about 2 weeks.
- They do not need any medicine to help them go away.
-
Call Your Doctor If:
- Pain becomes severe
- Changes in vision
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.
Eye Swelling
Is this your child's symptom?
- Swelling of eyelids or area around the eye
- No redness of white part of the eye (sclera)
- No yellow or green discharge (pus)
- Swelling is not caused by an eye injury. If so, see that guide.
- Eye Swelling Scale
- Mild: eyelid is puffy, but can open eyes like normal
- Moderate: more than puffy, but eyes still open some
- Severe: eyelids swollen shut or almost shut
If NOT, try one of these:
Causes of Eye Swelling on One Side
- Rubbing the Eye. Rubbing from any cause will make the eyelids puffy. Often, it starts from getting an irritant in the eye. Young children often touch their eyes with dirty hands. They also may get food in the eye.
- Insect Bite near the eye. A reaction to the insect's spit causes swelling. The loose eye tissues swell easily. The most common bite is from a mosquito.
- Contact Dermatitis near the eye. An example is poison ivy.
- Injury near the eye. Can cause a bruise and swelling.
- Sty. A minor infection of an eyelash.
- Dacryocystitis. An infection of the tear sac in the corner of the eye.
- Ethmoid Sinus Infection (serious). This causes swelling and redness of the eyelid. The ethmoid sinus is behind the eye.
- Periorbital Cellulitis (serious). A bacterial infection of the eyelid. Caused by spread from nearby infected wound or insect bite. The eyelid is very red and usually painful to touch.
Causes of Eye Swelling on Both Sides
- Allergic Conjunctivitis. Itchy pink eyes from pollen or pet dander.
- Viral Conjunctivitis. The main symptom is red eyes with a cold.
- Bacterial Conjunctivitis. The main symptom is yellow pus in the eye or eyes. Eyelids may be matted shut.
- Edema (serious). Edema is retained fluid within body tissues. Edema fluid first appears as swelling of the feet due to gravity. Edema fluid also occurs around both eyes after lying down. It's caused by kidney, heart or liver failure.
- Anaphylaxis (very serious). A severe life-threatening allergic reaction. Triggered by foods, drugs and bee stings. Serious symptoms such as trouble breathing or swallowing occur. Hives are almost always present.
Swelling of Eye: Clues to the Cause
- Swelling of 1 eye is often due to an insect bite. Mosquito bites are a common cause. It can also be from an irritant (e.g. food) transferred to the eye by the hands.
- Suspect mosquito bites if there are bites on other parts of the body. Insect bites of the upper face can cause the eyelid to swell. This can last for a few days. With insect bites, the swelling can be pink as well as large. Large swelling is common for ages 1-5 years.
- Swelling of both eyes is usually due to pollen that's airborne. This includes tree, grass or weed pollen. These pollens float in the air and can travel hundreds of miles. Itching also makes the swelling worse.
- Swelling of the face is usually due to allergic reactions to swallowed substances. Examples are foods or medicines. May be part of a severe allergic reaction.
- Allergic reactions to antibiotic eyedrops can cause severe swelling of both eyes.
- Swollen eyelids from insect bites, pollens or other allergies are itchy.
- Swollen eyelids from eyelid infections are painful and tender to the touch.
When to Call for Eye Swelling
Call 911 Now
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Self Care at Home
|
Call 911 Now
- You think your child has a life-threatening emergency
Call Doctor or Seek Care Now
- Severe swelling (shut or almost) of both eyes
- Severe swelling (shut or almost) of one eye with fever
- Eyelid (outer) is very red and swollen with fever
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Call Doctor Within 24 Hours
- Fever
- Severe swelling (shut or almost) of one eye without fever
- Eyelid (outer) is very red and swollen without fever
- Eyelid is painful or very tender
- Swollen ankles or feet
- Sinus pain or pressure
- Moderate swelling with the eye open some. Exception: due to a mosquito bite.
- You think your child needs to be seen, but the problem is not urgent
Call Doctor During Office Hours
- Mild swelling (puffy eye or eyes) lasts more than 3 days
- Eyelid swelling is a chronic problem and not explained
- You have other questions or concerns
Self Care at Home
- Eyelid swelling from suspected bug bite
- Eyelid swelling without a cause
Care Advice
Treatment for Eyelid Swelling from Suspected Bug Bite
-
What You Should Know About Eye Swelling from Bug Bites:
- Mosquito bites are very common.
- Bites to the face can cause severe swelling around the eye. Reason: The tissues around the eye are loose.
- Size is larger in young children.
- The swelling is harmless.
- Here is some care advice that should help.
-
Cold Pack for Swelling:
- Apply ice wrapped in a wet washcloth to the eye for 20 minutes.
-
Allergy Medicine for Swelling and Itching:
- Give an allergy medicine by mouth. This will help to lessen the swelling and itching.
- Benadryl every 6 hours is best. Teen dose is 50 mg.
- Give it 2 or 3 times.
- If you only have another allergy med at home (but not Benadryl), use that. Follow the package directions.
-
Eye Drops:
- The eyelid swelling often will improve after a cold pack or Benadryl is given.
- Age 6 years and older. For eyelid swelling that interferes with vision after cold pack, use some eye drops. Use a long-acting vasoconstrictor eye drop (such as Visine). No prescription is needed.
- Dose: 1 drop every 8 to 12 hours as needed for 1 or 2 days.
- Do not use for over 5 days. Reason: Will cause red eyes from rebound effect.
-
What to Expect:
- Itching may last for 2 days.
- Pinkness or redness lasts about 3 days.
- The eye may be puffy for up to 7 days.
-
Call Your Doctor If:
- Swelling lasts over 7 days
- Redness lasts over 3 days
- Becomes painful to touch
- You think your child needs to be seen
- Your child becomes worse
Treatment for Eyelid Swelling Without a Cause
-
What You Should Know about Eyelid Swelling Without a Cause:
- Most eye swelling without a cause is from rubbing the eyes.
- The eye tissues are loose and easily swell.
- The rubbing is often from getting an irritant in the eye. It's often seen in young children who touch their eyes with dirty hands. While eating, some children even get food in their eyes.
- This type of swelling to an irritant can be treated at home.
- Here is some care advice that should help.
-
Cold Pack for Swelling:
- Apply ice wrapped in a wet washcloth to the eye for 20 minutes.
-
Allergy Medicine for Swelling and Itching:
- Give an allergy medicine by mouth. This will help to lessen the swelling and itching.
- Benadryl every 6 hours is best. Teen dose is 50 mg.
- Give it 2 or 3 times.
- If you only have another allergy med at home (but not Benadryl), use that. Follow the package directions.
-
Eye Drops:
- The eyelid swelling often will improve after a cold pack or Benadryl is given.
- Age 6 years and older. For eyelid swelling that interferes with vision after cold pack, use some eye drops. Use a long-acting vasoconstrictor eye drop (such as Visine). No prescription is needed.
- Dose: 1 drop every 8 to 12 hours as needed for 1 or 2 days.
- Do not use for over 5 days. Reason: Will cause red eyes from rebound effect.
-
What to Expect:
- The itching should stop after the irritant is washed out of the eye. This may take up to a few hours.
- The swelling will clear 24 hours after the child stops rubbing the eye.
-
Call Your Doctor If:
- Swelling lasts over 3 days
- Eyelid becomes red and painful to the touch
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.
Fever
Is this your child's symptom?
- An abnormal high body temperature
- Fever is the only symptom. Your child has a true fever if:
- Rectal (Bottom), Ear or Forehead temperature: 100.4° F (38.0° C) or higher
- Oral (Mouth) temperature: 100° F (37.8° C) or higher
- Under the arm (Armpit) temperature: 99° F (37.2° C) or higher
- Caution: Ear temperatures are not accurate before 6 months of age
- Caution: Forehead temperatures must be digital. Forehead strips are not accurate.
If NOT, try one of these:
Causes of Fever
- Overview. Almost all fevers are caused by a new infection. Viruses cause 10 times more infections than bacteria. The number of germs that cause an infection are in the hundreds. Only a few common ones will be listed.
- Viral Infections. Colds, flu and other viral infections are the most common cause. Fever may be the only symptom for the first 24 hours. The start of viral symptoms (runny nose, cough, loose stools) is often delayed. Roseola is the most extreme example. Fever may be the only symptom for 2 or 3 days. Then a rash appears.
- Bacterial Infections. A bladder infection is the most common cause of silent fever in girls. Strep throat is also a common cause of unexplained fever.
- Sinus Infection. This is a problem caused by a cold. The main symptom is the return of fever after it has been gone for a few days. The sinus congestion also changes to sinus pain. Color of nasal discharge is not very helpful for making this diagnosis.
- Vaccine Fever. Fever with most vaccines begins within 12 hours. It lasts 2 to 3 days. This is normal and harmless. It means the vaccine is working.
- Newborn Fever (Serious). Fever that occurs during the first 3 months of life can be serious. All of these babies need to be seen as soon as possible. The fever may be due to sepsis (a bloodstream infection). Bacterial infections in this age group can get worse quickly. They need rapid treatment.
- Meningitis (Very Serious). A bacterial infection of the membrane that covers the spinal cord and brain. The main symptoms are a stiff neck, headache and confusion. Younger children are lethargic or so irritable that they can't be consoled. If not treated early, can suffer brain damage.
- Overheated. The fever is usually low grade. Can occur during heat waves or from being overdressed. The temp becomes normal in a few hours after moving to a cooler place. Can also occur during hard exercise. Fever goes away quickly with rest and drinking extra fluids.
- Not Due to Teething. Research shows that "getting teeth" does not cause fevers.
Fever and Crying
- Fever on its own shouldn't cause much crying.
- Frequent crying in a child with fever is caused by pain until proven otherwise.
- Hidden causes can be ear infections, kidney infections, sore throats and meningitis.
Roseola: Classic Cause of Unexplained Fever in Young Children
- Most children get Roseola between 6 months and 3 years of age.
- Cause: human herpes virus 6
- Rash: pink, small, flat spots on the chest and stomach. Rash is the same on both sides of the body.
- Then spreads to the face.
- Classic feature: 2 or 3 days of high fever without a rash or other symptoms.
- The rash starts 12 to 24 hours after the fever goes away.
- The rash lasts 1 to 3 days.
- By the time the rash appears, the child feels fine.
Normal Temperature Range
- Rectal. A reading of 98.6° F (37° C) is just the average rectal temp. A normal low can be 96.8° F (36° C) in the morning. It can change to a high of 100.3° F (37.9° C) late in the day. This is a normal range.
- By mouth. A reading of 97.6° F (36.5° C) is just the average mouth temp. A normal low can be 95.8° F (35.5° C) in the morning. It can change to a high of 99.9° F (37.7° C) late in the day. This is a normal range.
When to Call for Fever
Call 911 Now
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Self Care at Home
|
Call 911 Now
- Not moving or too weak to stand
- Can't wake up
- Trouble breathing with bluish lips or face
- Purple or blood-colored spots or dots on skin
- You think your child has a life-threatening emergency
Call Doctor or Seek Care Now
- Trouble breathing
- Great trouble swallowing fluids or spit
- Not alert when awake ("out of it")
- Acts or talks confused
- Age less than 12 weeks old with any fever. Caution: do NOT give your baby any fever medicine before being seen.
- Fever over 104° F (40° C)
- Shaking chills (shivering) lasting more than 30 minutes
- Nonstop crying or cries when touched or moved
- Won't move an arm or leg normally
- Dehydration suspected. No urine in more than 8 hours, dark urine, very dry mouth and no tears.
- Pain or burning when passing urine
- Weak immune system. Examples are: sickle cell disease, HIV, cancer, organ transplant, taking oral steroids.
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Call Doctor Within 24 Hours
- Age 3-6 months old with fever
- Age 6-24 months old with fever that lasts more than 24 hours. There are no other symptoms (such as cough or diarrhea).
- Fever lasts more than 3 days
- Fever returns after being gone more than 24 hours
- Recent travel outside the country to high risk area
- You think your child needs to be seen, but the problem is not urgent
Call Doctor During Office Hours
- You have other questions or concerns
Self Care at Home
- Fever with no other symptoms and your child acts mildly ill
Care Advice for Fever
-
What You Should Know About Fever:
- Having a fever means your child has a new infection.
- It's most likely caused by a virus.
- You may not know the cause of the fever until other symptoms develop. This may take 24 hours.
- Most fevers are good for sick children. They help the body fight infection.
- Use the ranges below to help put your child's level of fever into perspective:
- 100° - 102° F (37.8° - 39° C) Low grade fever: helpful, good range. Don't treat.
- 102° - 104° F (39 - 40° C) Average fever: helpful. Treat if causes discomfort.
- Over 104° F (40° C) High fever: causes discomfort, but harmless. Always treat.
- Over 106° F (41.1° C) Very high fever: important to bring it down. Rare to go this high.
- Over 108° F (42.3° C) Dangerous fever: fever itself can be harmful.
-
Treatment for All Fevers - Extra Fluids
- Fluids alone can lower the fever. Reason: being well-hydrated helps the body give off heat through the skin.
- Offer your child extra water or other fluids by mouth. Cold fluids are better. Until 6 months old, only give extra formula or breastmilk.
- For all children, dress in 1 layer of light weight clothing, unless shivering. Reason: also helps heat loss from the skin.
- Caution: if a baby under 1 year has a fever, never overdress or bundle up. Reason: babies can get over-heated more easily than older children.
- For fevers 100°-102° F (37.8° - 39°C), fever meds are rarely needed. Fevers of this level don't cause discomfort. They do help the body fight the infection.
- Exception: if you feel your child also has pain, treat it.
-
Fever Medicine:
- Fevers only need to be treated with medicine if they cause discomfort. Most often, that means fevers above 102° F (39° C). Also use for shivering (shaking chills). Shivering means the fever is going up.
- For fevers above 102° F (39° C), give an acetaminophen product (such as Tylenol).
- Another choice is an ibuprofen product (such as Advil).
- Goal of treatment: Bring the temperature down to a comfortable level. Most often, the fever meds lower the fever by 2° to 3° F (1 - 1.5° C). They do not bring it down to normal. It takes 1 or 2 hours to see the effect.
- Do not use aspirin. Reason: Risk of Reye syndrome, a rare but serious brain disease.
- Do not use both acetaminophen and ibuprofen together. Reason: Not needed and a risk of giving too much.
-
Sponging With Lukewarm Water:
- Note: Sponging is an option for high fevers, but not required. It is rarely needed.
- When to Use: Fever above 104° F (40° C) AND doesn't come down with fever meds. Always give the fever medicine at least an hour to work before sponging.
- How to Sponge: Use lukewarm water (85 - 90° F) (29.4 - 32.2° C). Sponge for 20-30 minutes.
- If your child shivers or becomes cold, stop sponging. Other option: You can also make the water warmer.
- Caution: Do not use rubbing alcohol. Reason: Can cause a coma.
-
Return to School:
- Your child can return to school after the fever is gone. Your child should feel well enough to join in normal activities.
-
What to Expect:
- Most fevers with viral illnesses range between 101° and 104° F (38.4° and 40° C).
- They may last for 2 or 3 days.
- They are not harmful.
-
Call Your Doctor If:
- Your child looks or acts very sick
- Any serious symptoms occur such as trouble breathing
- Fever goes above 104° F (40° C)
- Any fever occurs if less than 12 weeks old
- Fever without other symptoms lasts more than 24 hours (if age less than 2 years)
- Fever lasts more than 3 days (72 hours)
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.
Fever - How to Take the Temperature
When Does Your Child Have a Fever?
- Rectal, Forehead or Ear temperature: 100.4° F (38.0° C) or higher
- Oral (mouth) temperature: 100° F (37.8° C) or higher
- Under the arm (armpit) temperature: 99° F (37.2° C) or higher
- Caution: Ear temperatures are not accurate before 6 months of age
Where to Take the Temperature
- Rectal temps are the most accurate. Forehead temps are the next most accurate. Oral and ear temps are also accurate if done properly. Temps done in the armpit are the least accurate. Armpit temps are useful for screening at any age.
- Age under 3 months old (90 days old).An armpit temp is the safest and is good for screening. If the armpit temp is above 99° F (37.2° C), re-check it. Use a rectal reading. Reason: If young babies have a fever, they need to see a doctor now. New research shows that forehead temps may also be accurate under 3 months of age.
- Age 3 months to 4 years old. Rectal or forehead temps are accurate. An ear thermometer can be used after 6 months old. An armpit temp is good for screening if it is taken right.
-
Age 4 years and older.
Safe to take the temp orally (by mouth). Ear and forehead thermometers are also good. - Digital (electronic) thermometers are easily found in stores. They do not cost very much. They can be used for rectal, armpit and oral temps. Most of them give an accurate temp in 10 seconds or less. The AAP suggests you replace any glass thermometer in the house with one of these products.
Rectal Temperature: How to Take
- Age: Birth to 4 years old
- Have your child lie stomach down on your lap. Another way is on the back with the legs pulled up to the chest.
- Put some petroleum jelly on the end of the thermometer and the anus.
- Slide the thermometer gently into the anus no more than 1 inch. If your child is less than 6 months old, put it in no more than ½ inch. That means until you can no longer see the silver tip.
- Be gentle. There should not be any resistance. If there is, stop.
- Hold your child still. Leave a digital thermometer in until it beeps (about 10 seconds).
- Your child has a fever if the rectal temp is above 100.4° F (38° C).
Armpit Temperature: How to Take
- Age: Any age for screening
- Put the tip of the thermometer in an armpit. Make sure the armpit is dry.
- Close the armpit by holding the elbow against the chest. Do this until it beeps (about 10 seconds). The tip of the thermometer must stay covered by skin.
- Your child has a fever if the armpit temp is above 99.0° F (37.2° C). If you have any doubt, take your child's temp by rectum or forehead.
Oral Temperature: How to Take
- Age: 4 years and older
- If your child had a cold or hot drink, wait 30 minutes.
- Put the thermometer under one side of the tongue towards the back. It's important to put the tip in the right place.
- Have your child hold the thermometer with his lips and fingers. Don't use the teeth to keep in place. Keep the lips sealed until it beeps (about 10 seconds).
- Your child has a fever if the temp is above 100° F (37.8° C).
Digital Pacifier Temperature: How to Take
- Age: Birth to 1 year. Only good for screening. Requires the baby to suck on it, which is not always possible.
- Have your child suck on the pacifier until it beeps (about 10 seconds).
- Your child has a fever if the pacifier temp is above 100° F (37.8° C).
Ear Temperature: How to Take
- Age: 6 months and older (not accurate before 6 months)
- This thermometer reads the heat waves coming off the eardrum.
- A correct temp depends on pulling the ear backward. Pull back and up if over 1 year old.
- Then aim the tip of the ear probe between the opposite eye and ear.
- Parents like this thermometer because it takes less than 2 seconds. It also does not need the child to cooperate. It does not cause any discomfort.
- Caution. Being outdoors on a cold day will cause a low reading. Your child needs to be inside for 15 minutes before taking the temp. Earwax, ear infections and ear tubes do not keep from getting correct readings.
Forehead (Temporal Artery) Temperature: How to Take
- Age: Any age
- This thermometer reads the heat waves coming off the temporal artery. This blood vessel runs across the forehead just below the skin.
- Place the sensor head at the center of the forehead.
- Slowly slide the thermometer across the forehead toward the top of the ear. Keep it in contact with the skin.
- Stop when you reach the hairline.
- Read your child's temp on the display screen.
- Note: some newer forehead thermometers don't need to slide across the forehead. Follow the box directions on how to take the temp.
- Used in more doctor's offices than any other thermometer.
- Parents like this thermometer because it takes less than 2 seconds. It also does not need the child to cooperate. It does not cause any discomfort.
- Caution: Forehead temperatures must be digital. Forehead strips are not accurate.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.
Fever - Myths Versus Facts
Many parents have false beliefs (myths) about fever. They think fever will hurt their child. They worry and lose sleep when their child has a fever. This is called fever phobia. In fact, fevers are harmless and often helpful. Let these facts help you better understand fever.
MYTH. My child feels warm, so she has a fever.
FACT. Children can feel warm for a many reasons. Examples are playing hard, crying, getting out of a warm bed or hot weather. They are "giving off heat." Their skin temperature should return to normal in about 20 minutes. About 80% of children who act sick and feel warm do have a fever. If you want to be sure, take the temperature. These are the cutoffs for fever using different types of thermometers:
- Rectal (bottom), ear or forehead temperature: 100.4° F (38.0° C) or higher
- Oral (mouth) temperature: 100° F (37.8° C) or higher
- Under the arm (Armpit) temperature: 99° F (37.2° C) or higher
MYTH. All fevers are bad for children.
FACT. Fevers turn on the body's immune system. They help the body fight infection. Normal fevers between 100° and 104° F (37.8° - 40° C) are good for sick children.
MYTH. Fevers above 104° F (40° C) are dangerous. They can cause brain damage.
FACT. Fevers with infections don't cause brain damage. Only temperatures above 108° F (42° C) can cause brain damage. It's very rare for the body temperature to climb this high. It only happens if the air temperature is very high. An example is a child left in a closed car during hot weather.
MYTH. Anyone can have a seizure triggered by fever.
FACT. Only 4% of children can have a seizure with fever.
MYTH. Seizures with fever are harmful.
FACT. These seizures are scary to watch, but they stop within 5 minutes. They don't cause any permanent harm. They don't increase the risk for speech delays, learning problems, or seizures without fever.
MYTH. All fevers need to be treated with fever medicine.
FACT. Fevers only need to be treated if they cause discomfort (makes your child feel bad). Most fevers don't cause discomfort until they go above 102° or 103° F (39° or 39.5° C).
MYTH. Without treatment, fevers will keep going higher.
FACT. Wrong, because the brain knows when the body is too hot. Most fevers from infection don't go above 103° or 104° F (39.5°- 40° C). They rarely go to 105° or 106° F (40.6° or 41.1° C). While these are "high" fevers, they also are harmless ones.
MYTH. With treatment, fevers should come down to normal.
FACT. With treatment, most fevers come down 2° or 3° F (1° or 1.5° C).
MYTH. If you can't "break the fever", the cause is serious.
FACT. Fevers that don't come down to normal can be caused by viruses or bacteria. The response to fever medicines tells us nothing about the cause of the infection.
MYTH. Once the fever comes down with medicines, it should stay down.
FACT. It's normal for fevers with most viral infections to last for 2 or 3 days. When the fever medicine wears off, the fever will come back. It may need to be treated again. The fever will go away and not return once the body overpowers the virus. Most often, this is day 3 or 4.
MYTH. If the fever is high, the cause is serious.
FACT. If the fever is high, the cause may or may not be serious. If your child looks very sick, the cause is more likely to be serious.
MYTH. The exact number of the temperature is very important.
FACT. How your child looks and acts is what's important. The exact temperature number is not.
MYTH. Oral temperatures between 98.7° and 100° F (37.1° to 37.8° C) are low-grade fevers.
FACT. These temperatures are normal. The body's normal temperature changes throughout the day. It peaks in the late afternoon and evening. A true low-grade fever is 100° F to 102° F (37.8° - 39° C) .
SUMMARY. Keep in mind that fever is fighting off your child's infection. Fever is one of the good guys.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.
Fifth Disease
Is this your child's symptom?
- Viral rash that starts with red cheeks and spreads to the shoulders
If NOT, try one of these:
Symptoms of Fifth Disease
- Bright red cheeks on both sides for 1 to 3 days. Looks like "slapped cheeks".
- Followed by pink "lace-like" (net-like) rash of arms and legs.
- "Lacy" rash mainly is on thighs and upper arms/shoulders.
- Rash also is on chest and stomach in 50% of children.
- The rash does not itch or hurt.
- No fever or low-grade one less than 102° F (39° C).
- Peak age: 4 -12 years.
Cause of Fifth Disease
- It is caused by the human parvovirus B19.
- Not related to the dog parvovirus.
Prevent Spread to Others
- Good hand washing can prevent spread of this illness.
- Once the rash occurs, the child can no longer spread the virus.
When to Call for Fifth Disease
Call 911 Now
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Self Care at Home
|
Call 911 Now
- You think your child has a life-threatening emergency
Call Doctor or Seek Care Now
- Only 1 cheek is red and also has fever
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Call Doctor Within 24 Hours
- Fever over 102° F (39° C)
- You think your child needs to be seen, but the problem is not urgent
Call Doctor During Office Hours
- Sore throat lasts more than 48 hours
- Mother or other caregiver is pregnant
- You have other questions or concerns
Self Care at Home
- Fifth disease suspected
Care Advice for Fifth Disease
-
What You Should Know About Fifth Disease:
- It is a viral rash that is harmless.
- It does not itch or hurt.
- It can be treated at home.
- Here is some care advice that should help.
-
Fever Medicine:
- For fevers above 102° F (39° C), give an acetaminophen product (such as Tylenol).
- Another choice is an ibuprofen product (such as Advil).
- Note: Fevers less than 102° F (39° C) are important for fighting infections.
- For all fevers: Keep your child well hydrated. Give lots of cold fluids.
-
Pregnant Women - Special Risk:
- The risk of Fifth disease is to the unborn babies of pregnant women. It is not harmful to the woman herself.
- A pregnant woman should see her doctor if she is exposed.
- He will do a test to see if the mother has had the disease. If she has, she is protected.
- If not, the pregnancy will need to be watched closely. Some babies that get it before birth can have problems. Ten percent can have a very low red blood cell count and 2% may die.
- But, birth defects are never a result of this virus.
-
What to Expect:
- The lace-like rash can come and go for 1 to 3 weeks.
-
Return to School:
- Once your child has the "slapped cheeks", they can no longer spread the illness. Also, the lacy rash cannot be spread to others either.
- Your child does not need to stay home from child care or school.
- It can be spread during the week before the rash begins.
- Exposed children should try not to have any contact with pregnant women. This may be hard to know ahead of time.
-
Call Your Doctor If:
- Fever above 102° F (39° C) occurs
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.
Finger Injury
Is this your child's symptom?
- Injuries to fingers
If NOT, try one of these:
Types of Finger Injuries
- Cuts, Scrapes (skinned knuckles) and Bruises. These are the most common injuries.
- Jammed Finger. The end of a straightened finger or thumb receives a blow. Most often, this is from a ball. The energy is absorbed by the joint surface and the injury occurs there. This is called traumatic arthritis. For jammed fingers, always check that the fingertip can be fully straightened.
- Crushed or Smashed Fingertip. Most often, this is from a car door or a screen door. The end of the finger may get a few cuts or a blood blister. Sometimes, the nail can be damaged. Broken bones are not common with this kind of injury. If they do occur, they are at risk for a bone infection (osteomyelitis).
- Fingernail Injury. If the nailbed is cut, it needs sutures to prevent a deformed fingernail.
- Subungual Hematoma (Blood Clot under the Nail). Most often caused by a crush injury. This can be from a door crushing the finger. It can also be from a heavy object falling on the nailbed. Many are only mildly painful. Some are severely painful and throbbing. These need the pressure under the nail released. A doctor can put a small hole through the nail. This can relieve the pain and prevent loss of the fingernail.
- Dislocations. The finger has been pushed out of its joint.
- Fractures. Finger has a broken bone.
Pain Scale
- Mild: your child feels pain and tells you about it. But, the pain does not keep your child from any normal activities. School, play and sleep are not changed.
- Moderate: the pain keeps your child from doing some normal activities. It may wake him or her up from sleep.
- Severe: the pain is very bad. It keeps your child from doing all normal activities.
When to Call for Finger Injury
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Self Care at Home
|
Call Doctor or Seek Care Now
- Skin is split open or gaping and may need stitches
- Large swelling is present
- Blood under a nail is causing more than mild pain
- Fingernail is torn off
- Base of nail has popped out from under the skin fold
- Cut over knuckle of hand
- Dirt in the wound is not gone after 15 minutes of scrubbing
- Can't open and close the hand or use the fingers normally
- Severe pain and not better 2 hours after taking pain medicine
- Age less than 1 year old
- You think your child has a serious injury
- You think your child needs to be seen, and the problem is urgent
Call Doctor Within 24 Hours
- You think your child needs to be seen, but the problem is not urgent
Call Doctor During Office Hours
- Dirty cut and no tetanus shot in more than 5 years
- Clean cut and no tetanus shot in more than 10 years
- Pain not better after 3 days
- Not using the finger normally after 2 weeks
- You have other questions or concerns
Self Care at Home
- Minor finger injury
Care Advice for Minor Finger Injuries
-
What You Should Know About Finger Injuries:
- There are many ways that children can hurt their fingers.
- There are also many types of finger injuries.
- You can treat minor finger injuries at home.
- Here is some care advice that should help.
-
Pain Medicine:
- To help with the pain, give an acetaminophen product (such as Tylenol).
- Another choice is an ibuprofen product (such as Advil).
- Use as needed.
-
Bruised/Swollen Finger:
- Soak in cold water for 20 minutes.
- Repeat as needed.
-
Small Cuts or Scratches:
- For any bleeding, put direct pressure on the wound. Use a gauze pad or clean cloth. Press down firmly on the place that is bleeding for 10 minutes. This is the best way to stop bleeding. Keep using pressure until the bleeding stops.
- Wash the wound with soap and water for 5 minutes.
- For any dirt in the wound, scrub gently.
- For any cuts, use an antibiotic ointment (such as Polysporin). No prescription is needed.
- Cover it with a bandage (such as Band-Aid). Change daily.
-
Jammed Finger:
- Caution: Be certain range of motion is normal. Your child should be able to bend and straighten each finger. If movement is limited, your doctor must check for a broken bone.
- Soak the hand in cold water for 20 minutes.
- If the pain is more than mild, "buddy-tape" it to the next finger.
-
Smashed or Crushed Fingertip:
- Wash the finger with soap and water for 5 minutes.
- For any cuts, use an antibiotic ointment (such as Polysporin). No prescription is needed.
- Cover it with a bandage (such as Band-Aid).
-
Torn Nail (from catching it on something):
- For a cracked nail without rough edges, leave it alone.
- For a large flap of nail that's almost torn through, cut it off. Use a pair of scissors that have been cleaned. Cut along the line of the tear. Reason: Pieces of nail taped in place will catch on objects.
- Soak the finger for 20 minutes in cold water for pain relief.
- Use an antibiotic ointment (such as Polysporin). No prescription is needed. Then cover with a bandage (such as Band-Aid). Change daily.
- After about 7 days, the nailbed should be covered by new skin. It should no longer hurt. A new nail will grow in over 6 to 8 weeks.
-
Call Your Doctor If:
- Pain becomes severe
- Pain not better after 3 days
- Finger not normal after 2 weeks
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.

- Apply direct pressure to the entire wound with a sterile gauze dressing or a clean cloth.
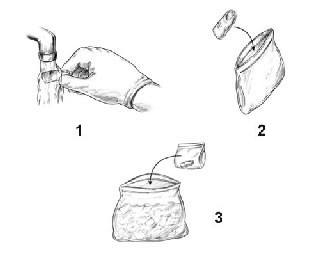
- Step 1: Briefly rinse amputated part with water (to remove any dirt)
- Step 2: Place amputated part in plastic bag (to protect and keep clean)
- Step 3: Place plastic bag containing the part in a container of ice (to keep cool and preserve tissue).
Note: Take patient and amputated part to emergency department immediately.
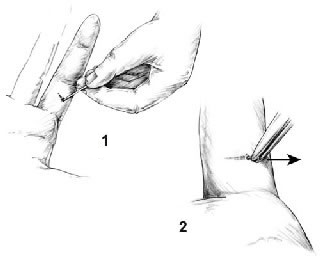
You can remove splinters, larger slivers, and thorns with a needle and tweezers. Check the tweezers beforehand to be certain the ends (pickups) meet exactly. (If they do not, bend them.) Sterilize the tools with rubbing alcohol or a flame.
Clean the skin surrounding the sliver briefly with rubbing alcohol before trying to remove it. Be careful not to push the splinter in deeper. If you don't have rubbing alcohol, use soap and water, but don't soak the area if FB is wood (Reason: can cause swelling of the splinter).
Remove the splinter:
- Step 1: Use the needle to completely expose the large end of the sliver. Use good lighting. A magnifying glass may help.
- Step 2: Then grasp the end firmly with the tweezers and pull it out at the same angle that it went in. Getting a good grip the first time is especially important with slivers that go in perpendicular to the skin or those trapped under the fingernail.
Fire Ant Sting
Is this your child's symptom?
- Stung by a fire ant
- Fire ant stings are more common in the Southern U.S.
If NOT, try one of these:
Local Skin Reactions to the Sting
- The main symptoms are pain, burning, swelling and redness at the sting site.
- Pain. Pain and burning at the site usually lasts 10 minutes. The pain is far less than that of a bee sting.
- Itching. Itching follows the pain and can last for weeks.
- Hive. Hive-like bump occurs at sting site within 30 minutes (100%). This looks like a red spot with raised white center.
- Pimples. Pimples with yellow fluid (pustules) occur at the sting site within 24 hours (96%). These pimples are almost diagnostic for fire ant stings. They are very itchy. They usually open on their own by 3 days. Then, they dry over. Sometimes, they can last for up to a week.
- Normal Swelling. Normal swelling from venom can increase for 24 hours after the sting. Stings of the upper face can cause severe swelling around the eye. This is harmless.
- Severe Swelling. Sometimes, fire ant bites can cause severe swelling. Hand or foot bites can cause swelling that crosses the wrist (or ankle). The degree of swelling can interfere with function and need steroids. These do not carry an increased risk of allergic reaction with future stings.
- Redness. Stings can become red. This is normal. That doesn't mean they are infected. Infections rarely occur in stings.
Anaphylactic Reaction to the Sting
- A severe life-threatening allergic reaction is called anaphylaxis.
- The main symptoms are hives with trouble breathing and swallowing. It starts within 2 hours of the sting.
- This severe reaction to fire ant stings happens in 1 to 2% of children.
- Hives. After fire ant stings, some children just develop hives all over or face swelling. Hives or face swelling alone may be able to be treated at home. But, at times, these symptoms can also lead to anaphylaxis. Be sure to call your doctor now to help decide.
Cause of Fire Ant Sting Reactions
- The ant's stinger injects venom into the skin.
- The venom is what causes all the symptoms.
- A fire ant attaches to the skin with its jaws and swivels its body. It stings multiple times with its back stinger.
- One fire ant can leave a semi-circular pattern of more than one sting.
General Information About Fire Ants
- In infested areas, fire ants cause many more stings than bees or yellow jackets.
- Over 50% of people living in these areas are stung each year.
- Fire ants are found throughout the Southern U.S., from Florida to Texas. They have also appeared in California, New Mexico and Arizona.
- Colonies of fire ants live in small mounds of dirt, usually 6 inches tall.
- When the mound is disturbed, hundreds of fire ants stream out and attack.
- The fire ant causes a "burning" feeling at the site of the stings. This is how it got its name.
Prevention of Fire Ant Stings
- The only way to prevent fire ant stings is to avoid their colonies.
- Teach your children to know their colonies (mounds) and to keep their distance.
- Insect repellents (including those that have DEET) don't help to prevent fire ant stings.
- Wear socks. Fire ants cannot bite through socks.
When to Call for Fire Ant Sting
Call 911 Now
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Self Care at Home
|
Call 911 Now
- Past severe allergic reaction to fire ant stings (not just hives) and stung less than 2 hours ago
- Wheezing or trouble breathing
- Hoarseness, cough or tightness in the throat or chest
- Trouble swallowing or drooling
- Speech is slurred
- Acts or talks confused
- Passed out (fainted) or too weak to stand
- You think your child has a life-threatening emergency
Call Doctor or Seek Care Now
- Sting inside the mouth
- Sting on the eye
- Stomach pain or vomiting
- Age less than 1 year with 20 or more stings. Newborn if more than 5.
- More than 5 stings for 10 pounds (5 kg) of weight. In teens, more than 50 stings.
- Fever and sting looks infected (spreading redness)
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Call Doctor Within 24 Hours
- Painful spreading redness started more than 24 hours after the bite. Note: any redness starting in the first 24 hours is a reaction to the bite.
- More than 48 hours since the sting and redness getting larger
- Swelling is huge (4 inches or 10 cm). It spreads across a joint such as the wrist.
- You think your child needs to be seen, but the problem is not urgent
Call Doctor During Office Hours
- Scab that looks infected (drains pus or gets bigger) not better with antibiotic ointment
- Severe itching not better after 24 hours of using steroid cream
- You have other questions or concerns
Self Care at Home
- Normal reaction to a fire ant sting
Care Advice for Fire Ant Stings
-
What You Should Know About Fire Ant Stings:
- Pain from a fire ant sting is less severe than with a bee sting. Most often, it's gone in 10 minutes.
- Fire ant stings form a pimple and become red. This is normal. That doesn't mean they are infected.
- Here is some care advice that should help.
-
Pain Medicine:
- To help with the pain, give an acetaminophen product (such as Tylenol).
- Another choice is an ibuprofen product (such as Advil).
- Use as needed.
-
Steroid Cream for Itching:
- For relief of itching, use 1% hydrocortisone cream (such as Cortaid). Use 3 times per day. No prescription is needed.
-
Allergy Medicine for Itching:
- For severe itching or swelling, give Benadryl by mouth. No prescription is needed.
- Use 3 times per day as needed.
-
Pustules (Pimples) - Do Not Open:
- By 24 hours, a small blister will form over the sting.
- Do not open them.
- Try not to scratch them.
- If you open the blisters, they often become infected.
- Left alone, they will most likely dry up in 4 days.
-
Antibiotic Ointment:
- If the pimples break open, use an antibiotic ointment (such as Polysporin.) No prescription is needed.
- Use 3 times per day to prevent skin infections. Keep using it for 1 or 2 days.
-
What to Expect:
- Severe pain or burning at the site lasts 5 to 10 minutes.
- Itching follows the pain and is the main symptom. It can last a week.
- Swelling: Normal swelling from ant venom can increase for 24 hours after the sting.
- The redness can last 3 days and the swelling 7 days.
-
Call Your Doctor If:
- Redness lasts over 3 days
- Swelling becomes huge or spreads past the wrist or ankle
- Sting begins to look infected (redness gets larger after 48 hours)
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.
Flu
Is this your child's symptom?
- Your child has symptoms of influenza (Flu) and it's in your community
- Main symptoms: fever AND one or more respiratory symptoms (cough, sore throat, very runny nose)
- Influenza (Flu) is a viral infection
- You think your child has influenza because other family members have it
- You think your child has influenza because close friends have it
If NOT, try one of these:
Symptoms of Influenza
- Main symptoms are a fever with a runny nose, sore throat, and bad cough.
- More muscle pain, headache, fever, and chills than with usual colds.
- If there is no fever, your child probably doesn't have flu. More likely he has a cold.
Cause of Influenza
- Influenza viruses that change yearly
Diagnosis: How to Know Your Child Has Influenza
- Influenza occurs every year in the fall and winter months. During this time, if flu symptoms occur, your child probably has the flu.
- Your child doesn't need any special tests.
- Call your doctor if your child is High-Risk for complications of the flu. See the list below. These are the children who may need prescription anti-viral drugs.
- For Low-Risk children, usually you don't need to see your child's doctor. If your child develops a possible complication of the flu, then call your doctor. See the "What to Do" section.
High-Risk Children for Complications From Influenza (AAP)
Children are considered High-Risk for complications if they have any of the following:
- Lung disease (such as asthma)
- Heart disease (such as a congenital heart disease)
- Cancer or weak immune system conditions
- Neuromuscular disease (such as muscular dystrophy)
- Diabetes, sickle cell disease, kidney disease or liver disease
- Diseases needing long-term aspirin therapy
- Pregnancy or severe obesity
- Healthy children under 2 years old are also considered High-Risk (CDC)
- Note: All other children are referred to as Low-Risk
Prescription Antiviral Drugs for Influenza
- Antiviral drugs (such as Tamiflu) are sometimes used to treat influenza. They must be started within 48 hours when the flu symptoms start. After 48 hours of fever, starting the drug is not helpful.
- The AAP recommends they be used for any patient with severe symptoms.
- The AAP recommends the drugs for most High-Risk children with underlying health problems. See that list.
- The AAP doesn't recommend antiviral drugs for Low-Risk children with mild flu symptoms.
- Their benefits are limited. They usually reduce the time your child is sick by 1 to 1.5 days. They reduce the symptoms, but do not make them go away.
- Side effects: Vomiting in 10% of children on Tamiflu.
- Most healthy children with flu do not need an antiviral drug.
When to Call for Flu
Call 911 Now
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Self Care at Home
|
Call 911 Now
- Severe trouble breathing (struggling for each breath, can barely speak or cry)
- Lips or face are bluish when not coughing
- You think your child has a life-threatening emergency
Call Doctor or Seek Care Now
- Trouble breathing. Exception: present only when coughing.
- Breathing is much faster than normal
- Lips or face have turned bluish during coughing
- Wheezing (high-pitched purring or whistling sound when breathing out)
- Stridor (harsh sound with breathing in) is heard now
- Ribs are pulling in with each breath (retractions)
- Chest pain and can't take a deep breath
- Dehydration suspected. No urine in more than 8 hours, dark urine, very dry mouth and no tears.
- Not alert when awake ("out of it")
- Weak immune system. Examples are: sickle cell disease, HIV, cancer, organ transplant, taking oral steroids.
- Severe High-Risk child (see that list in Causes). This includes lung disease, heart disease, and bedridden.
- Age less than 12 weeks old with fever. Caution: do NOT give your baby any fever medicine before being seen.
- Fever over 104° F (40° C)
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Call Doctor Within 24 Hours
- High-Risk child for complications of flu. Includes children with other chronic diseases. (See that list in Causes). Also, includes healthy children less than 2 years old.
- Nonstop coughing spells
- Age less than 3 months old with any cough
- Earache or ear drainage
- Sinus pain (not just congestion)
- Fever lasts more than 3 days
- Fever returns after being gone more than 24 hours
- You think your child needs to be seen, but the problem is not urgent
Call Doctor During Office Hours
- Age more than 6 months and needs a flu shot
- Coughing causes vomiting 3 or more times
- Coughing has kept home from school for 3 or more days
- Nasal discharge lasts more than 2 weeks
- Cough lasts more than 3 weeks
- Flu symptoms lasts more than 3 weeks
- You have other questions or concerns
Self Care at Home
- Influenza with no complications and your child is Low-Risk
Care Advice for Influenza
-
What You Should Know About Influenza:
- Flu symptoms include cough, sore throat, runny nose, and fever. During influenza season, if your child has these symptoms, he probably has the flu.
- Most parents know if their child has flu. They have it too or it's in the school. It's also in the news. You don't need any special tests when you think your child has flu.
- If your child develops a complication of the flu, then call your child's doctor. Examples are an earache or trouble breathing. These problems are included in the "What to Do" section.
- For healthy people, the symptoms of influenza are like those of a bad cold.
- With flu, however, the onset is more abrupt. The symptoms are more severe. Feeling very sick for the first 3 days is common.
- The treatment of influenza depends on your child's main symptoms. It is no different from treatment used for other viral colds and coughs.
- Bed rest is not needed.
- Most children with flu don't need to see their doctor.
- Here is some care advice that should help.
-
Runny Nose with Lots of Discharge: Blow or Suction the Nose
- The nasal mucus and discharge is washing germs out of the nose and sinuses.
- Blowing the nose is all that's needed. Teach your child how to blow the nose at age 2 or 3.
- For younger children, gently suction the nose with a suction bulb.
- Put petroleum jelly on the skin under the nose. Wash the skin first with warm water. This will help to protect the nostrils from any redness.
-
Nasal Saline To Open a Blocked Nose:
- Use saline (salt water) nose spray to loosen up the dried mucus. If you don't have saline, you can use a few drops of water. Use distilled water, bottled water or boiled tap water.
- Step 1. Put 3 drops in each nostril. If under 1 year old, use 1 drop.
- Step 2. Blow (or suction) each nostril out while closing off the other nostril. Then, do the other side.
- Step 3. Repeat nose drops and blowing (or suctioning) until the discharge is clear.
- How Often. Do nasal saline rinses when your child can't breathe through the nose.
- Limit. If under 1 year old, no more than 4 times per day or before every feeding.
- Saline nose drops or spray can be bought in any drugstore. No prescription is needed.
- Saline nose drops can also be made at home. Use ½ teaspoon (2 mL) of table salt. Stir the salt into 1 cup (8 ounces or 240 mL) of warm water. Use bottled water or boiled water to make saline nose drops.
- Reason for nose drops: Suction or blowing alone can't remove dried or sticky mucus. Also, babies can't nurse or drink from a bottle unless the nose is open.
- Other option: use a warm shower to loosen mucus. Breathe in the moist air, then blow each nostril.
- For young children, can also use a wet cotton swab to remove sticky mucus.
-
Medicines for Flu:
- Cold Medicines. Don't give any drugstore cold or cough medicines to young children. They are not approved by the FDA under 6 years. Reasons: not safe and can cause serious side effects. Also, they are not helpful. They can't remove dried mucus from the nose. Nasal saline works best.
- Allergy Medicines. They are not helpful, unless your child also has nasal allergies. They can also help an allergic cough.
- No Antibiotics. Antibiotics are not helpful for flu. Antibiotics may be used if your child gets an ear or sinus infection.
-
Homemade Cough Medicine:
- Goal: Decrease the irritation or tickle in the throat that causes a dry cough.
- Age 3 months to 1 year: give warm clear fluids to treat the cough. Examples are apple juice and lemonade. Amount: use a dose of 1-3 teaspoons (5-15 mL). Give 4 times per day when coughing. Caution: do not use honey until 1 year old.
- Age 1 year and older: use Honey ½ to 1 teaspoon (2-5 mL) as needed. It works as a homemade cough medicine. It can thin the secretions and loosen the cough. If you don't have any honey, you can use corn syrup.
- Age 6 years and older: use Cough Drops to decrease the tickle in the throat. If you don't have any, you can use hard candy. Avoid cough drops before 6 years. Reason: risk of choking.
-
Sore Throat Pain Relief:
- Age over 1 year. Can sip warm fluids such as chicken broth or apple juice. Some children prefer cold foods such as popsicles or ice cream.
- Age over 6 years. Can also suck on hard candy or lollipops. Butterscotch seems to help.
- Age over 8 years. Can also gargle. Use warm water with a little table salt added. A liquid antacid can be added instead of salt. Use Mylanta or the store brand. No prescription is needed.
- Medicated throat sprays or lozenges are generally not helpful.
-
Fluids - Offer More:
- Try to get your child to drink lots of fluids.
- Goal: Keep your child well hydrated.
- It also will thin out the mucus discharge from the nose.
- It also loosens up any phlegm in the lungs. Then it's easier to cough up.
-
Fever Medicine:
- For fevers above 102° F (39° C), give an acetaminophen product (such as Tylenol).
- Another choice is an ibuprofen product (such as Advil).
- Avoid Aspirin because of the strong link with Reye syndrome.
- Note: Fevers less than 102° F (39° C) are important for fighting infections.
- For all fevers: Keep your child well hydrated. Give lots of cold fluids.
-
Pain Medicine:
- For muscle aches or headaches, give an acetaminophen product (such as Tylenol).
- Another choice is an ibuprofen product (such as Advil).
- Use as needed.
-
Prescription Antiviral Drugs for Influenza:
- Antiviral drugs (such as Tamiflu) are sometimes used to treat influenza. They must be started within 48 hours of when flu symptoms start. After 48 hours of fever, starting the drug is not helpful.
- The AAP recommends they be used for any patient with severe symptoms. They also recommend the drugs for most High-Risk children. See that list in Causes.
- If your child has a chronic disease and gets the flu, call your doctor. The doctor will decide if your child needs a prescription.
- The AAP doesn't recommend antiviral drugs for Low-Risk children with normal flu symptoms.
- Their benefits are limited. They reduce the time your child is sick by 1 to 1 ½ days. They reduce the symptoms, but do not make them go away.
- Side effects: Vomiting in 10% of children on Tamiflu.
- Most healthy children with flu do not need an antiviral drug.
- Also, it is not used to prevent flu. Reason: You would need to take the medicine every day for months.
-
Return to School:
- Spread is rapid, and the virus is easily passed to others.
- The time it takes to get the flu after contact is about 2 days.
- Your child can return to school after the fever is gone for 24 hours.
- Your child should feel well enough to join in normal activities.
-
What to Expect:
- Influenza causes a cough that lasts 2 to 3 weeks.
- Sometimes your child will cough up lots of phlegm (mucus). The mucus can be grey, yellow or green. This is normal.
- Coughing up mucus is very important. It helps protect the lungs from pneumonia.
- We want to help a productive cough, not turn it off.
- The fever lasts 2 to 3 days.
- The runny nose lasts 7 to 14 days.
-
Prevention: How to Protect Yourself from Getting Sick:
- Wash hands often with soap and water.
- Alcohol-based hand cleaners also work well.
- Avoid touching the eyes, nose or mouth. Germs on the hands can spread this way.
- Try to avoid close contact with sick people.
- Avoid ERs and urgent care clinics if you don't need to go. These are places where you are more likely to be exposed to flu.
-
Prevention: How to Protect Others - Stay Home When Sick:
- Cover the nose and mouth with a tissue when coughing or sneezing.
- Wash hands often with soap and water. After coughing or sneezing are important times.
- Limit contact with others to keep from infecting them.
- Stay home from school for at least 24 hours after the fever is gone. (CDC).
-
Flu Shot and Prevention:
- Getting a flu shot is the best way to protect your family from flu.
- Influenza vaccines are strongly advised for all children over 6 months of age. (AAP)
- Adults should also get the shot.
- The shot most often prevents the disease.
- Even if your child gets the flu, the shot helps to reduce the symptoms.
- A new flu shot is needed every year. Reason: Flu viruses keep changing.
- After the flu shot, it takes 2 weeks to fully protect from flu. But then, the protection lasts for the full flu season. An antiviral medicine only protects from flu while taking it.
-
Call Your Doctor If:
- Trouble breathing occurs
- Retractions (pulling in between the ribs) occur
- Dehydration occurs
- Earache or sinus pain occurs
- Fever lasts more than 3 days or goes above 104° F (40° C)
- Nasal discharge lasts more than 14 days
- Cough lasts more than 3 weeks
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.
Fluid Intake Decreased
Is this your child's symptom?
- Drinking less than normal amounts of fluid
If NOT, try one of these:
Causes For Drinking Less Fluid Than Normal
- Sore Throat. A sore throat is the most common cause. The pain is made worse by swallowing. Most sore throats are caused by a virus. Strep bacteria cause 20% of sore throats with fever.
- Mouth Ulcers. Mouth ulcers are another common cause of a painful mouth. The pain is made worse by swallowing. Most mouth ulcers are caused by a virus (such as Coxsackie virus).
- Nausea. Nausea means a sick stomach feeling and loss of appetite. Also called an upset stomach, but without vomiting. Usually from a viral infection of the stomach or liver.
- Blocked Nose. A common cause in bottle or breastfed infant. Reason: if nose is clogged, the baby can't breathe while sucking.
- Trouble Breathing (Serious). Shortness of breath from any lung disease can reduce fluid intake. Examples are pneumonia, wheezing or severe croup. Reason: the baby quickly gets tired from sucking and breathing at the same time.
- Foreign Object in the Esophagus (Serious). The esophagus is the tube from the mouth to the stomach. A swallowed foreign object can become stuck here. Examples are coins or small toy parts. The main symptoms are gagging, refusal of fluids or drooling. The peak age is 1 to 3 years.
- Abscess of Tonsil (Serious). A bacterial infection of the tonsil can spread to the surrounding tissues. The main symptoms are severe trouble swallowing, fever and one-sided throat pain. It's also hard to fully open the mouth. The peak age is teens.
Dehydration: How to Tell
The main risk of not drinking enough fluids is dehydration. This means the body has lost too much water. It is a reason to see a doctor right away. Your child may have dehydration if not drinking much fluid and:
- The urine is dark yellow and has not passed any in more than 8 hours.
- Inside of the mouth and tongue are dry.
- There are no tears if your child cries.
- Slow blood refill test: longer than 2 seconds. First, press on the thumbnail and make it pale. Then let go. Count the seconds it takes for the nail to turn pink again. Ask your doctor to teach you how to do this test.
- A child with severe dehydration becomes too weak to stand. They can also be very dizzy when trying to stand.
When to Call for Fluid Intake Decreased
Call 911 Now
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Self Care at Home
|
Call 911 Now
- Not moving or very weak
- You think your child has a life-threatening emergency
Call Doctor or Seek Care Now
- Too weak to suck or drink
- Signs of dehydration, such as:
- Has not passed urine in more than 8 hours
- Crying does not cause tears
- Very dry mouth
- Sunken soft spot
- Sleepy child
- Will not drink or drinks very little for more than 8 hours
- Will not drink and new onset of drooling
- Trouble breathing
- Can't move neck normally
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Call Doctor Within 24 Hours
- Poor drinking and also has fever
- Poor drinking lasts more than 3 days
- You think your child needs to be seen, but the problem is not urgent
Call Doctor During Office Hours
- You have other questions or concerns
Self Care at Home
- Drinking adequate amount of fluids and no signs of dehydration
Care Advice for Decreased Fluid Intake
-
What You Should Know About A Decreased Fluid Intake:
- Eating less solids during an illness is normal.
- Drinking less fluids is not.
- So far, your child does not have any signs of dehydration.
- Here are some tips to help increase fluid intake.
-
Fluids - Offer More:
- Give your child lots of their favorite liquid.
- Use fluids like chocolate milk, fruit drinks, water or even soft drinks. The type doesn't matter. The type only matters if your child has diarrhea or starts throwing up.
-
Solid Foods - Less Important:
- Don't worry about solid food intake.
- It's normal not to feel hungry or want to eat when sick.
- Preventing dehydration is the only thing that is important.
-
Sore Mouth Treatment:
- If the mouth is sore, give cold drinks.
- Do not use citrus juices.
- For babies, offer fluids in a cup, spoon or syringe rather than a bottle. Reason: The nipple may increase pain.
- To help with the pain, give an acetaminophen product (such as Tylenol). Another choice is an ibuprofen product (such as Advil). Use as needed.
-
Liquid Antacid for Mouth Pain (Age 1 Year and Older):
- For mouth pain, use a liquid antacid (such as Mylanta or the store brand). Give 4 times per day as needed. After meals often is a good time.
- Age 1 to 6 years. Put a few drops in the mouth. Can also put it on with a cotton swab.
- Age over 6 years. Use 1 teaspoon (5 mL) as a mouth wash. Keep it on the ulcers as long as possible. Then can spit it out or swallow it.
- Caution: Do not use regular mouth washes, because they sting.
-
Nasal Saline To Open a Blocked Nose:
- Use saline (salt water) nose spray to loosen up the dried mucus. If you don't have saline, you can use a few drops of water. Use distilled water, bottled water or boiled tap water.
- Step 1. Put 3 drops in each nostril. If under 1 year old, use 1 drop.
- Step 2. Blow (or suction) each nostril out while closing off the other nostril. Then, do the other side.
- Step 3. Repeat nose drops and blowing (or suctioning) until the discharge is clear.
- How Often. Do nasal saline rinses when your child can't breathe through the nose.
- Limit. If under 1 year old, no more than 4 times per day or before every feeding.
- Saline nose drops or spray can be bought in any drugstore. No prescription is needed.
- Saline nose drops can also be made at home. Use ½ teaspoon (2 mL) of table salt. Stir the salt into 1 cup (8 ounces or 240 mL) of warm water. Use bottled water or boiled water to make saline nose drops.
- Reason for nose drops: Suction or blowing alone can't remove dried or sticky mucus. Also, babies can't nurse or drink from a bottle unless the nose is open.
- Other option: use a warm shower to loosen mucus. Breathe in the moist air, then blow each nostril.
- For young children, can also use a wet cotton swab to remove sticky mucus.
-
For Shortness of Breath - Give Smaller Feedings:
- For trouble breathing, feed more often. Feed every ½ hour.
- Offer smaller amounts per feeding.
- Reason: This allows your baby to rest in between feedings.
-
Call Your Doctor If:
- Trouble swallowing gets worse
- Signs of dehydration occur
- Poor drinking lasts more than 3 days
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.
Food Allergy
Is this your child's symptom?
- Allergic reactions to foods
- The most common symptom is hives
- Questions about food allergies
- Oral Allergy Syndrome is also covered. The main symptom is mouth itching and swelling. The main triggers are raw fruits and veggies.
Symptoms of Food Allergies
- Hives all over and swelling of the face are the most common symptoms. Hives are raised pink bumps with pale centers (welts). They look like bug bites.
- Mouth itching and swelling
- Runny nose and coughing
- Vomiting and diarrhea
- Life-threatening allergic reactions also must have trouble breathing and/or swallowing. The medical name for this is anaphylaxis. Most of these reactions have a sudden onset within 10 to 20 minutes. All occur within 2 hours of eating a certain food. People who have had this carry an emergency kit like an Epi-Pen.
Causes of Food Allergies
- 8 foods cause 90% of food allergies
- In the first year of life: cow's milk, soy milk and egg
- Older children: peanuts, tree nuts, fish, shellfish and wheat
- Shellfish include shrimp, crab, lobster, clams, oysters and scallops
- Tree nuts include all the nuts (such as almonds and cashews) except peanuts.
- Of children with a proven food allergy, 40% have severe reactions. The other 60% have mild reactions.
- Peanuts and tree nuts are the most common triggers for severe reactions.
Cross Reactions With Other Foods
Children with allergies listed below can react to other foods:
- Cow's milk allergy: 90% also react with goat's milk and 40% with soy milk
- Egg: 5% react with chicken
- Peanut: 5% react with other legumes (like peas or beans). About 30% also react to tree nuts.
- Tree nut : 40% react with other tree nuts
- Fish: 50% react with other fish. Only 10% also react to shellfish.
- Shellfish: 70% react with other shellfish
- Melon: 90% react with banana and avocado
How Long do Food Allergies Last?
- Cow's milk: 80% outgrown by age 16
- Soy milk: 80% by age 16
- Egg: 70% by age 16
- Peanut: 20% by age 16
- Tree nut: 10% by age 16
Allergic Disease - Can You Prevent with Diet?
- Most allergic diseases (food allergies, eczema and asthma) cannot be prevented.
- Helpful: Feeding only breastmilk for 4 months or longer
- Not helpful: Avoiding high-risk foods for pregnant or breastfeeding women
- Not helpful: Soy formulas instead of cow's milk formula
- Not helpful: A delay in starting baby foods past 6 months
- Not helpful: A delay in starting high-risk foods like peanut butter or eggs
- Source: AAP
Oral Allergy Syndrome (OAS)
- A minor reaction to some raw fruits and veggies
- Causes itching and swelling only to the lips and tongue
- Also called Pollen-Food Syndrome
Symptoms of OAS
- Rapid onset of itching (or tingling) and swelling of the mouth.
- This can involve the lips, tongue, throat, and roof of the mouth.
- The uvula (tag of tissue hanging down in back) can become very swollen.
- These symptoms follow eating a high risk raw fruit or veggie.
- OAS can start by age 5.
- Serious symptoms or very bad reactions rarely happen.
Causes of OAS
- A contact allergy. It only involves the parts of the mouth that touch the raw food.
- Trigger foods for OAS are always raw (not cooked.)
- Fresh Fruits. These include apple, apricot, banana, cherry, melons, orange, peach and pear.
- Raw Veggies. These include carrot, celery, parsley, potato and tomato. Carrots and celery have the highest risk for also causing serious symptoms.
- Certain Seeds. These include sunflower seeds and fennel seeds.
OAS and Nose Allergies Can Be Linked
- Over 50% of people who are allergic to pollen also have OAS. This means 10% of all people.
- Ragweed pollen allergy can cross-react with all melons. Also, sometimes with bananas and tomatoes.
- Birch pollen allergy can cross-react with raw potatoes, carrots, celery and apples.
- Grass pollen allergy can cross-react with tomato and kiwi.
When to Call for Food Allergy
Call 911 Now
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Self Care at Home
|
Call 911 Now
- Life-threatening allergic reaction to similar food in the past. Food eaten less than 2 hours ago.
- Trouble breathing or wheezing
- Hoarse voice or cough start all of a sudden
- Trouble swallowing, drooling or slurred speech start all of a sudden
- You think your child has a life-threatening emergency
Call Doctor or Seek Care Now
- Hives all over start 2 to 4 hours after eating high-risk food. High-risk foods include nuts, fish, shellfish, or eggs.
- Major face swelling (not just lips) starts 2 to 4 hours after eating high-risk food
- Vomiting or stomach cramps starts 2 to 4 hours after eating high-risk food
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Call Doctor Within 24 Hours
- Other symptoms that might be from a food allergy and present now
- You think your child needs to be seen, but the problem is not urgent
Call Doctor During Office Hours
- Recurrent symptoms that might be from a food allergy but not present now
- Oral Allergy Syndrome suspected but never confirmed by a doctor
- Food allergy diagnosed and you want to restart that food
- You have other questions or concerns
Self Care at Home
- Food allergy: mild reaction
- Oral allergy syndrome
Care Advice
Treatment of a Food Allergy
-
What You Should Know About Food Allergies:
- About 5% of children have food allergies.
- Most children with a new food reaction need to be seen.
- If your child is stable, hives often can be treated at home.
- Hives as the only symptom can have many causes.
- Your child can be seen later to decide future risks and best treatment.
- Here is some care advice that should help.
-
Benadryl:
- Give Benadryl 4 times per day for hives all over. No prescription is needed.
- If you only have another allergy med at home (but not Benadryl), use that. Follow the package directions.
- Use the Benadryl 4 times per day until the hives are gone for 12 hours.
- Caution: Do not use if age is under 1 year. Reason: Benadryl makes most children sleepy. Give your doctor a call for advice.
-
Cool Bath for Itching:
- To help with any itching, can also give a cool bath. Do this for 10 minutes.
- Caution: Do not cause a chill.
-
How to Prevent Future Reactions:
- Help your child avoid the food that caused the symptoms.
- Read labels on all food products fully.
- Tell other people who care for your child of your child's food allergy. Also, inform the staff at your child's school.
- Learn more at Food Allergy Research and Education.
-
What to Expect:
- Hives from foods often last just a short time.
- They often are gone in less than 6 hours.
-
Return to School:
- Hives cannot be spread to others.
- Your child can go back to school once feeling better. The hives shouldn't keep him from doing normal things.
-
Call Your Doctor If:
- Trouble breathing occurs
- Trouble swallowing or drooling occurs
- Severe hives not better after 2 doses of Benadryl
- Hives last over 24 hours
- You think your child needs to be seen
- Your child becomes worse
Treatment of Oral Allergy Syndrome Symptoms
-
What You Should Know:
- Oral Allergy Syndrome (OAS) is very common. It happens in 10% of people. Most of them also have pollen allergies.
- The symptoms are not harmful and can be treated at home.
- Needed for OAS: Your child has never had any serious symptoms with this food.
- OAS symptoms don't last very long.
- Here is some care advice that should help.
-
Rinse the Mouth:
- Rinse the lips and mouth with warm water. Do this a few times.
- Reason: To remove any traces of the food.
-
Cold Pack:
- Use ice or a cold pack to the swollen lips or tongue for 10 minutes.
- Reason: To lessen the swelling and the itch.
-
Benadryl:
- One dose of Benadryl may help the symptoms go away faster.
- No prescription is needed.
- If you only have another allergy med at home (but not Benadryl), use that. Follow the package directions.
-
How to Prevent Future OAS:
- Keep a list of the foods that cause your child's symptoms.
- Avoid these foods if they are raw (fresh).
- The cooked version of these foods usually won't cause any symptoms.
-
What to Expect:
- With or without treatment, the itching will go away in 1 to 2 hours.
- The mouth swelling will also go away quickly.
-
Call Your Doctor If:
- Trouble swallowing or drooling occurs
- Trouble breathing occurs
- Swelling or rash occurs anywhere else
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.
Frostbite
Is this your child's symptom?
- Frostbite is a cold injury to the skin
Symptoms of Frostbite
- Symptoms of mild frostbite (or frostnip) are cold, tingling and painful skin.
- True frostbite causes white, hard, numb skin. It can be serious. It always needs medical care after re-warming.
- Common sites are toes, fingers, tip of the nose, the outer ear or cheeks.
Cause of Frostbite
- The nerves, blood vessels and skin cells are frozen for a short time.
- The ears, nose, fingers, and toes are most often affected.
Frostbite Severity
Frostbite can be classified like burns:
- Frostnip (mild frostbite). Cold, tingling and painful skin. No skin changes after re-warming.
- 1st Degree. White and waxy (hard) while frozen. Mild redness and swelling after re-warming. No blisters.
- 2nd Degree. Same as 1st degree plus blisters after 24 hours.
- 3rd Degree. Blood-filled blisters leading to skin damage and scarring.
Hypothermia
- Frostbite and hypothermia are two different medical problems.
- Frostbite results from a cold injury to the skin. The body's core temperature can be normal.
- In contrast, hypothermia signals a marked decrease in the body's core temperature. Frostbite may or may not occur. Hypothermia is defined as a body temperature less than 95° F (35° C) rectally. It can be deadly without intervention.
Factors Leading to Frostbite
- Medical Conditions. Patients with diabetes, Raynaud's disease, and previous frostbite are all at greater risk.
- Type of Contact. Frostbite is made worse if the skin and clothing are wet. Touching bare hands to cold metal during freezing weather can cause frostbite right away.
- Time of Contact. The longer the exposure, the greater the heat loss and the chance of frostbite. The wind-chill index also plays a part in how quickly frostbite occurs.
When to Call for Frostbite
Call 911 Now
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Self Care at Home
|
Call 911 Now
- Can't wake up
- Speech is slurred
- Acts or talks confused
- Stumbling or falling
- Body temperature is less than 95° F (35° C) rectally
- Body temperature is less than 94° F (34.4° C) by mouth
- You think your child has a life-threatening emergency
Call Doctor or Seek Care Now
- You think your child has a serious injury
- White, hard, numb skin (before rewarming)
- Skin color and feeling does not return to normal after 1 hour of rewarming
- Severe shivering still present after re-warming and drying
- Severe pain still there after rewarming and taking pain medicine
- You think your child needs to be seen, and the problem is urgent
Call Doctor Within 24 Hours
- Frostbite skin gets blisters
- Blisters start to look infected (spreading redness or pus)
- You think your child needs to be seen, but the problem is not urgent
Call Doctor During Office Hours
- You have other questions or concerns
Self Care at Home
- Mild frostbite
Care Advice for Mild Frostbite
-
What You Should Know About Frostbite:
- Frostbite means the nerves and skin were frozen for a short time.
- Most frostbite is mild. Most often, it gets better with warming up.
- Here is some care advice that should help.
-
Rewarming With Wet Heat:
- Move into a warm room.
- For Frostbite of Fingers or Toes. Place the body part in warm water. A bathtub or sink is often the best method. The water should be very warm (104° to 108° F, or 40° to 42° C). It should not be hot enough to burn. Keep soaking in the warm water for about 30 minutes. A pink flush means circulation has returned to the body part. At this point, the numbness should be gone.
- For Frostbite of the Face (such as ears, nose). Put a warm wet washcloth on the area. You should keep doing this for about 30 minutes. A pink flush means circulation has returned to the area.
- With more severe frostbite, the last 10 minutes of rewarming can be painful.
- If not using a tub, keep the rest of your child's body warm. Cover with blankets.
-
Common Treatment Mistakes:
- A common mistake is to put snow on the frostbitten area or to rub it. Both can cause damage to thawing tissues.
- Do not re-warm with dry heat. Do not use heat lamps, heating pads or electric heaters. Reason: Skin that has frostbite can't sense burning.
- Do not re-warm if could freeze again in the next few hours. Freezing-warming-freezing causes more harm than freezing-warming.
-
Drink Warm Liquids:
- Have your child drink lots of warm liquids such as hot chocolate.
-
Ibuprofen For Pain:
- For true frostbite, give an ibuprofen product (such as Advil) for pain relief.
-
Aloe Vera Ointment for Pain:
- Put aloe vera ointment on the frostbite.
- Use twice daily for 5 days.
-
What to Expect:
- Frostnip does not cause any damage to the skin. After rewarming, skin feeling, color and softness come back in less than 1 hour.
- Mild frostbite: After rewarming, the skin may be flushed and tingly. This lasts for a few hours.
-
Prevention of Frostbite: (especially important in children with previous frostbite)
- Cold sensitivity and recurrent frostbite is common following severe frostbite.
- Dress in layers for cold weather. The first layer should be thermal underwear. The outer layer needs to be waterproof. The layers should be loose, not tight. Mittens are warmer than gloves. Do not use tight gloves or shoes. They might interfere with circulation.
- Wear a hat, because over 50% of heat loss occurs from the head.
- Change wet gloves or socks right away.
- Teach your child to know the first warning signs of frostbite. Tingling and numbness are signs to go indoors.
-
Call Your Doctor If:
- Color and feeling do not return to normal after 1 hour of re-warming
- Frostbite gets blisters
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.
Genital Injury - Female
Is this your child's symptom?
- Injuries to the female genital area (labia, vulva, vagina)
Types of Genital Injuries in Females
- The genital area in girls is protected. Serious injuries are rare.
- Minor injuries can cause lots of bleeding because of the rich blood supply.
- Cut. Minor cuts or scrapes heal quickly.
- Bruise. Bruises and swelling of the labia are most often from a straddle injury. They heal quickly.
- Hematoma (Blood Clot). Bleeding into the labia can form a pocket of blood (hematoma). A small clot will go away on its own. A large clot may need to be drained.
- Vaginal Laceration (Serious). Any penetrating injury of the vagina needs to be examined. There may be a cut or tear of the vagina. The main symptom is pain and bleeding that won't stop.
- Urethral Injury (Serious). This is not seen in females with external injuries. It can occur with pelvic fractures. The main symptoms are bloody urine and trouble passing urine.
Straddle Injuries
- An injury to the groin from falling on an object that is being straddled.
- Examples are playground equipment, crossbars of a bike, or a fence.
- Girls usually get a bruise or small cut of the outer labia. The vagina and urethra are protected by the labia and not harmed.
When to Call for Genital Injury - Female
Call 911 Now
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Self Care at Home
|
Call 911 Now
- Major bleeding that can't be stopped
- Fainted or too weak to stand
Call Doctor or Seek Care Now
- Skin bleeding won't stop after 10 minutes of direct pressure
- Bleeding from inside the vagina
- Pointed object was put in the vagina, then taken out
- Foreign object in the vagina and can't get out
- Skin is split open or gaping and may need stitches
- Pain or trouble passing urine
- Blood in urine
- Severe pain and not better 2 hours after taking pain medicine
- Age less than 1 year old
- Could have been caused by sexual abuse
- You think your child has a serious injury
- You think your child needs to be seen, and the problem is urgent
Call Doctor Within 24 Hours
- You think your child needs to be seen, but the problem is not urgent
Call Doctor During Office Hours
- Dirty cut and no tetanus shot in more than 5 years
- Clean cut and no tetanus shot in more than 10 years
- Genital pain or swelling lasts more than 7 days
- You have other questions or concerns
Self Care at Home
- Minor genital injury
Care Advice for Minor Genital Injuries
-
Bleeding - How to Stop:
- For any bleeding, put direct pressure on the wound. Use a gauze pad or clean cloth. Press for 10 minutes or until the bleeding has stopped.
- Note: Minor cuts in the genital area can bleed a lot. This is because of the rich blood supply.
- For the same reason, the cut heals quickly.
-
Cut or Scrape Treatment:
- Wash the wound with soap and water for 5 minutes.
- For any dirt, scrub gently with a wash cloth.
- Put on an antibiotic ointment (such as Polysporin). No prescription is needed. Use 2 times per day.
-
Cold Cloth for Bruise:
- For bruises or swelling, put a cold wet washcloth on the skin.
- Use once for 20 minutes, but only if tolerated.
- Reason: Helps reduce the bleeding and pain.
-
Pain Medicine:
- To help with the pain, give an acetaminophen product (such as Tylenol).
- Another choice is an ibuprofen product (such as Advil).
- Use as needed.
-
What to Expect:
- Cuts and other minor injuries in the genital area heal quickly. Most often, they heal in 3 or 4 days.
-
Call Your Doctor If:
- Pain becomes severe
- Passing urine becomes painful or hard to do
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.
Genital Injury - Male
Is this your child's symptom?
- Injuries to the male genital area (scrotum or penis)
Types of Genital Injuries in Males
- The penis and scrotum are exposed. In young boys, the scrotum is injured more often than the penis. All the common skin injuries can occur here.
- Cut. Minor cuts or scrapes heal quickly.
- Bruise. Minor bruises heal quickly.
- Zipper Injury. The foreskin or skin on the penis can get caught on a zipper. Most parents will want a doctor to help with removal.
- Urethral Injury (Serious). The urethra passes through the entire penis. It can be injured by a kick to the groin or a straddle injury. The urethra can be bruised or torn. The main symptoms are bloody urine and trouble passing urine.
- Painful Scrotum. A blow to the testicle will normally cause severe pain. If there was no damage, the pain should go away within 30 minutes. If it persists, the boy needs to be examined.
- Swollen Scrotum (Serious). Any boy with a swollen scrotum from an injury needs to be examined. It may be minor, but need to rule out any other problems.
- Hematoma (Blood Clot) of Scrotum. Blunt trauma can cause a large blood clot to form inside the scrotum. Sometimes, it needs to be drained. This can happen from being hit by a ball during sports. The main finding is severe pain and a swollen scrotum.
- Rupture of Testicle (Serious). A direct blow to the scrotum can also cause a tear of the capsule around the testicle. To save the testicle, this needs emergency surgery. This can happen from a kick to the groin. The main finding is severe pain and a swollen scrotum.
Straddle Injuries
- An injury to the groin from falling on an object that is being straddled.
- Examples are playground equipment, crossbars of a bike, or a fence.
- In boys with a straddle injury, the urethra can be bruised or torn. The urethra allows urine to pass from the bladder to the outside.
- A symptom of a damaged urethra is blood at the penis opening. Other findings are bloody urine, trouble starting the stream or pain when passing urine.
When to Call for Genital Injury - Male
Call 911 Now
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Self Care at Home
|
Call 911 Now
- Major bleeding that can't be stopped
- Fainted or too weak to stand
Call Doctor or Seek Care Now
- Skin is split open or gaping and may need stitches
- Swollen or painful scrotum
- Pain or trouble passing urine
- Blood in urine or at penis opening
- Severe pain and not better 2 hours after taking pain medicine
- Age less than 1 year old
- Could have been caused by sexual abuse
- You think your child has a serious injury
- You think your child needs to be seen, and the problem is urgent
Call Doctor Within 24 Hours
- You think your child needs to be seen, but the problem is not urgent
Call Doctor During Office Hours
- Dirty cut and no tetanus shot in more than 5 years
- Clean cut and no tetanus shot in more than 10 years
- Genital pain or swelling lasts more than 7 days
- You have other questions or concerns
Self Care at Home
- Minor genital injury
Care Advice for Minor Genital Injuries
-
Bleeding - How to Stop:
- For any bleeding, put direct pressure on the wound. Use a gauze pad or clean cloth. Press for 10 minutes or until the bleeding has stopped.
- Note: Minor cuts in the genital area can bleed a lot. This is because of the rich blood supply.
- For the same reason, the cut heals quickly.
-
Cut or Scrape Treatment:
- Wash the wound with soap and water for 5 minutes.
- For any dirt, scrub gently with a wash cloth.
- Put on an antibiotic ointment (such as Polysporin). No prescription is needed. Use 2 times per day.
-
Cold Cloth for Bruise:
- For bruises or swelling, put a cold wet washcloth on the skin.
- Use once for 20 minutes, but only if tolerated.
- Reason: Helps reduce the bleeding and pain.
-
Pain Medicine:
- To help with the pain, give an acetaminophen product (such as Tylenol).
- Another choice is an ibuprofen product (such as Advil).
- Use as needed.
-
What to Expect:
- Cuts and other minor injuries in the genital area heal quickly. Most often, they heal in 3 or 4 days.
-
Call Your Doctor If:
- Pain becomes severe
- Passing urine becomes painful or hard to do
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.
Hair Loss
Is this your child's symptom?
- Hair loss in patches or throughout the scalp
- The missing hairs can be broken off or just fall out
- The medical term for hair loss is alopecia
If NOT, try one of these:
Causes
Common causes of hair loss are listed below. Most don't usually require medical treatment.
- Ringworm of the Scalp. This is the main cause of patchy hair loss that needs medical treatment. Your child's doctor will prescribe a medicine to treat ringworm of the scalp. It's taken by mouth.
- Newborn Hair Loss. The hair of many newborns falls out during the first few months of life. This baby hair is replaced by permanent hair.
- Rubbing or Friction. Babies can rub off a patch of hair on the back of the head. This most commonly occurs in infant 3 to 6 months old. It is a result of friction during head-turning against a firm surface. Examples are crib mattresses, playpens, and infant seats. The hair grows back once the baby starts sitting up. Also called friction alopecia or pressure alopecia. Repeated or severe friction can cause hair loss at any age.
- Tight Hair Styles. If hair is pulled too tight, it will eventually break. Mostly seen with tight braids, pony tails or dreadlocks (especially corn row styles). Hair can also be lost because of vigorous hair-brushing or back combing. Hot hairstyling tools can also cause hair damage. Also known as traction alopecia, mechanical alopecia, or "hair abuse."
- Twisting or Pulling Out the Hair. This is a nervous habit called trichotillomania. Frequent twisting of the hair results in broken hairs of different lengths. The missing hair occurs in patches of different shapes. This creates bald spots. Rarely, it can include plucking of the eyebrows or eyelashes. Can occur with nail biting, lip biting or sucking, and sore picking habits. In older children, may be associated with OCD.
- Stress. Hair follicles are very sensitive to physical or emotional stress. The hair begins to fall out about 3-4 months after a severe stress. Reason: Hair follicles are very sensitive to physical or emotional stress. Examples are a high fever, severe illness or surgery. Also, an emotional crisis or a crash diet can be triggers. In pregnant teens, the stress can be childbirth. After hair stops shedding, the hair will slowly grow back. This can take 6 to 8 months for all the hair to grow back. The whole cycle takes about 12 months. This type of hair loss is called telogen effluvium.
When to Call for Hair Loss
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Self Care at Home
|
Call Doctor or Seek Care Now
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Call Doctor Within 24 Hours
- Scalp is red and very swollen in area of hair loss
- You think your child needs to be seen, but the problem is not urgent
Call Doctor During Office Hours
- Scabs or crusts are present in the hair
- Ringworm of the scalp suspected. (Round patch of hair loss with scales, rough surface, redness or itching)
- Broken hairs from tight hair style and pimples are present in scalp
- Patch of hair loss and cause not known
- Widespread hair thinning and cause not known
- Hair loss from nervous habit of twisting the hair (needs counseling)
- Hair loss is a chronic problem
- Normal hair loss suspected, but doesn't grow back within 6 months
- You have other questions or concerns
Self Care at Home
- Newborn normal hair loss in infancy
- Hair loss on back of head from chronic rubbing and friction
- Hair loss from tight hair style
- Widespread hair thinning follows a major stress about 3 months ago
Care Advice
Newborn Normal Hair Loss in Infancy
-
What You Should Know About Newborn Normal Hair Loss:
- Newborns are born with varying amounts of hair.
- The baby hair of many newborns falls out during the first 6 months of life. Hair loss peaks at 3 months old. The mother may also lose some of her hair at this time.
- This baby hair is then replaced by permanent hair.
- The normal hair comes in between 6 and 12 months.
- This shedding phase in newborns is always normal.
- Hair loss is not caused by shampoos.
-
Call Your Doctor If:
- Hair does not grow back by 12 months old
- You have other questions or concerns
Hair Loss on Back of Head from Chronic Rubbing and Friction
-
What You Should Know About Rubbing Off Hair on Back of Head:
- Babies can rub off a patch of hair on the back of the head. This most commonly occurs in infant 3 to 6 months old.
- The hair loss is from friction during head-turning against a firm surface. Examples are crib mattresses, playpens, activity mats and infant seats.
- The hair grows back once the baby starts to sit up.
- This may take 6 to 12 months.
- Can also occur in any bedridden child (e.g., severe cerebral palsy).
-
Treatment for Hair Loss from Friction and Too Much Time on Back:
- After 1 month old, give your baby more tummy time.
- Caution: Tummy time should always occur under adult supervision. Reason: Risk of suffocation until child reaches an age when can turn over.
- Tummy time has many benefits.
- It will help the back of head become more rounded and less flat.
- It will also build up strength in shoulder muscles.
-
Call Your Doctor If:
- Hair does not grow back by 6 months after learning to sit
- You have other questions or concerns
Hair Loss From Tight Hair Style
-
What You Should Know About Hair Loss from Tight Hair Style:
- Symptoms: Broken hairs are seen at the hairline or where the hair is parted. It's usually the same on both sides of the head.
- Cause: If hair is pulled too tight, it will eventually break. This gives a frizzy look from hairs broken off at various lengths.
- Examples: It's most commonly seen with tight braids, pony tails or dreadlocks. Hair can also be lost because of vigorous hair-brushing or back combing. Hot hairstyling tools can also cause hair damage. Can also occur during exercise while wearing head phones.
- Hair loss is not caused by shampoos.
-
Treatment of Broken Hairs from Tight Hair Style:
- Change the hair style to one that doesn't put tension on the hair.
- If that is not acceptable, loosen the ponytail or braids.
- These hair styles are at risk if they feel tight or cause any pain.
- Outcome: If tight hair styles are avoided, the hair will return to normal.
- Warning: If tight braiding continues over 10 years, permanent hair loss can occur.
-
Pimples in the Hair and on the Scalp:
- Cause: Most pimples are caused by blocked hair follicles.
- Treatment: Stop using any ointments or oils in the hair. Reason: they block the hair follicles.
- Stop any hair style that puts tension on the hair. Reason: damages the hair follicle and makes it prone to infection.
- Wash any ointment or greasy pomade off the scalp with soap and water.
- Antibiotic Cream: Apply an antibiotic cream to the pimples. Do not use ointment. Use it 2 times a day for 3 days. No prescription is needed.
- Outcome: Most pimples will clear up in 3 days.
-
Call Your Doctor If:
- Hair does not grow back by 6 months after hair style changed
- You have other questions or concerns
Widespread Hair Thinning Following Major Stress About 3 Months Ago
-
What You Should Know About Hair Loss after Stress:
- Symptoms: Lots of hair is noticed in a comb or brush. The hair falls out from all parts of the scalp. This leads to major thinning of the hair, but no bald spots.
- Cause: Severe stressful event. Hair follicles are very sensitive to physical or emotional stress. Examples are a high fever, severe illness or surgery. Also, an emotional crisis or a crash diet can be triggers. In pregnant teens, the stress can be childbirth. Hair loss is not caused by shampoos.
- Time Frame: The hair begins to fall out about 3-4 months after a severe stress. It continues to fall out excessively over the next 3 or 4 months. After hair stops shedding, the hair will slowly grow back. This can take 6 to 8 months for all the hair to grow back. The whole cycle takes about 12 months.
- There's no way to hurry the process. The hair growth cycle needs to run its course.
- Here is some care advice that should help.
-
Hair Care:
- Treat the hair gently.
- Wash the hair no more than once per day. Always use a hair conditioner.
- Comb the hair rather than brushing it.
- Be careful at combing out any tangled hair.
- Avoid any tight hair styles such as braids or a pony tail.
- Don't put tension on the hair.
- No special shampoo or cream is needed or helpful.
-
What to Expect:
- No more than 50% of the hair will be lost.
- Once it starts to regrow, all the hair will grow back in about 6 months.
- The new hair will look normal.
-
Call Your Doctor If:
- Hair does not grow back by 12 months after stressful event
- You have other questions or concerns
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.
Hand-Foot-And-Mouth Disease (HFMD)
Is this your child's symptom?
- Tiny red spots and water blisters on the hands and feet caused by a virus
- Rash is seen on the palms, fingers, soles and toes
- The diagnosis cannot be made without these
- Also can cause small mouth ulcers (sores)
If NOT, try one of these:
Symptoms of Hand-Foot-and-Mouth Disease (HFMD)
- Small red spots and tiny water blisters on the hands and feet. Seen on the palms, fingers, soles and toes.
- The diagnosis cannot be made without these.
- Small painful ulcers (sores) in the mouth. Look for them on the tongue and sides of mouth. Most children with HFMD have these, but they can be hard to see.
- Also, small blisters or red spots on the buttocks (30%)
- Low-grade fever less than 102° F (39° C)
- Mainly occurs in children age 6 months to 4 years
Cause of HFMD
- Coxsackie A-16 virus and other enteroviruses
- Not related to any animal disease
Severe Form of HFMD
- Since 2012, a severe form of HFMD has occurred in much of the world. It's caused by a new Coxsackie A6 virus.
- The rash spreads to the arms, legs and face. The rash is made up of many small blisters.
- Children with such a severe rash may need to be seen. Reason: to confirm the diagnosis. Exception: close contact with HFMD within the last 7 days.
- Treatment is the same. Drink enough fluids to prevent dehydration.
- Peeling of the fingers and toes is common. It looks bad but is harmless. It happens at 1 to 2 weeks. Use a moisturizing cream on the raw skin.
- Some fingernails and toenails may fall off. It occurs in 4% of severe cases. It happens at 3 to 6 weeks out. Trim them if they catch on things.
- Fingernails grow back by 3 to 6 months and toenails by 9 to 12 months. They will look normal.
When to Call for Hand-Foot-And-Mouth Disease (HFMD)
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Self Care at Home
|
Call Doctor or Seek Care Now
- Dehydration suspected. No urine in more than 8 hours, dark urine, very dry mouth and no tears.
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Call Doctor Within 24 Hours
- Red, swollen and tender gums
- Ulcers and sores also on the outer lip
- Rash spreads to the arms and legs (severe form of HFMD)
- Fever lasts more than 3 days
- You think your child needs to be seen, but the problem is not urgent
Call Doctor During Office Hours
- Fingernails or toenails fall off
- You have other questions or concerns
Self Care at Home
- Hand-foot-mouth disease and no other problems
Care Advice for Hand-Foot-and-Mouth Disease (HFMD)
-
What You Should Know About HFM Disease:
- Most often, hand-foot-and-mouth disease (HFMD) is a harmless rash.
- It is caused by a virus called Coxsackie.
- Here is some care advice that should help.
-
Liquid Antacid for Mouth Pain (Age 1 Year and Older):
- For mouth pain, use a liquid antacid (such as Mylanta or the store brand). Give 4 times per day as needed. After meals often is a good time.
- Age 1 to 6 years. Put a few drops in the mouth. Can also put it on the mouth sores with a cotton swab.
- Age over 6 years. Use 1 teaspoon (5 mL) as a mouth wash. Keep it on the ulcers as long as possible. Then can spit it out or swallow it.
- Caution: Do not use regular mouth washes, because they sting.
-
Fluids and Soft Diet:
- Try to get your child to drink adequate fluids.
- Goal: Keep your child well hydrated.
- Cold drinks, milk shakes, popsicles, slushes, and sherbet are good choices.
- Solid Foods. Offer a soft diet. Good ones are mac and cheese, mashed potatoes, cereals with milk and ice cream. Also, avoid foods that need much chewing. Do not give citrus, salty, or spicy foods. Note: Fluid intake is more important than eating any solids.
- For babies, you may need to stop the bottle. Give fluids by cup, spoon or syringe instead. Reason: The nipple can increase the pain.
-
Pain Medicine:
- Mouth sores are painful.
- Blisters also may be painful, especially on the feet.
- To help with the pain, give an acetaminophen product (such as Tylenol).
- Another choice is an ibuprofen product (such as Advil).
- Use as needed.
-
Fever Medicine:
- For fevers above 102° F (39° C), give an acetaminophen product (such as Tylenol).
- Another choice is an ibuprofen product (such as Advil).
- Note: Fevers less than 102° F (39° C) are important for fighting infections.
- For all fevers: Keep your child well hydrated. Give lots of cold fluids.
-
Blisters on the Skin
- Blisters don't need any special treatment. You can wash them like normal skin.
- Blisters on the palms and soles do not open.
- Those on arms and elsewhere sometimes open. The fluid is contagious to other people. Open blisters do not need to be covered. They quickly dry over.
-
Return to School:
- HFMD is easily spread to others.
- However, most often, it's a mild and harmless illness.
- After contact with HFMD, children come down with symptoms in 3-6 days.
- Can return to child care or school after the fever is gone. Most often, this takes 2 to 3 days.
- Children with widespread blisters may need to stay home until the blisters dry up. That takes about 7 days.
-
What to Expect:
- Fever lasts 2 or 3 days.
- Mouth sores should go away by 7 days.
- Rash on the hands and feet lasts 10 days. The rash on the hands and feet may then peel.
-
Call Your Doctor If:
- Signs of dehydration occur
- Fever lasts more than 3 days
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.

This is what hand foot and mouth disease looks like on the tongue. There are sores or blisters on the tongue. Make sure to wash hands often to prevent spreading the disease.

This shows the sores or blisters from hand foot and mouth disease on the foot. Make sure to wash hands often to prevent spreading the disease.
Hay Fever
Is this your child's symptom?
- An allergic reaction of the nose, usually from pollen
- An itchy nose, clear discharge and sneezing is common
If NOT, try one of these:
Triggers of Nasal Allergies
- Cause. An allergic reaction of the nose and sinuses to an inhaled substance. The medical name for this is allergic rhinitis. The allergic substance is called an allergen.
- Most allergens float in the air. That's how they get in the nose. Here are the common ones:
- Pollens. Trees, grass, weeds and molds are the most common pollens. Tree pollens come in the spring. Grass pollens come in the summer. Weed pollens come in the fall. Pollens cause seasonal allergies. You can't avoid pollens because they are in the air. Most nasal allergies continue through the pollen season. They can last 4 to 8 weeks. Pollens cause seasonal allergic rhinitis. This is also called hay fever.
- Pets. Allergens can also be from cats, dogs, horses, rabbits and other animals. Most people don't keep a pet that they are allergic to. They only have sporadic allergy symptoms when they are exposed to that specific animal. These symptoms will usually last a few hours. If someone with a cat visits you, they will bring cat dander with them. This will cause brief symptoms. If you own the pet, though, your child will have symptoms all the time.
- House Dust. House dust contains many allergens. It always contains dust mites. If your humidity is high, it will contain mold. House dust causes year round, daily symptoms. The medical name for this is perennial allergic rhinitis.
Symptoms of Nasal Allergies
- Clear nasal discharge with sneezing, sniffing, and itching of nose (100%)
- Eye allergies (itchy, red, watery and puffy) also can occur (70%)
- Ear and sinus congestion or fullness can occur
- Throat can also feel scratchy or have a tickly feeling at times
- Itchy ear canals, itchy skin or hoarse voice sometimes also occur
- Symptoms happen during pollen season
- Same symptoms during the same month of the last year
- Past diagnosis by a doctor is helpful
- No fever
How to Tell Seasonal Nasal Allergies from the Common Cold
- Symptoms happen during pollen season
- Had the same symptoms during the same month last year
- Hay fever symptoms last 6-8 weeks for each pollen. (Colds last 1-3 weeks).
- Allergies: itchy eyes and nose. Not seen with colds.
- Colds: fever and/or sore throat. Not seen with allergies
- Both: runny nose and watery eyes. Can also have a cough with both, but less common with allergies.
Nose and Eye Allergies: Age of Onset
- Seasonal pollen allergies usually begin at age 2 to 5 years.
- The symptoms peak in school age children, teens and young adults.
- Pollen symptoms are rare in children under age 2. They require at least 2 seasons of exposure to the pollen.
- Children under age 2 who have chronic nasal symptoms have other causes. Examples are recurrent colds, large adenoids or cow's milk allergy.
- Food allergies can start during the first year of life, but not pollen allergies.
When to Call for Hay Fever
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Self Care at Home
|
Call Doctor Within 24 Hours
- You think your child needs to be seen
- Lots of coughing
- Sinus pain (not just congestion) does not go away with allergy medicines. Note: sinus pain is around the cheekbone or eyes.
Call Doctor During Office Hours
- Hay fever symptoms make it hard to go to school or do normal activities. Note: taking allergy medicine for 2 days has not helped.
- Diagnosis of hay fever has never been made by a doctor
- Year-round symptoms of nasal allergies
- Snoring is a frequent problem
- You have other questions or concerns
Self Care at Home
- Nasal allergy symptoms or hay fever
Care Advice for Nose Allergies or Hay Fever
-
What You Should Know About Nose Allergies or Hay Fever:
- Hay fever is very common. It happens in about 15% of children.
- Nose and eye symptoms can be controlled by giving allergy medicines.
- Pollens are in the air every day during pollen season. So, allergy meds must be given daily. They need to be used for 2 months or longer during pollen season.
- Here is some care advice that should help.
-
Allergy Medicines:
- Allergy medicines are called antihistamines. They are the drug of choice for nasal allergies.
- They will help control the symptoms. These include a runny nose, nasal itching and sneezing.
- You can give a short-acting allergy medicine (such as Benadryl). No prescription is needed. It needs to be given every 6 to 8 hours.
- The bedtime dosage is especially important for healing the lining of the nose.
- The key to control is to give allergy meds every day during pollen season.
-
Long-Acting Allergy Medicines:
- You can also use a long-acting allergy medicine (such as Zyrtec). No prescription is needed.
- Advantage: Causes less sedation than older allergy meds such as Benadryl. It is long-acting and last up to 24 hours.
- Dose:
- Age 2-5 years old, discuss with your child's doctor. If approved, give 2.5 mg (2.5 mL or ½ teaspoon) of liquid syrup. Use once daily in the morning.
- Age 6-11 years old, give 5 mg chewable tablet once daily in morning.
- Age 12 years and older, give 10 mg tablet once daily in morning.
- Downside: Doesn't control hay fever symptoms as well as older allergy medicines. Also, sometimes will have breakthrough symptoms before 24 hours. If that happens, you can give a single dose of Benadryl.
- Cost: ask the pharmacist for a store brand. Reason: Costs less than the brand name products.
-
Nasal Saline to Wash Out Pollen:
- Use saline (salt water) nose drops or spray (such as store brand). This helps to wash out pollen or to loosen up dried mucus. If you don't have saline, you can use a few drops of water. Use bottled water, distilled water or boiled tap water. Teens can just splash a little water in the nose and then blow.
- Step 1: Put 3 drops in each nostril.
- Step 2: Blow each nostril out while closing off the other nostril. Then, do the other side.
- Step 3: Repeat nose drops and blowing until the discharge is clear.
- How often: Do nasal saline rinses when your child can't breathe through the nose. Also, do them if the nose is very itchy.
- Saline nose drops or spray can be bought in any drugstore. No prescription is needed.
- Saline nose drops can also be made at home. Use ½ teaspoon (2 mL) of table salt. Stir the salt into 1 cup (8 ounces or 240 mL) of warm water. Use bottled water or boiled water to make saline nose drops.
- Other option: Use a warm shower to loosen mucus. Breathe in the moist air, then blow each nostril.
-
Eye Allergy Treatment:
- For eye symptoms, wash off the face and eyelids. This will remove pollen or any other allergic substances.
- Then put a cold wet washcloth on the eyes.
- Most often, an allergy medicine given by mouth will help the eye symptoms. Sometimes, eye drops are also needed. (See below # 6 and #7)
-
Antihistamine Eye Drops - Ketotifen (1st Choice) for Eye Allergy Symptoms:
- Ketotifen eye drops (such as Zaditor) are a safe and effective product. No prescription is needed.
- Dose: 1 drop every 12 hours.
- For severe allergies, use ketotifen eyedrops every day during pollen season. This will give the best control.
-
Antihistamine/Vasoconstrictive Eye Drops (2nd Choice) for Eye Allergy Symptoms:
- Ask your pharmacist to suggest a brand (such as Visine-A). The A stands for antihistamine. No prescription is needed.
- Dose: 1 drop every 8 hours
- Do not use for over 5 days. Reason: Will cause red eyes from rebound effect.
- Downside: Doesn't work as well as Ketotifen eye drops.
-
Wash Pollen Off Body:
- Remove pollen from the hair and skin with shampoo and a shower. This is especially important before bedtime.
-
What to Expect:
- Since pollen allergies recur each year, learn to control the symptoms.
-
Pollen - How to Reduce the Pollen Your Child Breathes:
- Pollen is carried in the air.
- Keep windows closed in the home, at least in your child's bedroom.
- Keep windows closed in car. Turn the air conditioner on recirculate.
- Avoid window fans or attic fans. They pull in pollen.
- Try to stay indoors on windy days. Reason: The pollen count is much higher when it's dry and windy.
- Avoid playing with the outdoor dog. Reason: Pollen collects in the fur.
- Pollen Count: You can get your daily pollen count from Pollen.com. Just type in your zip code.
-
Call Your Doctor If:
- Symptoms are not better in 2 days after starting allergy medicine
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.
Head Injury
Is this your child's symptom?
- Injuries to the head
- Includes the scalp, skull and brain
Types of Head Injuries
- Scalp Injury. Most head injuries only damage the scalp. Examples are a cut, scrape, bruise or swelling. It is common for children to fall and hit their head while growing up. This is especially common when a child is learning to walk. Big lumps (bruises) can occur with minor injuries. This is because there is a large blood supply to the scalp. For the same reason, small cuts on the head may bleed a lot. Bruises on the forehead sometimes cause black eyes 1 to 3 days later. This is caused by blood spreading downward by gravity.
- Skull Fracture. Only 1% to 2% of children with head injuries will get a skull fracture. Most often, there are no other symptoms except for a headache. The headache occurs at the site where the head was hit. Most skull fractures occur without any injury to the brain. They heal easily.
- Concussion. A head injury that changes how the brain normally works. It is usually caused by a sudden blow or jolt to the head. Most children bump or hit their heads without causing a concussion. The most common signs are a brief period of confusion or memory loss. This happens after the injury. Other signs of a concussion can include a headache or vomiting. Dizziness or acting dazed can also be signs. A person does not need to be knocked out to have had a concussion. Following a concussion, some children have ongoing symptoms. These can include headaches, dizziness or thinking difficulties. School problems or emotional changes can occur. These symptoms can last for several weeks.
- Brain Injuries (Serious) are uncommon. This includes bleeding, bruises or swelling within the brain. They are suspected by the symptoms listed below:
- Hard to wake up or keep awake or
- Acts or talks confused or
- Slurred speech or
- Weakness of arms or legs or
- Walking is not steady.
- These symptoms are an emergency. If they happen, call 911.
Concussion Treatment
- Treating a concussion requires both Physical Rest and Brain Rest.
- Brain rest means a gradual return to full studying and school attendance.
- Physical rest means a gradual return to normal activity, work and gym class.
- If symptoms occur (like a headache), the child needs to return to the previous level of physical and mental activity. In 24 hours, they can try again to take it to the next level.
- Athletes involved in sports need to have a stepwise plan for "return to play." Progressing through stages should be supervised by a doctor or athletic trainer.
Pain Scale
- Mild: your child feels pain and tells you about it. But, the pain does not keep your child from any normal activities. School, play and sleep are not changed.
- Moderate: the pain keeps your child from doing some normal activities. It may wake him or her up from sleep.
- Severe: the pain is very bad. It keeps your child from doing all normal activities.
When to Call for Head Injury
Call 911 Now
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Self Care at Home
|
Call 911 Now
- Seizure occurred
- Knocked out (unconscious) for more than 1 minute
- Not moving neck normally. Caution: protect the neck from any movement.
- Hard to wake up
- Acts or talks confused or slurred speech present now
- Walking not steady or weakness of arms/legs present now
- Major bleeding that can't be stopped
- You think your child has a life-threatening emergency
Call Doctor or Seek Care Now
- Age less than 1 year old
- Knocked out (unconscious) for less than 1 minute
- Skin is split open or gaping and may need stitches
- Bleeding that won't stop after 10 minutes of direct pressure
- Large swelling (larger than 1 inch or 2.5 cm)
- Large dent in skull
- Blow from hard object (such as a golf club)
- Fall from a dangerous height
- You think your child has a serious injury
- You think your child needs to be seen, and the problem is urgent
Call Doctor Within 24 Hours
- Headache lasts more than 24 hours
- You think your child needs to be seen, but the problem is not urgent
Call Doctor During Office Hours
- Dirty cut and no tetanus shot in more than 5 years
- Clean cut and no tetanus shot in more than 10 years
- You have other questions or concerns
Self Care at Home
- Minor head injury
Care Advice for Head Injuries
-
What You Should Know About Mild Head Injuries:
- Most head injuries only cause a swelling or bruise to the scalp.
- The main symptom is pain.
- Swelling of the scalp does not mean there is any swelling of the brain. The scalp and brain are not connected. They are separated by the skull bone.
- The skull bone protects the brain from getting injured.
- Big lumps or bruising can occur with minor injuries to the scalp. This is normal. Reason: the scalp has a large blood supply.
- The mildest brain injury is a concussion. Most of those also turn out fine.
- Here is some care advice that should help.
-
Wound Care:
- If there is a scrape or cut, wash it off with soap and water.
- For any bleeding, put direct pressure on the wound. Use a gauze pad or clean cloth. Press for 10 minutes or until the bleeding has stopped.
-
Cold Pack For Swelling:
- Use a cold pack or ice bag wrapped in a wet cloth. Put it on any swelling. Do this for 20 minutes.
- Reason: Prevent big lumps ("goose eggs"). Also, helps with the pain.
- Repeat in 1 hour, then as needed.
-
Watch Your Child Closely for 2 Hours:
- Watch your child closely during the first 2 hours after the injury.
- Have your child lie down and rest until all symptoms have cleared. Note: mild headache, mild dizziness and nausea are common.
- Allow your child to sleep if he wants to, but keep him nearby.
- Wake him up after 2 hours of sleeping. Check that he is alert and knows who you are. Also, check that he can talk and walk normally.
-
Diet - Start With Clear Fluids:
- Offer only clear fluids to drink, in case he vomits.
- Allow a regular diet after 2 hours.
- Exception: babies can continue breastfeeding or formula.
-
Pain Medicine:
- To help with the pain, give an acetaminophen product (such as Tylenol). Another choice is an ibuprofen product (such as Advil). Use as needed.
- Exception: Do not give until 2 hours have passed from injury without any vomiting.
- Caution: Never give aspirin to children and teens. Reason: Always increases risk of bleeding.
-
Special Precautions For 1 Night:
- Mainly, sleep in same room as your child for the first night.
- Reason: If a problem occurs, you will recognize it if you are close by. Problems include a bad headache, vomiting or confusion. Also, look for any change in your child's normal behavior.
- Option: If you are worried, wake your child once during the night. Check how he walks and talks.
- After 24 hours, return to a normal sleep routine.
-
What to Expect:
- Most head trauma only causes a scalp injury.
- The deep headache usually clears in 24 hours.
- The scalp pain at the site of impact may last 3 days.
- The swelling may take a week to go away.
-
Call Your Doctor If:
- Pain or crying becomes severe
- Vomits 2 or more times
- Your child becomes hard to wake up or confused
- Walking or talking is not normal
- Headache lasts more than 24 hours
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.

This scalp laceration (cut) is gaping open. It will require closure with sutures or medical staples.
First Aid Care Advice:
- Apply direct pressure for 10 minutes to stop any bleeding.
- Wash the cut with soap and water.
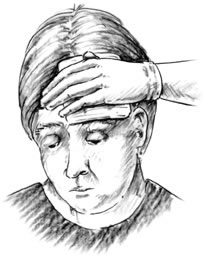
- Apply direct pressure to the entire wound with a sterile gauze dressing or a clean cloth.

This scalp laceration (cut) is gaping open. It will require closure with sutures or medical staples.
First Aid Care Advice:
- Apply direct pressure for 10 minutes to stop any bleeding.
- Wash the cut with soap and water.

This photo shows a scalp laceration after it has been closed with 4 metal medical staples.
Headache
Is this your child's symptom?
- Pain or discomfort of the head
- This includes the forehead to the back of the head
- Not caused by a head injury
If NOT, try one of these:
Causes of Acute Headaches
- Viral Illnesses. Most acute headaches are part of a viral illness. Flu is a common example. These headaches may relate to the level of fever. Most often, they last a few days.
- Hunger Headaches. About 30% of people get a headache when they are hungry. It goes away within 30 minutes of eating something.
- MSG Headache. MSG is a flavor enhancer sometimes added to soups or other foods. In larger amounts, it can cause the sudden onset of a throbbing headache. Flushing of the face also occurs.
- Common Harmless Causes. Hard exercise, bright sunlight, blowing a wind instrument or gum chewing have been reported. So has severe coughing. "Ice cream headaches" are triggered by any icy food or drink. The worse pain is between the eyes (bridge of nose).
- Head Injury. Most just cause a scalp injury. This leads to a painful spot on the scalp for a few days. Severe, deeper or entire-head pain needs to be seen.
- Frontal Sinus Infection. Can cause a headache on the forehead just above the eyebrow. Other symptoms are nasal congestion and postnasal drip. Rare before 10 years old. Reason: the frontal sinus is not yet formed. Other sinus infections cause face pain, not headaches.
- Meningitis (Very Serious). A bacterial infection of the membrane that covers the spinal cord and brain. The main symptoms are a stiff neck, headache, confusion and fever. Younger children are lethargic or so irritable that they can't be consoled. If not treated early, child can suffer brain damage.
Causes of Recurrent Headaches
- Muscle Tension Headaches. Most common type of frequent headaches. Muscle tension headaches give a feeling of tightness around the head. The neck muscles also become sore and tight. Tension headaches can be caused by staying in one position for a long time. This can happen when reading or using a computer. Other children get tension headaches as a reaction to stress or worry. Examples of this are pressure for better grades or family arguments.
- Migraine Headaches. Severe, very painful headaches that keep your child from doing normal activities. They are throbbing and often occur just on one side. Symptoms have a sudden onset and offset. Vomiting or nausea is present in 80%. Lights and sound make them worse. Most children want to lie down in a dark, quiet room. Migraines most often run in the family (genetic).
- School Avoidance. Headaches that mainly occur in the morning on school days. They keep the child from going to school. The headaches are real and due to a low pain threshold.
- Rebound Headaches. Caused by overuse of pain medicines in high doses. Most often happens with OTC meds. Caffeine is present in some pain meds and may play a role. Treatment is taking pain meds at the correct dosage.
- Not Due to Needing Glasses (Vision Headaches). Poor vision and straining to see the blackboard causes eye pain. Sometimes, it also causes a muscle tension headache. But, getting glasses rarely solves a headache problem that doesn't also have eye pain.
Pain Scale
- Mild: your child feels pain and tells you about it. But, the pain does not keep your child from any normal activities. School, play and sleep are not changed.
- Moderate: the pain keeps your child from doing some normal activities. It may wake him or her up from sleep.
- Severe: the pain is very bad. It keeps your child from doing all normal activities.
When to Call for Headache
Call 911 Now
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Self Care at Home
|
Call 911 Now
- Hard to wake up or passed out
- Acts or talks confused
- Weakness of arm or leg on one side of the body
- You think your child has a life-threatening emergency
Call Doctor or Seek Care Now
- Vomiting
- Blurred vision or seeing double
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Call Doctor Within 24 Hours
- Fever
- Sinus pain (not just congestion) of forehead
- Swelling around the eye with pain
- You think your child needs to be seen, but the problem is not urgent
Call Doctor During Office Hours
- Headache without other symptoms lasts more than 24 hours
- Migraine headache suspected, but never diagnosed
- Sore throat lasts more than 48 hours
- Any headache lasts more than 3 days
- Headaches are a frequent problem
- You have other questions or concerns
Self Care at Home
- Mild headache
- Migraine headache, just like past ones
Care Advice
Treatment for Mild Headache
-
What You Should Know About Mild Headaches:
- Headaches are very common with some viral illnesses. Most often, these will go away in 2 or 3 days.
- Unexplained headaches can occur in children, just as they do in adults. They usually pass in a few hours or last up to a day.
- Most recurrent headaches that can occur in anyone are muscle tension headaches.
- Most headaches (including muscle tension headaches) are helped by the following measures.
-
Pain Medicine:
- To help with the pain, give an acetaminophen product (such as Tylenol).
- Another choice is an ibuprofen product (such as Advil).
- Use as needed.
- Headaches due to fever are also helped by bringing the fever down.
-
Food May Help:
- Give fruit juice or food if your child is hungry.
- If your child hasn't eaten in more than 4 hours, offer some food.
- Reason: Skipping a meal can cause a headache in many children.
-
Rest - Lie Down:
- Lie down in a quiet place and relax until feeling better.
-
Cold Pack for Pain:
- Put a cold pack or a cold wet washcloth on the forehead.
- Do this for 20 minutes. Repeat as needed.
-
Stretch Neck Muscles:
- Stretch and rub any tight neck muscles.
-
Muscle Tension Headache Prevention:
- If something bothers your child, help him talk about it. Help him get it off his mind.
- Teach your child to take breaks when he is doing school work. Help your child to relax during these breaks.
- Teach your child the importance of getting enough sleep.
- Some children may feel pressure to achieve more. This may cause headaches. If this is the case with your child, help him find a better balance.
- Caution: Frequent headaches are often caused by too much stress or worry. To be sure, get your child a medical checkup first.
-
Call Your Doctor If:
- Headache becomes severe
- Vomiting occurs
- Headache without other symptoms lasts more than 24 hours
- Headache lasts more than 3 days
- You think your child needs to be seen
- Your child becomes worse
Treatment for Migraine Headache
-
What You Should Know About Migraine Headaches:
- This headache is like the migraine headaches that your child has had before.
- The sooner a migraine headache is treated, the more likely the treatment will work.
- Often the most helpful treatment is going to sleep.
- Here is some care advice that should help.
-
Migraine Medicine:
- If your child's doctor has prescribed a medicine for migraines, use it as directed. Give it as soon as the migraine starts.
- If not, you can use ibuprofen (such as Advil). It is the best over-the-counter drug for migraines. Give it now. Repeat in 6 hours if needed.
-
Try to Sleep:
- Have your child lie down in a dark, quiet place.
- Try to fall asleep.
- People with a migraine often wake up from sleep with their migraine gone.
-
Prevention of Migraine Attacks:
- Drink lots of fluids.
- Don't skip meals.
- Get enough sleep each night.
-
What to Expect:
- With treatment, migraine headaches usually go away in 2 to 6 hours.
- Most people with migraines get 3 or 4 attacks per year.
-
Return to School:
- Children with a true migraine headache are not able to stay in school.
- Children with migraine headaches also commonly get muscle tension headaches. For those, they should take a pain medicine and go to school.
-
Call Your Doctor If:
- Headache becomes much worse than past migraines
- Headache lasts longer than past migraines
- You think your child needs to be seen
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.
Heat Exposure and Reactions
Is this your child's symptom?
- Symptoms after being in high temperatures (such as heat waves)
- Symptoms after hard work or sports during hot weather
- Heat cramps, heat exhaustion and heatstroke are covered
- Prevention of heat exposure symptoms also covered
If NOT, try one of these:
Types of Heat Reactions
- There are 3 main reactions to hot temperatures and heat waves.
- Heatstroke or Sunstroke (Serious). Symptoms include hot, flushed skin with high fever over 105° F (40.5° C). A rectal temperature is more accurate than an oral temperature in these cases. 50% of children with heatstroke do not sweat. Heatstroke can cause confusion, coma or shock. Heatstroke is a life-threatening emergency. It has a high death rate if not treated promptly.
- Heat Exhaustion. Symptoms include pale skin, profuse sweating and nausea. Dizziness, fainting, or weakness can also be signs. Can have a mild fever 100 - 102° F (37.8 - 39° C) for a short time. Most of the time, there is no fever. Most of these symptoms are caused by dehydration from sweating. A person can progress from heat exhaustion to heatstroke. So, all patients with severe symptoms (such as fainting) need to be seen now. Mild symptoms (such as dizziness) can be treated at home with fluids and rest. But, if these don't resolve with treatment, these children also need to be seen.
- Heat Cramps. Severe muscle cramps in the legs (calf or thigh muscles) and stomach are present. No fever. Tightness or spasms of the hands may occur. After your child drinks fluids and cools down, he or she will feel better. All symptoms should go away in a few hours.
Causes of Heat Reactions
- All 3 reactions are caused by exposure to high temperatures often with high humidity.
- During hot weather, hard work or sports can cause heat production to exceed heat loss.
- Poor hydration interferes with sweating and increases the risk of heat reactions.
- Babies are at more risk because they are less able to sweat when hot.
- A hot humid climate can also add risk if you aren't used to it. This happens on vacations. The first heat wave of the summer can cause similar problems. It takes 8 to 10 days for you to become used to high summer temperatures.
- Heatstroke is a breakdown in how the body regulates temperature. It usually follows exposure to a very high temperature. Examples are being inside a hot car or in a steam tent. Being indoors without air-conditioning during heat waves is also a risk factor.
When to Call for Heat Exposure and Reactions
Call 911 Now
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
|
Self Care at Home
|
Call 911 Now
- Hard to wake up or can't wake up
- Acts or talks confused
- Seizure occurred
- Signs of shock (very weak or gray, cool skin)
- Fever over 105° F (40.5° C)
- You think your child has a life-threatening emergency
Call Doctor or Seek Care Now
- Age less than 12 weeks old and not acting normal after heat exposure
- Age less than 12 weeks old with fever. Caution: do NOT give your baby any fever medicine before being seen.
- Vomiting keeps from drinking fluids
- Dehydration suspected. No urine in more than 8 hours, dark urine, very dry mouth and no tears.
- Fever or dizziness still there after drinking fluids for more than 2 hours
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Call Doctor Within 24 Hours
- You think your child needs to be seen, but the problem is not urgent
Self Care at Home
- Normal muscle cramps or sore muscles from heat exposure
- Normal dizziness from heat exposure
- Normal fever (under 104° F or 40.0° C) from heat exposure
- Prevention of heat reactions
Care Advice for Heat Exposure
-
Drink Lots of Fluids:
- All the symptoms of heat reactions respond to fluid replacement.
- Type of Fluid. Give your child as much cold water as he will drink. Do this until he feels better.
- If you have a sports drink (such as Gatorade), give it instead. Sports drinks contain water, salt and sugar.
- How Much (Teens). Start with 3 cups (24 ounces or 720 mL). Then give 1 cup (240 mL) every 15 minutes for the next 1-2 hours.
- Preteens (6-12). Start with 2 cups (16 ounces or 480 mL). Then give 6 ounces (180 mL) every 15 minutes for the next 1-2 hours.
- Urine Color. The urine color can tell you if drinking enough fluids. Dark yellow urine means mild dehydration. Clear or light yellow urine means your child is drinking enough fluids.
-
Heat Cramps - What You Should Know:
- Heat cramps are the most common reaction to heat exposure. They are never serious. Sometimes, they can be an early warning sign of heat exhaustion.
- The cramps occur in the muscles that were working the hardest.
- Heat cramps can be quite painful.
- Heat cramps mean that the body needs rest and more liquids and salt.
- Heat cramps should clear in 1 to 2 hours after lost fluids are replaced.
-
Heat Exhaustion:
- Put the child in a cool place. Have him lie down with the feet elevated.
- Undress him (except for underwear) so the body surface can give off heat.
- Sponge the entire body surface constantly with cool water. Make the water as cold as tolerated without causing shivering.
- Weakness should clear in 2 to 3 hours after lost fluids are replaced.
-
Dizziness - What You Should Know:
- Dizziness and weakness can be caused by mild dehydration. This occurs from all the sweating that happens when hot.
- Dizziness should clear in 1 to 2 hours after the lost fluids are replaced.
- Mild dehydration can also cause nausea. It should pass after drinking enough fluids.
-
Fever - What You Should Know:
- The body can become overheated from activity when it's hot outdoors. The temperature should come down to normal after drinking fluids and resting. This may take 1 or 2 hours.
- Fluids: First, have your child drink some liquids.
- Cool Bath: Second, take a cool bath or shower for 5 minutes. Reason: Brings down the temperature faster.
- No Meds: Fever medicines are of no value for this type of fever.
-
Salty Food:
- After your child has taken 2 or 3 glasses of water, offer some salty foods. Potato chips or pretzels are helpful.
- Don't give salt tablets. Reason: They slow down the absorption of water and may cause vomiting.
-
Rest - Lie Down:
- Rest in a cool place with a fan until feeling better.
-
Prevention Of Heat Reactions:
- When working outside, have your child drink large amounts of cool water. This helps to prevent dehydration. For teens, this means at least 8 ounces (240 mL) every 15 to 30 minutes. Water is the ideal solution for replacing lost sweat. Very little salt is lost.
- Most often, special sports drinks offer no advantage over water. But, they are helpful if working out for longer than an hour. If that is the case, replace 1 water drink per hour with a sports drink.
- Have your child take water breaks every 15 minutes in the shade. Have him drink some water even if he's not thirsty. Thirst can be delayed until a person is almost dehydrated.
- Do not use salt tablets. They slow down stomach emptying and delay the absorption of fluids.
- Have your child wear a single layer of lightweight clothing. Change it if it becomes wet with sweat.
- Physical activity in hot weather should be increased slowly.
- Sports coaches suggest that exercise sessions be shortened and made easier when it's hot. This is usually when the temperature is over 82°F (28°C). Also, this is very important if the humidity is high.
- Protect babies with fevers from heatstroke by not bundling them in blankets. Also, do not dress them in too many clothes. Children usually need the same number of clothing layers as adults.
- During heat waves, spend as much time as possible inside with air-conditioning. Electric fans also help. Slow down. It takes at least a week to get used to hot summer temperatures.
-
Prevention - Hot Tubs:
- Age limit: Do not use hot tubs in children less than 3 years old.
- Reason: Poor heat tolerance and increased risk for rapid onset of high body temperature.
- When using a hot tub, limit use to 15 minutes. Use a "buddy" system in case a heat reaction suddenly occurs.
- Do not use a hot tub if your child has a fever. Also, do not use them right after hard work or sports. The body needs to get rid of heat.
-
Call Your Doctor If:
- Vomiting keeps from drinking
- Signs of dehydration occur
- Muscle cramps last more than 4 hours
- Fever goes above 104°F (40.0°C)
- Fever lasts more than 2 hours
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.
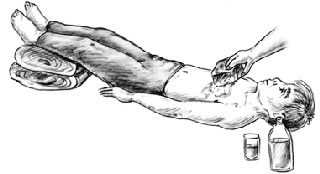
- Move the victim to a cool shady area. If possible, move into an air-conditioned place.
- The victim should lie down. Elevate the feet.
- Undress victim (except for underwear) so the body surface can give off heat.
- Sponge the entire body surface continuously with cool water. Fan the victim to increase evaporation.
- Give as much cold water or sports drink (e.g., Gatorade, Powerade) as the victim can tolerate. An adult or teen with heat exhaustion should drink 2-3 cups (480-720 ml) of liquids right away to replace what was lost. Then the adult or teen should drink approximately 1 cup (240 ml) every 15 minutes for the next 1-2 hours.
Heat Rash
Is this your child's symptom?
- A fine pink rash caused by overheating
- Mainly on the neck, chest, and upper back
If NOT, try one of these:
Symptoms of Heat Rash
- Tiny, pink bumps
- Mainly on the neck, chest and upper back
- Occurs during hot, humid weather or after lots of sun
- Heat rash can be itchy
- Older children may have a "prickly" pins and needles feeling
- In babies, the rash can have some tiny water blisters
- No fever or illness
- Also called "prickly heat"
Causes of Heat Rash
- Heat rash is caused by blocked-off sweat glands.
- Hot Weather. Hot, humid weather can cause the sweat glands to be overworked.
- Ointment. Babies can also get it in the wintertime from ointments put on the skin. Reason: Ointments can block off sweat glands.
- Location. Heat rash of the forehead can be caused by oil or ointment on the hair. Heat rash of the face of a breastfed baby can be caused by lanolin put on the nipples. Heat rash of the chest can be caused by menthol ointments put on for coughs.
- Exercise. Older children can get heat rash with hard exercise.
When to Call for Heat Rash
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Self Care at Home
|
Call Doctor or Seek Care Now
- Fever and looks infected (spreading redness or pus)
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Call Doctor Within 24 Hours
- Looks infected (spreading redness, pus), but no fever
- You think your child needs to be seen, but the problem is not urgent
Call Doctor During Office Hours
- Rash is not gone after 3 days of treatment
- You have other questions or concerns
Self Care at Home
- Heat rash
Care Advice for Heat Rash
-
What You Should Know About Heat Rash:
- Heat rash is caused by blocked-off sweat glands.
- It's common in hot, humid weather.
- Here is some care advice that should help.
-
Cooling the Skin:
- Cool off the skin to treat and prevent heat rash.
- For large rashes, give your child a cool bath without soap. Do this for 10 minutes. (Caution: Avoid any chill.) Let the skin air-dry. Do this 3 or more times a day.
- For small rashes, put a cool, wet washcloth on the area. Do this for 5 to 10 minutes. Then let the skin air-dry.
- Dress in as few layers of clothing as you can.
- Lower the temperature in your home if you can.
-
Sleeping Cooler:
- When your child is asleep, run a fan in the bedroom.
- During sleep, have your child lie on a cotton towel to absorb sweat. (Note: Only for older children age over 1 year.)
-
Steroid Cream for Itching:
- Use 1% hydrocortisone cream (such as Cortaid). No prescription is needed.
- Put it on itchy spots 3 times per day.
- Avoid hydrocortisone ointment.
- Calamine lotion can also work.
-
Do Not Use Ointments:
- Avoid all ointments or oils on the skin. Reason: They can block off sweat glands.
- Be sure the rash isn't caused by a menthol ointment being used for a cough.
-
What to Expect:
- With treatment, heat rash will clear up in 2 to 3 days.
-
Call Your Doctor If:
- Rash lasts more than 3 days on this treatment
- Rash starts to look infected
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.
Hives
Is this your child's symptom?
- An itchy rash made up of raised pink bumps
- Most often, rash is very itchy
Mosquito bites suspected, see
Symptoms of Hives
- Raised pink bumps with pale centers (welts)
- Hives look like mosquito bites
- Sizes of hives vary from ½ inch (12 mm) to several inches (cm) across
- Shapes and location of hives can be different. They can also change often.
- Itchy rash
Causes of Widespread Hives
- Viral Infection. The most common cause of hives all over the body is viral infections. Research has confirmed this. Other symptoms such as a fever, cough or diarrhea are also present. The hives may last 3 days. This is not an allergy.
- Bacterial Infection. Some bacterial infections can also cause hives. A common example is Strep. Hives are also seen with bladder infections. (UTIs)
- Drug Reaction. An example is a penicillin rash. Most rashes that start while taking an antibiotic are viral rashes. Allergy tests are normal 90% of the time. Only 10% turn out to be a drug allergy.
- Food Reaction. May be an allergy or a coincidence. If the food is a high risk one (such as peanuts), consult an allergist. Hives from foods usually resolve in 6 hours. Hives from infections last for days. Only 3% of hives are due to a food.
- Bee Sting. Widespread hives after a sting may be part of a serious allergic reaction. Need to consult an allergist.
- Anaphylactic Reaction (Very Serious). The sudden onset of hives with trouble breathing or swallowing. This is a severe allergic reaction to an allergic food or drug. Most often begins within 30 minutes of swallowing the substance. Always within 2 hours of exposure.
- Unknown. Over 30% of the time, the cause of hives is not found.
Causes of Localized Hives
- Irritants. Hives just in one spot are usually due to skin contact with an irritant. They are not an allergy.
- Plants. Many plants cause skin reactions. Sap from evergreens can cause local hives.
- Pollen. Playing in the grass can cause hives on exposed skin.
- Pet Saliva. Some people get hives where a dog or cat has licked them.
- Food. Some children get hives if a food is rubbed on the skin. An example could be a fresh fruit. Some babies get hives around their mouth from drooling a new food.
- Insect Bite. Local hives are a reaction to the insect's saliva. Can be very large without being an allergy.
- Bee Sting. This is a reaction to the bee's venom. Can be very large without being an allergy.
- Localized hives are not caused by drugs, infections or swallowed foods. These get into the bloodstream and cause widespread hives.
When to Call for Hives
Call 911 Now
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Self Care at Home
|
Call 911 Now
- Hives and life-threatening allergic reaction to similar substance in the past and exposure less than 2 hours ago
- Trouble breathing or wheezing
- Hoarse voice or cough start all of a sudden
- Trouble swallowing, drooling or slurred speech start all of a sudden
- You think your child has a life-threatening emergency
Call Doctor or Seek Care Now
- Hives start after eating a high-risk food. High-risk foods include nuts, fish, shellfish, or eggs.
- Hives started after taking a prescription medicine
- Age less than 1 year with hives all over
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Call Doctor Within 24 Hours
- Hives started after taking an over-the-counter medicine
- Severe hives (such as eyes swollen shut or very itchy)
- Fever or joint swelling is present
- Stomach pain or vomiting
- You think your child needs to be seen, but the problem is not urgent
Call Doctor During Office Hours
- Hives make it hard to go to school or do other normal activities. Note: taking Benadryl for 24 hours has not helped.
- Food could be the cause
- Had hives 3 or more times in past year with no known cause
- Hives last more than 1 week
- You have other questions or concerns
Self Care at Home
- Hives with no other problems
Care Advice for Hives
-
Hives Only on One Part of the Body - What You Should Know:
- Most are caused by skin contact with an irritant. Examples are plants, pollen, food or pet
saliva. - Localized hives are not caused by drugs, infections or swallowed foods. They are also not an allergy.
- Wash the allergic substance off the skin with soap and water.
- If itchy, use a cold pack for 20 minutes. You can also rub the hives with an ice cube for 10 minutes.
- Hives just on one part of the body should go away on their own. They don't need Benadryl.
- They should go away in a few hours.
- Most are caused by skin contact with an irritant. Examples are plants, pollen, food or pet
-
Hives All Over the Body - What You Should Know:
- Over 10% of children get hives 1 or more times.
- Most widespread hives are caused by a viral infection. This is not due to an allergy. Less than 10% are an allergic reaction to a food, drug, or insect bite. Often, the cause is not found.
- Here is some care advice that should help.
-
Benadryl for Hives All Over the Body:
- Give Benadryl 4 times per day for hives all over that itch. No prescription is needed.
- If you only have another allergy medicine at home (but not Benadryl), use that.
- Continue the Benadryl 4 times per day until the hives are gone for 12 hours.
- Caution: Do not use if age is under 1 year. Reason: Benadryl is a sedative. Give your doctor a call for advice.
-
Hives Caused by Foods:
- Foods can cause widespread hives.
- Sometimes, the hives are just around the mouth.
- Hives from foods usually last just a short time. They often are gone in less than 6 hours.
-
Cool Bath for Itching:
- To help with the itching, give a cool bath. Do this for 10 minutes. Caution: Avoid causing a chill.
- Can also rub very itchy spots with an ice cube for 10 minutes.
-
Wash Allergens Off Body:
- Give a bath or shower if caused by pollens or animal contact.
- Change clothes.
-
Stay Away from Allergens:
- If you know what is causing the hives, avoid this substance. An example is certain foods.
- Help your child stay away from this allergen in the future.
-
Return to School:
- Hives cannot be spread to others.
- Your child can go back to school once feeling better. The hives shouldn't keep him from normal activities.
- For hives from an infection, can go back after the fever is gone. Your child should feel well enough to join in normal activities.
-
What to Expect:
- Hives all over from a viral illness normally come and go.
- They may last for 3 or 4 days. Then, they go away.
- Most children get hives once.
-
Call Your Doctor If:
- Severe hives not better after 2 doses of Benadryl
- Itch not better after 24 hours on Benadryl
- Hives last more than 1 week
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.

- Hives is an itchy rash.
- The shapes of hives are variable. Sizes of hives vary from ½ inch to several inches across.
- Hives may disappear in one area and then reappear somewhere else, over the course of several hours.

- Hives is an itchy rash.
- The shapes of hives are variable. Sizes of hives vary from ½ inch to several inches across.
- Hives may disappear in one area and then reappear somewhere else, over the course of several hours.
Human or Animal Bite
Is this your child's symptom?
- Bite from a pet, wild animal or human
Types of Wounds
- Bruise. There is no break in the skin. No risk of infection.
- Scrape (Abrasion) or Scratch. A wound that doesn't go all the way through the skin. Low chance of infection. Antibiotic drugs are not needed.
- Cut (Laceration). A wound that goes through the skin to the fat or muscle tissue. Some chance of infection. Most need to be seen. Cleaning the wound can help prevent this. Antibiotic drugs may be needed.
- Puncture Wound. These wounds break through the skin. Greater risk of infection. Puncture wounds from cat bites are more likely to get infected. Antibiotic drugs may be needed.
- Wound Infection. This is the main risk of an animal bite. The main finding is redness around the bite and pain. It starts 8 hours to 3 days after the bite. It can often be prevented by early, careful cleaning of the bite. This is why most animal bites need to be seen.
Types of Animal Bites
- Large Wild Animal Bites. Rabies is a disease that can kill people. Bites or scratches from any large wild animal can pass on rabies. Animals at highest risk are bats, skunks, raccoons, foxes, or coyotes. These animals may spread rabies even if they have no symptoms.
- Small Wild Animal Bites. Small animals such as mice, rats, moles, or gophers do not carry rabies. Chipmunks, prairie dogs, squirrels and rabbits also do not carry rabies. Exception: one of these small animals actually attacks a human (an unprovoked bite). Sometimes, their bites can get infected.
- Large Pet Animal Bites. Most bites from pets are from dogs or cats. Bites from other pets such as horses can be handled using this guide. Dogs and cats are free of rabies in most U.S. and Canadian cities. Stray animals are always at risk for rabies until proven otherwise. Cats and dogs that always stay indoors should be safe. The main risk in pet bites is wound infection, not rabies. Cat bites become infected more often than dog bites. Cat scratches can get infected just like a bite because cats lick their claws.
- Small Indoor Pet Animal Bites. Small indoor pets are not at risk for rabies. Examples of these pets are gerbils, hamsters, guinea pigs, or mice. Tiny puncture wounds from these small animals also don't need to be seen. They carry a small risk for wound infections.
- Human Bites. Most human bites occur during fights, especially in teenagers. Sometimes a fist is cut when it strikes a tooth. Human bites are more likely to become infected than animal bites. Bites on the hands are at higher risk. Many toddler bites are safe because they don't break the skin.
- Bat Bites and Rabies. In the U.S., 90% of cases of rabies in humans are caused by bats. Bats have spread rabies without a visible bite mark.
Animals at Risk for Rabies
- Bat, skunk, raccoon, fox, or coyote
- Other large wild animals
- Pets that have never had rabies shots and spend time outdoors
- In the U.S., rabies occurs 4 times more in cats than in dogs.
- Outdoor animals who are sick or stray
- Dogs or cats in countries that do not require rabies shots
- In the U.S. and Canada, bites from city dogs and cats are safe.
- In the U.S., there are 2 - 3 deaths from rabies per year in humans.
When to Call for Human or Animal Bite
Call 911 Now
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Self Care at Home
|
Call 911 Now
- Major bleeding that can't be stopped
- Not moving or too weak to stand
- You think your child has a life-threatening emergency
Call Doctor or Seek Care Now
- Wild animal bite that breaks the skin
- Pet animal (such as dog or cat) bite that breaks the skin. Exception: minor scratches that don't go through the skin.
- Puncture wound (holes through skin) from a Cat's teeth or claws
- Puncture wound (holes through skin) of hand or face
- Human bite that breaks the skin
- Bite looks infected (redness or red streaks) or has a fever
- Bat contact or exposure, even without a bite mark
- Contact with a rabies-prone animal, even without a bite mark
- Minor cut or scrape and no past tetanus shots
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Call Doctor Within 24 Hours
- Last tetanus shot more than 5 years ago
- You think your child needs to be seen, but the problem is not urgent
Call Doctor During Office Hours
- You have other questions or concerns
Self Care at Home
- Bite did not break the skin or is only a bruise
- Minor scratches that don't go through the skin from a pet
- Tiny puncture wound from small pet, such as a hamster or puppy. Exception: cat puncture wound.
Care Advice for Animal or Human Bite
-
What You Should Know About Bites:
- Bites that don't break the skin can't become infected.
- Cuts and punctures always are at risk for infection.
- Here is some care advice that should help.
-
Clean the Bite:
- Wash all wounds right now with soap and water for 5 minutes.
- Also, flush well under running water for a few minutes. Reason: Can prevent many wound infections.
-
Bleeding - How to Stop:
- For any bleeding, put pressure on the wound.
- Use a gauze pad or clean cloth.
- Press for 10 minutes or until the bleeding has stopped.
-
Antibiotic Ointment:
- For small cuts, use an antibiotic ointment (such as Polysporin). No prescription is needed.
- Put it on the cut 3 times a day.
- Do this for 3 days.
-
Pain Medicine:
- To help with the pain, give an acetaminophen product (such as Tylenol).
- Another choice is an ibuprofen product (such as Advil).
- Use as needed.
-
Cold Pack for Pain:
- For pain or bruising, use a cold pack. You can also use ice wrapped in a wet cloth. Apply it to the bruise once for 20 minutes. Reason: Helps with bleeding, pain and swelling.
-
What to Expect:
- Most scratches, scrapes and other minor bites heal up fine in 5 to 7 days.
-
Call Your Doctor If:
- Bite starts to look infected (pus, redness, red streaks)
- Fever occurs
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.
Immunization Reactions
Is this your child's symptom?
- Reactions to a recent immunization (vaccine)
- Most are reactions at the shot site (such as pain, swelling, redness)
- General reactions (such as a fever or being fussy) may also occur
Reactions to These Vaccines are Covered:
- Chickenpox (varicella) virus
- DTaP (Diphtheria, Tetanus, Pertussis)
- Hemophilus influenzae type b
- Hepatitis A virus
- Hepatitis B virus
- Human Papilloma virus
- Influenza virus
- MMR (Measles, Mumps, Rubella)
- Meningococcal
- Polio virus
- Pneumococcal
- Rotavirus
- Tuberculosis (BCG vaccine)
Symptoms of Vaccine Reactions
- Local Reactions. Shot sites can have swelling, redness and pain. Most often, these symptoms start within 24 hours of the shot. They most often last 3 to 5 days. With the DTaP vaccine, they can last up to 7 days.
- Fever. Fever with most vaccines begins within 24 hours and lasts 1 to 2 days.
- Delayed Reactions. With the MMR and chickenpox shots, fever and rash can occur. These symptoms start later. They usually begin between 1 and 4 weeks.
- Anaphylaxis. Severe allergic reactions are very rare, but can occur with any vaccine. They start within 2 hours.
Vaccine Free App
- Vaccines on the Go app from Children's Hospital of Philadelphia
- This free app can answer any vaccine questions you may have
- It is fact-based and up-to-date
When to Call for Immunization Reactions
Call 911 Now
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Self Care at Home
|
Call 911 Now
- Trouble breathing or swallowing
- Not moving or very weak
- Can't wake up
- You think your child has a life-threatening emergency
Call Doctor or Seek Care Now
- Age less than 12 weeks old with fever. Caution: do NOT give your baby any fever medicine before being seen.
- Fever over 104° F (40° C)
- High-pitched crying lasts more than 1 hour
- Crying nonstop lasts more than 3 hours
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Call Doctor Within 24 Hours
- Redness or red streak starts more than 48 hours (2 days) after the shot
- Redness around the shot becomes larger than 3 inches (7.5 cm)
- Fever lasts more than 3 days
- Fever returns after being gone more than 24 hours
- Measles vaccine rash (starts day 6 to 12 after shot) lasts more than 4 days
- You think your child needs to be seen, but the problem is not urgent
Call Doctor During Office Hours
- Redness or red streak around shot is larger than 1 inch (2.5 cm)
- Redness, swelling or pain is getting worse after 3 days
- Fussiness from vaccine lasts more than 3 days
- You have other questions or concerns
Self Care at Home
- Normal immunization reaction
Care Advice for Immunization Reactions
Treatment for Common Immunization Reactions
-
What You Should Know About Common Shot Reactions:
- Immunizations (vaccines) protect your child against serious diseases.
- Pain, redness and swelling are normal where the shot was given. Most symptoms start within the first 12 hours after the shot was given. Redness and fever starting on day 1 of the shot is always normal.
- All of these reactions mean the vaccine is working.
- Your child's body is making new antibodies to protect against the real disease.
- Most of these symptoms will only last 2 or 3 days.
- There is no need to see your doctor for normal reactions, such as redness or fever.
- Medicine is only needed if your child has pain. Also, use a fever medicine for fever over 102° F (39 ° C).
- Here is some care advice that should help.
-
Reaction at Shot Site:
- Cold Pack: For pain at the shot site, use a cold pack. You can also use put ice in a wet washcloth on the sore shot site. Use for 20 minutes as needed.
- Pain Medicine: To help with the pain, give an acetaminophen product (such as Tylenol). Another choice is an ibuprofen product (such as Advil). Use as needed.
- Hives at the Shot Site: If itchy, can put on 1% hydrocortisone cream (such as Cortaid). No prescription is needed. Use twice daily as needed.
-
Fever Medicine:
- Fever with most vaccines begins within 12 hours and lasts 2 to 3 days. This is normal, harmless and possibly helpful.
- For fevers above 102° F (39° C), give an acetaminophen product (such as Tylenol).
- If over 6 months old, can give an ibuprofen product (such as Advil).
- For all fevers: Give extra fluids. Do not use too many clothes or blankets on your child.
-
General Symptoms From Vaccines:
- All vaccines can cause mild fussiness, crying and restless sleep. This is usually due to a sore shot site.
- Some children sleep more than usual. A decreased appetite and activity level are also common.
- These symptoms are normal. They do not need any treatment.
- They will usually go away in 24-48 hours.
-
Call Your Doctor If:
- Redness starts after 2 days (48 hours)
- Redness becomes larger than 2 inches (5 cm)
- Pain or redness gets worse after 3 days (or lasts more than 7 days)
- Fever starts after 2 days (or lasts more than 3 days)
- You think your child needs to be seen
- Your child becomes worse
Specific Immunization Reactions
-
Chickenpox Vaccine:
- Pain or swelling at the shot site for 1 to 2 days. (20% of children)
- Mild fever lasting 1 to 3 days begins 14 to 28 days after the shot (10%). Give acetaminophen or ibuprofen for fever over 102° F (39°C).
- Never give aspirin for fever, pain or within 6 weeks of getting the shot. Reason: Risk of Reye syndrome, a rare but serious brain disease.
- Chickenpox-like rash (usually 2 red bumps) at the shot site (3%)
- Chickenpox-like rash (usually 5 red bumps) scattered over the body (4%)
- This mild rash begins 5 to 26 days after the shot. Most often, it lasts a few days.
- Children with these rashes can go to child care or school. Reason: For practical purposes, vaccine rashes are not spread to others.
- Exception: Do not go to school if red bumps drain fluid and are widespread. Reason: can be actual chickenpox.
- Caution: If vaccine rash contains fluid, cover it with clothing. You can also use a bandage (such as Band-Aid).
-
Diphtheria, Tetanus, Pertussis (DTaP) Vaccine:
- The following harmless reactions to DTaP can occur:
- Pain, tenderness, swelling and redness at the shot site are the main side effects. This happens in 25% of children. It usually starts within the first 12 hours. Redness and fever starting on day 1 of the shot is always normal. It lasts for 3 to 7 days.
- Fever (in 25% of children) and lasts for 24 to 48 hours
- Mild drowsiness (30%), fretfulness (30%) or poor appetite (10%) and lasts for 24 to 48 hours.
- Large swelling over 4 inches (10 cm) can follow the later doses of DTaP. The area of redness is smaller. This usually occurs with the 4th or 5th dose. It occurs in 5% of children. Most children can still move the leg or arm normally.
- The large thigh or upper arm swelling goes away without treatment by day 3 (60%) to day 7 (90%).
- This is not an allergy. Future DTaP vaccines are safe to give.
-
Hemophilus Influenza Type B Vaccine (Hib):
- No serious reactions reported.
- Sore injection site or mild fever only occurs in 2% of children.
-
Hepatitis A Vaccine:
- No serious reactions reported.
- Sore injection occurs in 20% of children.
- Loss of appetite occurs in 10% of children.
- Headache occurs in 5% of children.
- Most often, no fever is present.
- If these symptoms occur, they most often last 1-2 days.
-
Hepatitis B Virus Vaccine (HBV):
- No serious reactions reported.
- Sore shot site occurs in 30% of children and mild fever in 3% of children.
- Fever from the vaccine is rare. Any baby under 2 months with a fever after this shot should be examined.
-
Influenza Virus Vaccine:
- Pain, tenderness or swelling at the injection site occurs within 6 to 8 hours. This happens in 10% of children.
- Mild fever under 103° F (39.5° C) occurs in 20% of children. Fevers mainly occur in young children.
- Nasal Influenza Vaccine: Congested or runny nose, mild fever.
-
Measles Vaccine (part of MMR):
- The measles shot can cause a fever (10% of children) and rash (5% of children). This occurs about 6 to 12 days after the shot.
- Mild fever under 103° F (39.5°C) in 10% and lasts 2 or 3 days.
- The mild pink rash is mainly on the trunk and lasts 2 or 3 days.
- No treatment is needed. The rash cannot be spread to others. Your child can go to child care or to school with the rash.
-
Call Your Doctor If:
- Rash changes to blood-colored spots
- Rash lasts more than 3 days
-
Meningococcal Vaccine:
- No serious reactions.
- Sore shot site for 1 to 2 days occurs in 50%. Limited use of the arm occurs in 15% of children.
- Mild fever occurs in 5%, headache in 40% and joint pain in 20%
- The vaccine never causes meningitis.
-
Mumps or Rubella Vaccine (part of MMR):
- There are no serious reactions.
- Sometimes, a sore shot site can occur.
-
Papillomavirus Vaccine:
- No serious reactions.
- Sore injection site for few days in 90%.
- Mild redness and swelling at the shot site (in 50%).
- Fever over 100.4° F (38.0° C) in 10% and fever over 102° F (39° C) in 2%.
- Headache in 30%.
-
Pneumococcal Vaccine:
- No serious reactions.
- Pain, tenderness, swelling or redness at the injection site in 20%.
- Mild fever under 102° F (39° C) in 15% for 1-2 days.
-
Polio Vaccine:
- Polio vaccine given by shot sometimes causes some muscle soreness.
- Polio vaccine given by mouth is no longer used in the U.S.
-
Rotavirus Vaccine:
- No serious reactions to this vaccine given by mouth.
- Mild diarrhea or vomiting for 1 to 2 days in 3%.
- No fever.
-
BCG Vaccine for Tuberculosis (TB):
- Vaccine used to prevent TB in high-risk groups or countries. It is not used in the US or most of Canada. Note: This is different than the skin test placed on the forearm to detect TB.
- BCG vaccine is given into the skin of the right shoulder area.
- Timing: Mainly given to infants and young children.
- Normal reaction: After 6 to 8 weeks, a blister forms. It gradually enlarges and eventually drains a whitish yellow liquid. The blister then heals over leaving a scar. The raised scar is proof of BCG protection against TB.
- Abnormal reaction: Abscess (infected lump) occurs in the shoulder or under the arm. Occurs in 1% of patients.
-
Call Your Doctor If:
- Blister turns into a large red lump
- Lymph node in the armpit becomes large
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.
Impetigo - Infected Sores
Is this your child's symptom?
- Coin-shaped sores on the skin covered by scabs
- The infected crusts are the color of honey
- Skin infection caused by a bacteria
If NOT, try one of these:
Symptoms of Impetigo
- Sores smaller than 1 inch (2.5 cm)
- Often covered by a soft, yellow-brown scab or crust
- Scabs may drain pus or yellow fluid off and on
- Starts as small red bumps. These change quickly to cloudy blisters or pimples. Then, they become open sores which drain fluid or pus.
- Sores increase in size
- Any sore or wound that grows and doesn't heal is usually impetigo.
Cause of Impetigo
- A skin infection caused by a bacteria. It starts in a small break in the skin. Examples are a scratch or insect bite.
- The most common bacteria are Staph and Strep. If the child has a sore throat, they may also have Strep throat. A rapid Strep test will give the answer.
- Impetigo often spreads and increases in number from scratching.
When to Call for Impetigo - Infected Sores
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Self Care at Home
|
Call Doctor or Seek Care Now
- Pink or tea-colored urine
- Fever and spreading redness around the impetigo
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Call Doctor Within 24 Hours
- Spreading redness around the impetigo and no fever
- Fever or sore throat are present
- Sore is larger than 1 inch (2.5 cm) across
- Sores and crusts inside the nose
- Impetigo gets worse after 48 hours on antibiotic ointment
- You think your child needs to be seen, but the problem is not urgent
Call Doctor During Office Hours
- Impetigo in 2 or more children (such as siblings or play groups)
- Child plays contact sports. Reason: to prevent spread.
- 3 or more impetigo sores. Reason: may need an oral antibiotic. Many of these children also have a Strep throat.
- Not healed up after 1 week on antibiotic ointment
- You have other questions or concerns
Self Care at Home
- Mild impetigo (1 or 2 sores that started with a scratch or insect bite)
Care Advice for Impetigo
-
What You Should Know About Impetigo:
- Impetigo is a skin infection. Most often, it starts in a scratch or insect bite.
- It usually responds to treatment with any antibiotic ointment.
- Here is some care advice that should help.
-
Remove Scabs:
- Soak off the scab using soap and warm water. The bacteria live underneath the scab.
-
Antibiotic Ointment:
- Put an antibiotic ointment (such as Polysporin) on the sores. No prescription is needed. You can also use one you already have.
- Do this 3 times per day.
- Cover it with a bandage (such as Band-Aid) to prevent scratching and spread.
- Repeat the washing, ointment and dressing 3 times per day.
-
Do Not Pick at the Sores:
- Help your child not to scratch and pick at the sores. This spreads the impetigo.
-
Return to School:
- Impetigo is spread to others by contact with skin lesions.
- Wash the hands often. Try not to touch the sores.
- For mild impetigo (1 or 2 sores), can go to school if it is covered.
- For severe impetigo, child needs to take an oral antibiotic for more than 24 hours. Then your child can go back to school.
- Contact Sports. In general, needs to be on antibiotics for 3 days before returning to sports. There must be no pus or drainage. Check with the team's trainer if there is one.
-
What to Expect:
- Sore stops growing in 1 to 2 days.
- The skin is healed in 1 week.
-
Call Your Doctor If:
- Impetigo sore gets bigger after 48 hours on antibiotic ointment
- Gets new impetigo sore on antibiotic ointment
- Not healed up in 1 week
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.
Infection Exposure Questions
- This topic includes information about transmission of common infections. How long to stay out of school or child care is covered.
- Incubation Period. Time it takes to start having symptoms after contact with infection.
- Contagious Period. Time during which a sick child's disease can spread to others. Sometimes, children can return to school before this period is over.
- Infections that cannot be spread to others, but there are a few exceptions. Your child's doctor will tell you for sure. Many common bacterial infections are not spread to others. Examples are ear, sinus, bladder, or kidney infections. Most pneumonia in children also can't be passed to others, but there are a few exceptions. Your child's doctor will tell you for sure. Sexually transmitted diseases are usually not spread to children. But, they can be spread if there is sexual contact or shared bathing.
Infection Exposure Table
| DISEASE |
INCUBATION PERIOD (DAYS) |
CONTAGIOUS PERIOD (DAYS) |
| Skin Infections/Rashes: | ||
| Chickenpox | 10-21 | 2 days before rash until all sores have crusts (6 - 7days) |
| Fifth disease (Erythema infectiosum) | 4-14 | 7 days before rash until rash begins |
| Hand, foot, and mouth disease | 3-6 | Onset of rash until fever gone. If widespread blisters, return after blisters are dry (6-7 days). |
| Impetigo (strep or staph) | 2-5 | Onset of sores until 24 hours on antibiotic |
| Lice | 7 | Onset of itch until 1 treatment |
| Measles | 8-12 | 4 days before rash until 4 days after rash appears |
| Roseola | 9-10 | Onset of fever until rash gone (2 days) |
| Rubella (German measles) | 14-21 | 7 days before rash until 5 days after rash appears |
| Scabies | 30-45 | Onset of rash until 1 treatment |
| Scarlet fever | 3-6 | Onset of fever or rash until 24 hours on antibiotic |
| Shingles (contagious for chicken pox) | 14-16 | Onset of rash until all sores have crusts (7 days) (Note: No need to isolate if sores can be kept covered.) |
| Warts | 30-180 | Minimally contagious |
| Respiratory Infections: | ||
| Bronchiolitis | 4-6 | Onset of cough until 7 days |
| Colds | 2-5 | Onset of runny nose until fever gone |
| Cold sores (herpes) | 2-12 | Footnote 1 |
| Coughs (viral) or croup (viral) | 2-5 | Onset of cough until fever gone |
| Diphtheria | 2-5 | Onset of sore throat until 4 days on antibiotic |
| Influenza | 1-2 | Onset of symptoms until fever gone |
| Sore throat, strep | 2-5 | Onset of sore throat until 24 hours on antibiotic |
| Sore throat, viral | 2-5 | Onset of sore throat until fever gone |
| Tuberculosis | 6-24 months | Until 2 weeks on drugs (Note: Most childhood TB is not contagious.) |
| Whooping cough | 7-10 | Onset of runny nose until 5 days on antibiotic |
| Intestinal Infections: | ||
| Diarrhea, bacterial | 1-5 | Footnote 2 for Diarrhea Precautions |
| Diarrhea, giardia | 7-28 | Footnote 2 for Diarrhea Precautions |
| Diarrhea, traveler's | 1-6 | Footnote 2 for Diarrhea Precautions |
| Diarrhea, viral (Rotavirus) | 1-3 | Footnote 2 for Diarrhea Precautions |
| Hepatitis A | 14-50 | 2 weeks before jaundice begins until jaundice resolved (7 days) |
| Pinworms | 21-28 | Minimally contagious, staying home is unnecessary |
| Vomiting, viral | 2-5 | Until vomiting stops |
| Other Infections: | ||
| Infectious mononucleosis | 30-50 | Onset of fever until fever gone (7 days) |
| Meningitis, bacterial | 2-10 | 7 days before symptoms until 24 hours on IV antibiotics in hospital |
| Meningitis, viral | 3-6 | Onset of symptoms and for 1-2 weeks |
| Mumps | 12-25 | 5 days before swelling until swelling gone (7 days) |
| Pinkeye without pus (viral) | 1-5 | Mild infection, staying home is unnecessary |
| Pinkeye with pus (bacterial) | 2-7 | Onset of pus until 1 day on antibiotic eyedrops |
Notes
Cold sores: Less than 6 years old, contagious until cold sores are dry (4-5 days). No isolation if sores are on part of body that can be covered. More than 6 years old, no isolation necessary if beyond touching, picking stage.
Diarrhea Precautions: Contagious until stools are formed. Stay home until fever is gone, diarrhea is mild, blood and mucus are gone, and toilet-trained child has control over loose stools. Shigella and E-coli 0157 require extra precautions. Consult your child care provider regarding attendance restrictions.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.
Influenza - Seasonal
Is this your child's symptom?
- Your child has symptoms of influenza (Flu) and it's in your community
- Main symptoms: fever AND one or more respiratory symptoms (cough, sore throat, very runny nose)
- Influenza (Flu) is a viral infection
- You think your child has influenza because other family members have it
- You think your child has influenza because close friends have it
If NOT, try one of these:
Symptoms of Influenza
- Main symptoms are a fever with a runny nose, sore throat, and bad cough.
- More muscle pain, headache, fever, and chills than with usual colds.
- If there is no fever, your child probably doesn't have flu. More likely he has a cold.
Cause of Influenza
- Influenza viruses that change yearly
Diagnosis: How to Know Your Child Has Influenza
- Influenza occurs every year in the fall and winter months. During this time, if flu symptoms occur, your child probably has the flu.
- Your child doesn't need any special tests.
- Call your doctor if your child is High-Risk for complications of the flu. See the list below. These are the children who may need prescription anti-viral drugs.
- For Low-Risk children, usually you don't need to see your child's doctor. If your child develops a possible complication of the flu, then call your doctor. See the "What to Do" section.
High-Risk Children for Complications From Influenza (AAP)
Children are considered High-Risk for complications if they have any of the following:
- Lung disease (such as asthma)
- Heart disease (such as a congenital heart disease)
- Cancer or weak immune system conditions
- Neuromuscular disease (such as muscular dystrophy)
- Diabetes, sickle cell disease, kidney disease or liver disease
- Diseases needing long-term aspirin therapy
- Pregnancy or severe obesity
- Healthy children under 2 years old are also considered High-Risk (CDC)
- Note: All other children are referred to as Low-Risk
Prescription Antiviral Drugs for Influenza
- Antiviral drugs (such as Tamiflu) are sometimes used to treat influenza. They must be started within 48 hours when the flu symptoms start. After 48 hours of fever, starting the drug is not helpful.
- The AAP recommends they be used for any patient with severe symptoms.
- The AAP recommends the drugs for most High-Risk children with underlying health problems. See that list.
- The AAP doesn't recommend antiviral drugs for Low-Risk children with mild flu symptoms.
- Their benefits are limited. They usually reduce the time your child is sick by 1 to 1.5 days. They reduce the symptoms, but do not make them go away.
- Side effects: Vomiting in 10% of children on Tamiflu.
- Most healthy children with flu do not need an antiviral drug.
When to Call for Influenza - Seasonal
Call 911 Now
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Self Care at Home
|
Call 911 Now
- Severe trouble breathing (struggling for each breath, can barely speak or cry)
- Lips or face are bluish when not coughing
- You think your child has a life-threatening emergency
Call Doctor or Seek Care Now
- Trouble breathing. Exception: present only when coughing.
- Breathing is much faster than normal
- Lips or face have turned bluish during coughing
- Wheezing (high-pitched purring or whistling sound when breathing out)
- Stridor (harsh sound with breathing in) is heard now
- Ribs are pulling in with each breath (retractions)
- Chest pain and can't take a deep breath
- Dehydration suspected. No urine in more than 8 hours, dark urine, very dry mouth and no tears.
- Not alert when awake ("out of it")
- Weak immune system. Examples are: sickle cell disease, HIV, cancer, organ transplant, taking oral steroids.
- Severe High-Risk child (see that list in Causes). This includes lung disease, heart disease, and bedridden.
- Age less than 12 weeks old with fever. Caution: do NOT give your baby any fever medicine before being seen.
- Fever over 104° F (40° C)
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Call Doctor Within 24 Hours
- High-Risk child for complications of flu. Includes children with other chronic diseases. (See that list in Causes). Also, includes healthy children less than 2 years old.
- Nonstop coughing spells
- Age less than 3 months old with any cough
- Earache or ear drainage
- Sinus pain (not just congestion)
- Fever lasts more than 3 days
- Fever returns after being gone more than 24 hours
- You think your child needs to be seen, but the problem is not urgent
Call Doctor During Office Hours
- Age more than 6 months and needs a flu shot
- Coughing causes vomiting 3 or more times
- Coughing has kept home from school for 3 or more days
- Nasal discharge lasts more than 2 weeks
- Cough lasts more than 3 weeks
- Flu symptoms lasts more than 3 weeks
- You have other questions or concerns
Self Care at Home
- Influenza with no complications and your child is Low-Risk
Care Advice for Influenza
-
What You Should Know About Influenza:
- Flu symptoms include cough, sore throat, runny nose, and fever. During influenza season, if your child has these symptoms, he probably has the flu.
- Most parents know if their child has flu. They have it too or it's in the school. It's also in the news. You don't need any special tests when you think your child has flu.
- If your child develops a complication of the flu, then call your child's doctor. Examples are an earache or trouble breathing. These problems are included in the "What to Do" section.
- For healthy people, the symptoms of influenza are like those of a bad cold.
- With flu, however, the onset is more abrupt. The symptoms are more severe. Feeling very sick for the first 3 days is common.
- The treatment of influenza depends on your child's main symptoms. It is no different from treatment used for other viral colds and coughs.
- Bed rest is not needed.
- Most children with flu don't need to see their doctor.
- Here is some care advice that should help.
-
Runny Nose with Lots of Discharge: Blow or Suction the Nose
- The nasal mucus and discharge is washing germs out of the nose and sinuses.
- Blowing the nose is all that's needed. Teach your child how to blow the nose at age 2 or 3.
- For younger children, gently suction the nose with a suction bulb.
- Put petroleum jelly on the skin under the nose. Wash the skin first with warm water. This will help to protect the nostrils from any redness.
-
Nasal Saline To Open a Blocked Nose:
- Use saline (salt water) nose spray to loosen up the dried mucus. If you don't have saline, you can use a few drops of water. Use distilled water, bottled water or boiled tap water.
- Step 1. Put 3 drops in each nostril. If under 1 year old, use 1 drop.
- Step 2. Blow (or suction) each nostril out while closing off the other nostril. Then, do the other side.
- Step 3. Repeat nose drops and blowing (or suctioning) until the discharge is clear.
- How Often. Do nasal saline rinses when your child can't breathe through the nose.
- Limit. If under 1 year old, no more than 4 times per day or before every feeding.
- Saline nose drops or spray can be bought in any drugstore. No prescription is needed.
- Saline nose drops can also be made at home. Use ½ teaspoon (2 mL) of table salt. Stir the salt into 1 cup (8 ounces or 240 mL) of warm water. Use bottled water or boiled water to make saline nose drops.
- Reason for nose drops: Suction or blowing alone can't remove dried or sticky mucus. Also, babies can't nurse or drink from a bottle unless the nose is open.
- Other option: use a warm shower to loosen mucus. Breathe in the moist air, then blow each nostril.
- For young children, can also use a wet cotton swab to remove sticky mucus.
-
Medicines for Flu:
- Cold Medicines. Don't give any drugstore cold or cough medicines to young children. They are not approved by the FDA under 6 years. Reasons: not safe and can cause serious side effects. Also, they are not helpful. They can't remove dried mucus from the nose. Nasal saline works best.
- Allergy Medicines. They are not helpful, unless your child also has nasal allergies. They can also help an allergic cough.
- No Antibiotics. Antibiotics are not helpful for flu. Antibiotics may be used if your child gets an ear or sinus infection.
-
Homemade Cough Medicine:
- Goal: Decrease the irritation or tickle in the throat that causes a dry cough.
- Age 3 months to 1 year: give warm clear fluids to treat the cough. Examples are apple juice and lemonade. Amount: use a dose of 1-3 teaspoons (5-15 mL). Give 4 times per day when coughing. Caution: do not use honey until 1 year old.
- Age 1 year and older: use Honey ½ to 1 teaspoon (2-5 mL) as needed. It works as a homemade cough medicine. It can thin the secretions and loosen the cough. If you don't have any honey, you can use corn syrup.
- Age 6 years and older: use Cough Drops to decrease the tickle in the throat. If you don't have any, you can use hard candy. Avoid cough drops before 6 years. Reason: risk of choking.
-
Sore Throat Pain Relief:
- Age over 1 year. Can sip warm fluids such as chicken broth or apple juice. Some children prefer cold foods such as popsicles or ice cream.
- Age over 6 years. Can also suck on hard candy or lollipops. Butterscotch seems to help.
- Age over 8 years. Can also gargle. Use warm water with a little table salt added. A liquid antacid can be added instead of salt. Use Mylanta or the store brand. No prescription is needed.
- Medicated throat sprays or lozenges are generally not helpful.
-
Fluids - Offer More:
- Try to get your child to drink lots of fluids.
- Goal: Keep your child well hydrated.
- It also will thin out the mucus discharge from the nose.
- It also loosens up any phlegm in the lungs. Then it's easier to cough up.
-
Fever Medicine:
- For fevers above 102° F (39° C), give an acetaminophen product (such as Tylenol).
- Another choice is an ibuprofen product (such as Advil).
- Avoid Aspirin because of the strong link with Reye syndrome.
- Note: Fevers less than 102° F (39° C) are important for fighting infections.
- For all fevers: Keep your child well hydrated. Give lots of cold fluids.
-
Pain Medicine:
- For muscle aches or headaches, give an acetaminophen product (such as Tylenol).
- Another choice is an ibuprofen product (such as Advil).
- Use as needed.
-
Prescription Antiviral Drugs for Influenza:
- Antiviral drugs (such as Tamiflu) are sometimes used to treat influenza. They must be started within 48 hours of when flu symptoms start. After 48 hours of fever, starting the drug is not helpful.
- The AAP recommends they be used for any patient with severe symptoms. They also recommend the drugs for most High-Risk children. See that list in Causes.
- If your child has a chronic disease and gets the flu, call your doctor. The doctor will decide if your child needs a prescription.
- The AAP doesn't recommend antiviral drugs for Low-Risk children with normal flu symptoms.
- Their benefits are limited. They reduce the time your child is sick by 1 to 1 ½ days. They reduce the symptoms, but do not make them go away.
- Side effects: Vomiting in 10% of children on Tamiflu.
- Most healthy children with flu do not need an antiviral drug.
- Also, it is not used to prevent flu. Reason: You would need to take the medicine every day for months.
-
Return to School:
- Spread is rapid, and the virus is easily passed to others.
- The time it takes to get the flu after contact is about 2 days.
- Your child can return to school after the fever is gone for 24 hours.
- Your child should feel well enough to join in normal activities.
-
What to Expect:
- Influenza causes a cough that lasts 2 to 3 weeks.
- Sometimes your child will cough up lots of phlegm (mucus). The mucus can be grey, yellow or green. This is normal.
- Coughing up mucus is very important. It helps protect the lungs from pneumonia.
- We want to help a productive cough, not turn it off.
- The fever lasts 2 to 3 days.
- The runny nose lasts 7 to 14 days.
-
Prevention: How to Protect Yourself from Getting Sick:
- Wash hands often with soap and water.
- Alcohol-based hand cleaners also work well.
- Avoid touching the eyes, nose or mouth. Germs on the hands can spread this way.
- Try to avoid close contact with sick people.
- Avoid ERs and urgent care clinics if you don't need to go. These are places where you are more likely to be exposed to flu.
-
Prevention: How to Protect Others - Stay Home When Sick:
- Cover the nose and mouth with a tissue when coughing or sneezing.
- Wash hands often with soap and water. After coughing or sneezing are important times.
- Limit contact with others to keep from infecting them.
- Stay home from school for at least 24 hours after the fever is gone. (CDC).
-
Flu Shot and Prevention:
- Getting a flu shot is the best way to protect your family from flu.
- Influenza vaccines are strongly advised for all children over 6 months of age. (AAP)
- Adults should also get the shot.
- The shot most often prevents the disease.
- Even if your child gets the flu, the shot helps to reduce the symptoms.
- A new flu shot is needed every year. Reason: Flu viruses keep changing.
- After the flu shot, it takes 2 weeks to fully protect from flu. But then, the protection lasts for the full flu season. An antiviral medicine only protects from flu while taking it.
-
Call Your Doctor If:
- Trouble breathing occurs
- Retractions (pulling in between the ribs) occur
- Dehydration occurs
- Earache or sinus pain occurs
- Fever lasts more than 3 days or goes above 104° F (40° C)
- Nasal discharge lasts more than 14 days
- Cough lasts more than 3 weeks
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.
Influenza Exposure
Is this your child's symptom?
- Exposure (Close Contact) to a person with influenza
- Questions about influenza
- Your child has no symptoms of influenza (no fever, cough, sore throat, runny nose)
- For children with symptoms of influenza, see the Influenza care guide.
If NOT, try one of these:
Flu Exposure (Close Contact) Definition
- Household Close Contact. Lives with a person with flu.
- Other Close Contact. The CDC defines 6 feet as how far coughing can spread the flu virus. How long the close contact lasts is also important. Close contact includes kissing, hugging or sharing eating and drinking utensils. It also includes close conversations. Direct contact with secretions of a person with flu is also close contact. Includes being in the same child care center room or carpool.
- In Same Building - Not Close Contact. Walking by a person or sitting in a room briefly is not close contact. Being in the same school, church, workplace or building also is not close contact.
- In Same Town - Not Close Contact. Living in a town where there are people with the flu is not close contact. Living in the same state or country (such as Mexico) carries no added risk.
High-Risk Children for Complications From Influenza (AAP)
Children are considered High-Risk for complications if they have any of the following:
- Lung disease (such as asthma)
- Heart disease (such as a congenital heart disease)
- Cancer or weak immune system conditions
- Neuromuscular disease (such as muscular dystrophy)
- Diabetes, sickle cell disease, kidney disease or liver disease
- Diseases requiring long-term aspirin therapy
- Pregnancy or severe obesity
- All healthy children under 2 years old are also considered High-Risk (CDC 2009)
- Note: All other children are referred to as Low-Risk
Prescription Antiviral Drugs for Influenza
- Antiviral drugs (such as Tamiflu) are sometimes used to treat influenza. They must be started within 48 hours of when flu symptoms start.
- The AAP recommends they be used for any patient with severe symptoms.
- The AAP also recommends the drugs for most High-Risk children. A list of High-Risk problems is also on the CDC website.
- The AAP doesn't recommend antiviral drugs for Low-Risk children with mild flu symptoms.
- Their benefits are limited. They usually reduce the time your child is sick by 1 to 1.5 days. They reduce the symptoms, but do not make them go away.
- Side effects: Vomiting in 10% of children.
When to Call for Influenza Exposure
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Self Care at Home
|
Call Doctor Within 24 Hours
- Influenza Close Contact within last 7 days and your child is High-Risk. See the list of children at High-Risk in Causes for complications of flu.
Call Doctor During Office Hours
- Age more than 6 months and needs a flu shot
- You have other questions or concerns
Self Care at Home
- Influenza questions and no Close Contact in the last 7 days
- Influenza prevention questions
- Tamiflu prescription questions
- Influenza Close Contact within the last 7 days, but Low-Risk or healthy child
- Influenza Minor Contact (same school or gathering), but no Close Contact
Care Advice
Influenza Questions and No Close Contact in the Last 7 days
-
What You Should Know About Flu Exposure:
- For most healthy people, the symptoms of influenza are like those of a bad cold.
- But, with flu, the onset is more abrupt. The symptoms are more severe.
- Feeling very sick for the first 3 days is common.
- The treatment of influenza depends on your child's main symptoms. It is no different from treatment used for other viral colds and coughs.
- Most children with flu don't need to see their doctor.
-
Influenza Symptoms:
- The main symptoms are fever, cough, sore throat and runny nose.
- Most often, fever is present. (Exception: Sometimes, no fever if the child has a weak immune system.)
- Other common symptoms are muscle pain, headache and fatigue.
- Some people also have vomiting and diarrhea, but never as the only symptom.
-
Influenza Diagnosis and Flu Tests:
- During influenza season, if your child has flu symptoms, he probably has the flu.
- Your child won't need any special tests.
- You should call your doctor if your child is High-Risk for complications of flu. These are children with chronic diseases. Examples of such diseases are asthma or a weak immune system. See the High-Risk list in Causes. Also, healthy children under 2 years of age are High-Risk.
- For Low-Risk children, you don't need to see your child's doctor.
- If your child develops a complication of the flu, then call your child's doctor. Examples of complications are an earache or trouble breathing. These problems are included in the "What to Do" section.
-
Influenza Treatment:
- For most children, the treatment of flu is based upon symptom relief. It's no different than the treatment of other viral coughs and colds.
- Tamiflu is the main antiviral drug used to treat influenza in some children.
- The AAP recommends it be used for any patient with severe symptoms.
- The AAP also recommends the drug for most High-Risk children. See that list in Causes. Mainly, it is used for children in the hospital or those with chronic diseases.
- Treatment is not recommended for Low-Risk children with normal flu symptoms. (AAP)
- Most patients recover without taking Tamiflu.
- Antiviral treatment must be started within 48 hours of the onset of flu symptoms. After 48 hours of fever, starting the drug is not helpful.
-
Return to School:
- Spread is rapid and the virus is easily passed to others. The time it takes to get the flu after contact is about 2 days. The range is 1-4 days.
- Your child can return to school after the fever is gone for 24 hours. (CDC).
- The influenza virus is spread in the air from sneezing and coughing.
- It also can be spread by the hands with flu germs on them.
-
What to Expect:
- The fever lasts 2 -3 days.
- The runny nose lasts 1-2 weeks.
- The cough lasts 2-3 weeks.
-
Call Your Doctor If:
- You have other questions or concerns
Influenza Prevention Questions
-
How to Protect Yourself From Getting Sick:
- Wash hands often with soap and water.
- Alcohol-based hand cleaners work very well.
- Avoid touching the eyes, nose or mouth. Germs on the hands can spread this way.
- Try to avoid close contact with sick people.
- Avoid ERs and urgent care clinics if you don't need to go. These are places where you are more likely to be exposed to flu.
-
How To Protect Others - Stay Home When Sick:
- Cover the nose and mouth with a tissue when coughing or sneezing.
- Wash hands often with soap and water. After coughing or sneezing are important times. Alcohol-based hand cleaners also work well.
- Limit contact with others to avoid getting them sick.
- Stay home from school or work while sick with fever. Your child can return to school after the fever is gone for 24 hours. (CDC).
-
Flu Shot:
- Getting a flu shot is the best way to protect your family from flu.
- Influenza vaccines are strongly advised for all children over 6 months of age. (AAP)
- Adults should also get the shot.
- The flu shot most often prevents the disease.
- Even if your child gets the flu, the shot helps to reduce the symptoms.
- A new flu shot is needed every year. Reason: Flu viruses keep changing.
- After the flu shot, it takes 2 weeks to fully protect from flu. But then, the protection lasts for the full flu season. An antiviral medicine only protects from flu while taking it.
-
Antiviral Drug (such as Tamiflu):
- The drug Tamiflu may help prevent flu after close contact. But, it is only advised for some very High-Risk patients (CDC). See the High-Risk list.
- The CDC recommends early treatment if flu symptoms occur, not preventive treatment. Reasons: Even after close contact, some children don't get flu. Also, Tamiflu is helpful only while your child is taking it. It won't prevent flu once your child stops taking it. To prevent flu, you would need to take the medicine every day for months.
- Most doctors also wait until flu symptoms start before treating with drugs.
- If your child is High-Risk, call your doctor within 24 hours of exposure. Your doctor will decide if an antiviral is needed.
- High-Risk adults with recent close contact should also call their doctor. The High-Risk adult group includes chronic disease, pregnant, or over 65.
-
Call Your Doctor If:
- You have other questions or concerns
Tamiflu Prescription Questions
-
Treating Influenza - Tamiflu:
- Tamiflu is a prescription anti-viral drug. It can be helpful in treating the flu virus.
- These drugs should be started within 48 hours of when flu symptoms start. After 48 hours of fever, starting the drug is not helpful. It's taken for a total of 5 days.
- When to Use: Severe symptoms OR underlying health problems (High-Risk group)
- For High-Risk children, call your child's doctor at the start of flu symptoms.
- Most healthy patients have mild to moderate symptoms. Tamiflu treatment is not needed for these patients.
- The benefits are limited. Tamiflu reduces the time your child is sick by 1 to 1.5 days. It helps reduce the symptoms, but does not make them go away.
- Tamiflu also has side effects. It causes vomiting in 10% of children.
- Also, it is not used to prevent flu. Reason: You would need to take the medicine every day for months.
-
Personal Stockpiling of Tamiflu - Not Advised:
- Some people want a prescription for Tamiflu for all family members. They want it on hand just in case they come down with flu. They currently are well and have not been exposed to flu.
- Doctors and the CDC are opposed to this practice. The AAP and your State's Public Health Department also do not support this.
- The supply of Tamiflu is limited. It is used for those with severe symptoms OR who are High-Risk.
-
Call Your Doctor If:
- You have other questions or concerns
Influenza Close Contact Within the Last 7 Days but Low-Risk child
-
What You Should Know:
- Although your child was exposed to flu, your child does not have any symptoms.
- Symptoms usually develop within 1-4 days of seasonal flu contact. 7 days is an outer limit.
- Even if your child gets the flu, your child most likely will do fine. Anti-viral treatment (Tamiflu) is not needed for Low-Risk children.
- Healthy children get better from flu by treating the symptoms.
-
Call Your Doctor If:
- You have other questions or concerns
Influenza Minor Contact (same school) but No Close Contact
-
What You Should Know:
- To catch influenza, your child needs to have close contact with an infected person.
- Close contact includes kissing, hugging, or sharing eating or drinking utensils. It also includes close conversations within 6 feet (2 meters) (CDC 2013). Being in the same child care group or car pool is also close contact.
- Being in the same school, church or building is not close contact.
- If there was no close contact, your child probably will not get the flu.
- Anti-viral medicine (Tamiflu) is not needed for Low-Risk children.
- Healthy children get better from flu by treating the symptoms.
-
Call Your Doctor If:
- You have other questions or concerns
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.
Insect Bite
Is this your child's symptom?
- Bite from an insect (bug)
- Bees, mosquitoes, fire ants, ticks and spiders are not covered. See those care guides.
If NOT, try one of these:
Symptoms of Insect Bites
- Insect bites usually cause a small red bump.
- Often, it looks like localized hives (one large one or several small ones).
- Sometimes, a small water blister occurs in the center of the bump. This is common in younger children.
- Itchy Insect Bites. Bites of mosquitoes, chiggers (harvest mites), fleas, and bedbugs usually cause itchy, red bumps.
- Painful Insect Bites. Bites of horseflies, deer flies, and gnats usually cause a painful, red bump. Fire ants, harvester ants, blister beetles, and centipedes also cause a painful, red bump. Within a few hours, fire ant bites can change to blisters or pimples.
Cause of Insect Bite Reaction
- The skin bumps are the body's reaction to the insect's saliva.
- While the bug is sucking blood, some of its secretions get mixed in.
Anaphylaxis With Insect Bites: Very Rare
- A severe life-threatening allergic reaction is called anaphylaxis.
- The main symptoms are difficulty breathing and swallowing starting within 2 hours of the sting. Onset usually is within 20 minutes.
- Anaphylaxis can occur with bee, yellow jacket, wasp, or fire ant stings. Anaphylactic reactions are very rare after other insect bites. Reason: other insects don't have venom.
Problems Caused by Insect Bites
- Impetigo. A local bacterial infection. Gives sores, soft scabs and pus. Caused by scratching or picking at the bites. More common in itchy bites.
- Cellulitis. The bacterial infection spreads into the skin. Gives redness spreading out from the bite. The red area is painful to the touch.
- Lymphangitis. This is a bacterial infection that spreads up the lymph channels. Gives a red line that goes up the arm or leg. More serious because the infection can get into the bloodstream. (This is called sepsis.)
When to Call for Insect Bite
Call 911 Now
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Self Care at Home
|
Call 911 Now
- Past life-threatening allergic reaction to same insect bite (not just hives) and bitten less than 2 hours ago
- Trouble breathing or wheezing
- Hoarse voice, cough, or tightness in the throat or chest
- Trouble swallowing, drooling or slurred speech
- Hard to wake up
- Acts or talks confused
- You think your child has a life-threatening emergency
Call Doctor or Seek Care Now
- Hives or swelling all over the body
- More than 20 fire ant stings in a child less than 1 year old
- Fever and bite looks infected (spreading redness)
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Call Doctor Within 24 Hours
- Severe pain and not better 2 hours after taking pain medicine
- New redness around the bite starts more than 24 hours after the bite
- More than 48 hours since the bite and redness gets larger
- Redness or red streak around the bite gets larger than 1 inch (2.5 cm)
- You think your child needs to be seen, but the problem is not urgent
Call Doctor During Office Hours
- Scab that looks infected (drains pus or gets bigger) not better with antibiotic ointment
- You have other questions or concerns
Self Care at Home
- Normal insect bite
- Questions about insect repellents (such as DEET)
Care Advice for Insect Bites
Treatment for Insect Bites
-
What You Should Know About Insect Bites:
- Most insect bites cause a red bump. Some are larger (like a hive). Some have a small water blister in the center. These are normal reactions to an insect bite.
- A large hive at the bite does not mean your child has an allergy.
- The redness does not mean the bite is infected.
- Here is some care advice that should help.
-
Itchy Insect Bite Treatment:
- Steroid Cream. To reduce the itching, use 1% hydrocortisone cream (such as Cortaid). No prescription is needed. Put it on 3 times a day until the itch is gone. If you don't have, use a baking soda paste until you can get some.
- If neither is available, use ice in a wet washcloth for 20 minutes.
- Also, you can put firm, sharp, direct, steady pressure on the bite. Do this for 10 seconds to reduce the itch. A fingernail, pen cap, or other object can be used.
- Allergy Medicine. If the bite is still itchy, try an allergy medicine (such as Benadryl). No prescription is needed. Sometimes it helps, especially in allergic children.
-
Painful Insect Bite Treatment:
- Soak a cotton ball in a baking soda solution. Rub the bite with it for 15 to 20 minutes. Do this once. This will usually reduce the pain.
- You can also use an ice cube in a wet washcloth for 20 minutes.
- To help with the pain, give an acetaminophen product (such as Tylenol). Another choice is an ibuprofen product (such as Advil). Use as needed.
- For painful bites, allergy medicines don't help.
-
Antibiotic Ointment for Infected Bite:
- If the insect bite has a scab on it and the scab looks infected, use an antibiotic ointment. An example is Polysporin. No prescription is needed. Use 3 times per day. (Note: Usually impetigo is caused by scratching with dirty fingers).
- Cover the scab with a bandage (such as Band-Aid). This will help prevent scratching and spread.
- Wash the sore and use the antibiotic ointment 3 times per day. Cover it with a clean bandage each time. Do this until healed.
- Caution: For spreading infections (redness or red streaks), your child needs to be seen.
-
What to Expect:
- Most insect bites are itchy for several days.
- Any pinkness or redness usually lasts 3 days.
- The swelling may last 7 days.
- Insect bites of the upper face can cause severe swelling around the eye. This is harmless.
- The swelling is usually worse in the morning after lying down all night. It will improve after standing for a few hours.
-
Call Your Doctor If:
- Severe pain lasts more than 2 hours after pain medicine
- Infected scab not better after 48 hours of antibiotic ointment
- Bite looks infected (spreading redness gets bigger after 48 hours)
- You think your child needs to be seen
- Your child becomes worse
Prevention of Insect Bites
-
Prevention Tips:
- Wear long pants, a long-sleeved shirt and a hat.
- Avoid being outside when the bugs are most active. Many insects that cause itchy bites are most active at sunrise or sunset. Examples are chiggers, no-see-ums, and mosquitoes.
- Insect repellents that contain DEET are helpful in preventing many insect bites. Read the label carefully.
-
DEET Products: Use on the Skin.
- DEET is a very effective bug repellent. It also repels ticks and other insects.
- The AAP approves DEET use over 2 months of age. Use 30% DEET or less. Use 30% DEET if you need 6 hours of protection. Use 10% DEET if you only need protection for 2 hours. (AAP 2003).
- Don't put DEET on the hands if your child sucks on their thumb or fingers. (Reason: prevent swallowing DEET.)
- Warn older children who apply their own DEET to use less. A total of 3 or 4 drops can protect the whole body.
- Put it on exposed areas of skin. Do not use near the eyes or mouth. Do not use on skin that is covered by clothing. Don't put DEET on sunburns or rashes. Reason: DEET can be easily absorbed in these areas.
- Wash it off with soap and water when your child comes indoors.
- Caution: DEET can damage clothing made of man-made fibers. It can also damage plastics (such as eye glasses) and leather. DEET can be used on cotton clothing.
-
Permethrin Products: Use on Clothing.
- Products that contain permethrin (such as Duranon) work well to repel insects and ticks.
- Unlike DEET, these products are put on clothing instead of skin.
- Put it on shirt cuffs, pant cuffs, shoes and hats.
- You can also use it on other outdoor items (mosquito screens, sleeping bags).
- Do not put permethrin on the skin. Reason: Sweat changes it so it does not work.
-
Picaridin Products:
- Picaridin is a repellent that is equal to 10% DEET.
- It can safely be put on skin or clothing.
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.
Jaundiced Newborn
Is this your child's symptom?
- Jaundice (yellow skin) in a baby during the first months of life
- The skin turns a yellow color from high bilirubin levels in the blood
Jaundice and Bilirubin
- Jaundice means the skin has turned yellow.
- Bilirubin is the pigment that turns the skin yellow.
- Bilirubin comes from the normal breakdown of old red blood cells.
- The liver normally gets rid of bilirubin. But, at birth, the liver may be immature.
- Half of babies have some jaundice. Usually it is mild.
- The level of bilirubin that is harmful is around 20. Reaching a level this high is rare.
- High levels need to be treated with bili-lights. That's why your doctor checks your baby's bilirubin levels until it becomes low.
Causes of Jaundice in Newborns
Physiological Jaundice (50% of newborns)
- Onset 2 to 3 days of age
- Peaks day 4 to 5, then improves
- Disappears 1 to 2 weeks of age
Breastfeeding or Malnutrition Jaundice (5 to 10% of newborns)
- Due to inadequate intake of breastmilk
- Pattern similar to physiological type
- Also, causes poor weight gain
Breastmilk Jaundice (10% of newborns)
- Due to substance in breastmilk which blocks removal of bilirubin
- Onset 4 to 7 days of age
- Lasts 3 to 12 weeks
- Not harmful
Rh and ABO Blood Group Incompatibility (Serious, but Rare)
- Onset during first 24 hours of life
- Can reach harmful levels
Liver Disease (Serious, but Rare)
- The main clue is light gray or pale yellow stools
- The jaundice doesn't go away
- Causes include liver infection (hepatitis) and liver blockage (biliary atresia)
When to Call for Jaundiced Newborn
Call 911 Now
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Self Care at Home
|
Call 911 Now
- Can't wake up
- Not moving or very weak
- You think your child has a life-threatening emergency
Call Doctor or Seek Care Now
- Age less than 1 month old and looks or acts abnormal in any way
- Feeding poorly (such as poor suck, does not finish)
- Hard to wake up
- Dehydration suspected. No urine in more than 8 hours, dark urine, very dry mouth and no tears.
- Fever. Caution: do NOT give your baby any fever medicine before being seen.
- Low temperature below 96.8° F (36.0° C) rectally that does not go up with warming
- Jaundice began during the first 24 hours of life
- Skin looks deep yellow or orange
- Jaundice has reached the legs
- Jaundice worse than when last seen
- You think your child needs to be seen, and the problem is urgent
Call Doctor Within 24 Hours
- High-risk baby for severe jaundice. Risk factors are: premature baby born at 36 weeks or less, ABO or Rh blood group problem, sib needed bili-lights, bleeding in the scalp, Asian race, breastfeeding problems.
- Whites of the eyes have turned yellow
- Jaundice spreads to stomach (belly)
- You are worried about the amount of jaundice
- You are worried your baby is not getting enough breastmilk
- Yellow, seedy stools are less than 3 per day. Exception: breastfed and before 5 days of life.
- Day 2-4 of life and no stool in more than 24 hours and breastfed
- Wet diapers are less than 6 per day. Exception: 3 wet diapers per day can be normal before 5 days of life if breastfed.
- 4 or more days old and has not been checked since discharge
- You think your child needs to be seen, but the problem is not urgent
Call Doctor During Office Hours
- Color gets deeper yellow after 7 days old
- Jaundice is not gone after 14 days of age
- Jaundice began or comes back after 7 days of age
- Stools are white, pale yellow or gray
- You have other questions or concerns
Self Care at Home
- Mild jaundice of newborn
Care Advice for Mild Jaundice
-
What You Should Know About Newborn Jaundice:
- Some jaundice is present in 50% of newborns.
- It lasts a short time and will go away. Most often, it is harmless.
- The first place for jaundice to start is on the face.
- Jaundice that is only of the face is always harmless.
- Here is some care advice that should help.
-
Bottle Feed More Often:
- If bottle fed, increase how often you feed your baby.
- Try to feed every 2 to 3 hours during the day.
- Don't let your baby sleep more than 4 hours at night without a feeding.
-
Breastfeed More Often:
- If breastfed, increase how often your feed your baby.
- Nurse your baby every 1½ to 2 hours during the day.
- Don't let your baby sleep more than 4 hours at night without a feeding.
- Goal: At least 10 feedings every 24 hours.
-
Infrequent Stools Means Your Baby Needs More Milk:
- Breastmilk and formula help carry bilirubin out of the body. Therefore, good feedings are important for bringing down the bilirubin level.
- In the first month, keep track of how many stools are passed daily. The number of stools reflects how much milk your baby is getting.
- If your baby is 5 days or older, he should have at least 3 stools daily. If stooling less than that, it usually means your baby needs more to eat.
- Try to increase the number and amount of feedings per day.
- If you are having any trouble with breastfeeding, consult a lactation expert. Also, schedule a weight check.
-
What to Expect:
- Physiological jaundice peaks on day 4 or 5.
- It slowly goes away over 1-2 weeks.
-
Judging Jaundice:
- Jaundice starts on the face and moves downward. Try to determine where it stops.
- View your baby unclothed in natural light near a window.
- Press on the skin with a finger to remove the normal skin tone.
- Then try to look if the skin is yellow before the pink color returns.
- Move down the body, doing the same. Try to look where the yellow color stops.
- Jaundice that only involves the face is harmless. As it involves the chest, the level is going up. If it involves the eyes, stomach, arms or legs, the bilirubin level needs to be checked.
-
Call Your Doctor If:
- Jaundice gets worse
- Whites of the eyes turn yellow
- Belly or legs turn yellow
- Feeds poorly or has a weak suck
- Baby starts to look or act abnormal
- Jaundice lasts more than 14 days
- You think your child needs to be seen
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.
Jellyfish Sting
Is this your child's symptom?
- Sting from a jellyfish
- Jellyfish cause most of the stings that occur in sea water
- The creature's stinger injects venom into the human skin. This is what causes the sting.
- The main symptoms are pain, burning and redness at the sting site. Red lines are common.
- The Sea Nettle is a type of stinging jellyfish often found in Chesapeake Bay
If NOT, try one of these:
Jellyfish Facts
- They are umbrella shaped, clear sea creatures with long trailing tentacles. They move slowly through the water by pulsing the upper body. Also carried by ocean currents. Their tentacles can be 10 feet or longer.
- Other Names. Jellies or sea jellies. Large groups of jellies are called a bloom. Blooms can close beaches.
- Where They Live. Found in every ocean and coastline.
- Numbers. Jellies have increased in numbers worldwide. Warmer ocean temps and pollution of ocean waters are factors. Fishing the ocean too much is also a cause. Tuna, shark and swordfish eat jellies.
- Stings. Stings can occur while wading, swimming or diving in salt water. Honolulu gets over 1000 911 calls per month for stings.
- Beached Jellies. Even beached or dying jellies can sting. So can pieces of tentacles floating in the water. They can release venom for up to 2 weeks.
- Treatment. Vinegar is used to stop the venom in stingers. Caution: Do not use ammonia, urine, rubbing alcohol, fresh water or ice. They all can trigger the release of more venom. If you don't have vinegar, move on to scraping off the stingers.
- Prevention. Mainly do not go in the water where jellies are seen. Wearing a thin layer of clothing (such as pantyhose) also can protect you. Reason: The stingers are short and cannot puncture clothing. Special "stinger suits" can be bought in diving stores.
Cause of Sting Reactions
- The long tentacles have thousands of stingers.
- When a stinger is touched, it pierces the skin and injects venom.
- The venom is what causes all the symptoms.
Types of Jellyfish Sting Reactions
- Local Reactions are most common. Symptoms are raised, red lines that cross each other. The sting causes pain or burning at the site. Sometimes hives in the sting area occur. Blisters can occur in severe cases. Severe pain lasts 1-2 hours. Itch may last for a week. If the skin damage is severe, red or purple lines can last for weeks.
- General Reactions can occur if there are many stings. More stings give a higher dose of venom. Large venom symptoms are vomiting, dizziness, weakness and headache.
- Anaphylaxis (A severe allergic reaction). Life-threatening reactions are very rare with the stings. Most are caused by box jellyfish found in the South Pacific and Australia. The main symptoms are trouble breathing and swallowing, along with hives. It starts rapidly, most often within 20 minutes of the sting.
When to Call for Jellyfish Sting
Call 911 Now
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Self Care at Home
|
Call 911 Now
- Past severe allergic reaction to jellyfish stings (not just hives) and stung less than 2 hours ago
- Wheezing or trouble breathing
- Hoarseness, cough or tightness in the throat or chest
- Trouble swallowing or drooling
- Speech is slurred
- Acts or talks confused
- Passed out (fainted) or too weak to stand
- You think your child has a life-threatening emergency
Call Doctor or Seek Care Now
- Sting inside the mouth
- Sting on the eye
- Sting covers a large area (more than 1 arm or leg)
- Stomach pain or vomiting
- Fever and sting looks infected (spreading redness)
- Severe pain not improved after 2 hours using care advice
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Call Doctor Within 24 Hours
- Blisters appear
- More than 48 hours since the sting and redness getting larger
- You think your child needs to be seen, but the problem is not urgent
Call Doctor During Office Hours
- Severe itching not better after 24 hours of using steroid cream
- Redness or rash lasts more than 48 hours
- Last tetanus shot was more than 10 years ago
- You have other questions or concerns
Self Care at Home
- Jellyfish sting - Normal local reaction
Care Advice for Jellyfish Sting
-
What You Should Know About Jellyfish Stings:
- Jellyfish cause most of the stings that occur in the ocean.
- Most stings are harmless. The pain is like a bee sting.
- Jellies have long tentacles with lots of tiny stingers.
- Pieces of tentacles that wash up on the beach can still cause stings.
- They produce lines of redness and burning pain.
- Here is some care advice that should help.
-
Step 1 - Sea Water Rinse to Remove Large Tentacles:
- Rinse area with sea water. This will help remove any large tentacles stuck to the skin.
- Do not rinse with fresh water (will trigger stingers).
- Do not scrub or rub area (will trigger stingers).
- Do this until you can get some vinegar.
-
Step 2 - Vinegar Rinse to Stop the Stinging: (Exception: Chesapeake Bay jellyfish - see #6)
- Rinse area with vinegar (5% acetic acid) for 15 minutes.
- Reason: Stops the stingers from stinging if still attached to the skin.
- Caution: Do not use with Chesapeake Bay jellyfish. (Reason: May trigger stingers. Instead, use a baking soda rinse with these stings).
- Avoid rubbing alcohol for all stings. Reason: will trigger the stingers.
- If you can't get vinegar, move on to scraping off the stingers.
-
Step 3 - Scrape the Area to Remove Small Stingers:
- Scrape off any stingers you can see. Use the edge of a credit card or dinner knife.
- Do not use your bare fingers. (Reason: you will get stings on your hands). Put on gloves if you have them.
- Then, coat area with shaving cream or any mild cream. Scrape the area again.
- If the stingers are stuck to body hair, shave with a razor.
-
Step 4 - Repeat Vinegar Rinse: (Exception: Chesapeake Bay Jellyfish - go to #6)
- Keep a cloth wet with vinegar on the area.
- Do this for 15 more minutes.
-
Chesapeake Bay Jellyfish (Sea Nettle) - Baking Soda Rinse To Stop The Stinging:
- Rinse area with a mixture of sea water and baking soda for 15 minutes.
- This stops the stingers from stinging if still attached to the skin.
- Then, remove small stingers with scraping or shaving.
- Caution: Do not use vinegar rinse.
-
Pain Medicine:
- To help with the pain, give an acetaminophen product (such as Tylenol).
- Another choice is an ibuprofen product (such as Advil).
- Use as needed.
-
Cold Pack for Pain:
- For pain and swelling, rub with an ice cube. You can also use a cold wet washcloth. Do this for 10 minutes as needed.
- Caution: Don't use until stingers are removed. (Reason: water or ice will trigger stingers).
-
Steroid Cream for Itching:
- For itching or swelling, put 1% hydrocortisone cream (such as Cortaid) on the sting.
- No prescription is needed.
- Use 3 times per day.
- Keep the cream in the fridge. (Reason: it feels better if put on cold).
-
What to Expect:
- Minor stings: Severe burning pain will lessen within 1-2 hours. Red blotches and lines often improve in 24 hours. Red lines may last 1-2 weeks.
- More severe stings: Blisters appear within 6 hours. You should be seen by a doctor if blisters appear.
-
Call Your Doctor If:
- Blisters appear
- Severe pain persists over 2 hours
- Redness or rash lasts over 2 weeks
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.
Leg Injury
Is this your child's symptom?
- Injuries to the leg (hip to foot)
- Injuries to a bone, muscle, joint or ligament
- Muscle pain caused by too much exercise or work (overuse). Overuse is covered in Leg Pain.
If NOT, try one of these:
Types of Leg Injuries
- Fracture. This is the medical name for a broken bone. The most common broken bone in the leg is the tibia. The tibia is the largest bone in the lower part of the leg. Children with a fracture are not able to bear weight or walk.
- Dislocation. This happens when a bone is pulled out of its joint. The most common one in the leg is a dislocated kneecap (patella).
- Sprains. Sprains are stretches and tears of ligaments. A sprained ankle is the most common ligament injury of the leg. It's usually caused by turning the ankle inward. Also, called a "twisted ankle." The main symptoms are pain and swelling of the outside of the ankle.
- Strains. Strains are stretches and tears of muscles (a pulled muscle)
- Muscle Overuse. Muscle pain can occur without an injury. There is no fall or direct blow. Muscle overuse injuries are from sports or exercise. Shin splints of the lower leg are often from running up hills.
- Muscle Bruise from a direct blow. Bleeding into the quad (thigh muscles) is very painful.
- Bone Bruise from a direct blow (like on the hip). Called a "hip pointer."
- Skin Injury. Examples are a cut, scratch, scrape or bruise. All are common with leg injuries.
Pain Scale
- Mild: Your child feels pain and tells you about it. But, the pain does not keep your child from any normal activities. School, play and sleep are not changed.
- Moderate: The pain keeps your child from doing some normal activities. It may wake him or her up from sleep.
- Severe: The pain is very bad. It keeps your child from doing all normal activities.
When to Call for Leg Injury
Call 911 Now
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Self Care at Home
|
Call 911 Now
- Major bleeding that can't be stopped
- Serious injury with many broken bones
- Bone is sticking through the skin
- Looks like a dislocated joint (hip, knee or ankle)
- You think your child has a life-threatening emergency
Call Doctor or Seek Care Now
- Skin is split open or gaping and may need stitches
- Age less than 1 year old
- Severe pain and not better 2 hours after taking pain medicine
- Can't move hip, knee or ankle normally
- Knee injury with a "snap" or "pop" felt at the time of impact
- You think your child has a serious injury
- You think your child needs to be seen, and the problem is urgent
Call Doctor Within 24 Hours
- Has a limp when walking
- Very large bruise
- Large swelling is present
- Pain not better after 3 days
- You think your child needs to be seen, but the problem is not urgent
Call Doctor During Office Hours
- Injury limits sports or school work
- Dirty cut and no tetanus shot in more than 5 years
- Clean cut and no tetanus shot in more than 10 years
- Pain lasts more than 2 weeks
- You have other questions or concerns
Self Care at Home
- Bruised muscle or bone from direct blow
- Pain in muscle from minor pulled muscle
- Pain around joint from minor stretched ligament
- Minor cut or scrape
Care Advice for Minor Leg Injuries
-
What You Should Know About Minor Leg Injuries:
- During sports, muscles and bones get bruised.
- Muscles get stretched.
- These injuries can be treated at home.
- Here is some care advice that should help.
-
Pulled Muscle, Bruised Muscle or Bruised Bone Treatment:
- Pain Medicine. To help with the pain, give an acetaminophen product (such as Tylenol). Another choice is an ibuprofen product (such as Advil). Use as needed. Ibuprofen works better for this type of pain.
- Cold Pack. For pain or swelling, use a cold pack. You can also use ice wrapped in a wet cloth. Put it on the sore muscles for 20 minutes. Repeat 4 times on the first day, then as needed. Reason: Helps with the pain and helps stop any bleeding. Caution: Avoid frostbite.
- Heat Pack. If pain lasts over 2 days, put heat on the sore muscle. Use a heat pack, heating pad or warm wet washcloth. Do this for 10 minutes, then as needed. Caution: Avoid burns. For stiffness all over, use a hot bath instead. Move the sore leg muscles under the warm water.
- Rest. Rest the injured part as much as possible for 48 hours.
- Stretching. For pulled muscles, teach your youngster about stretching and strength training.
-
Mild Sprains (stretched ligaments) of Ankle or Knee Treatment:
- First Aid: Apply ice now to reduce bleeding, swelling, and pain. The more bleeding and swelling there is, the longer it will take to get better. Wrap with an elastic bandage.
- Treat with R.I.C.E. (rest, ice, compression, and elevation) for the first 24 to 48 hours.
- Apply compression with a snug, elastic bandage for 48 hours. Numbness, tingling, or increased pain means the bandage is too tight.
- Cold Pack: For pain or swelling, use a cold pack. You can also use ice wrapped in a wet cloth. Put it on the ankle or knee for 20 minutes. Repeat 4 times on the first day, then as needed. Reason: Helps with the pain and helps stop any bleeding. Caution: Avoid frostbite.
- To help with the pain, give an acetaminophen product (such as Tylenol). Another choice is an ibuprofen product (such as Advil). Use as needed. Continue for at least 48 hours.
- Keep the injured ankle or knee elevated and at rest for 24 hours.
- After 24 hours, allow any activity that doesn't cause pain.
-
Small Cut or Scrape Treatment
- Use direct pressure to stop any bleeding. Do this for 10 minutes or until the bleeding stops.
- Wash the wound with soap and water for 5 minutes. Try to rinse the cut under running water.
- Gently scrub out any dirt with a washcloth.
- Use an antibiotic ointment (such as Polysporin). No prescription is needed. Then, cover with a bandage. Change daily.
-
What to Expect:
- Pain and swelling usually peak on day 2 or 3.
- Most often, swelling is gone in 7 days.
- Pain may take 2 weeks to fully go away.
-
Call Your Doctor If:
- Pain becomes severe
- Pain is not better after 3 days
- Pain lasts more than 2 weeks
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.

This shows a sprained ankle. The ankle and foot are swollen because they were not wrapped with an elastic bandage right after the injury.
First Aid Care Advice for Ankle Sprain:
- Wrap with a snug elastic bandage.
- Apply an ice pack (crushed ice in a plastic bag covered with a towel) to reduce swelling and pain.

- Apply direct pressure to the entire wound with a sterile gauze dressing or a clean cloth. Once the bleeding has stopped, cover with an adhesive bandage or gauze.
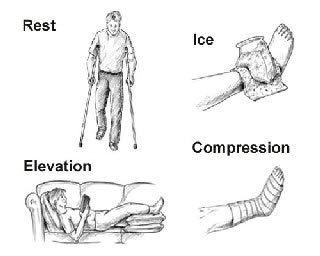
RICE is a way to remember the steps for taking care of a sprain, strain, or bruise. There are four things you should do:
- REST the injured part of your body for 24 hours. Can return to normal activity after 24 hours of rest if the activity does not cause severe pain.
- Apply a cold pack or an ICE bag (wrapped in a moist towel) to the area for 20 minutes. Repeat in 1 hour, then every 4 hours while awake.
- Apply COMPRESSION by wrapping the injured part with a snug, elastic bandage for 48 hours. If numbness, tingling, or increased pain occurs in the injured part, the bandage may be too tight. Loosen the bandage wrap.
- Keep the injured part of the body ELEVATED and at rest for 24 hours. For example, for an injured ankle, place that leg up on a pillow and stay off the feet as much as possible.

- Apply a cold pack or an ice bag (wrapped in a moist towel) to the area for 20 minutes. Repeat in 1 hour, then every 4 hours while awake.
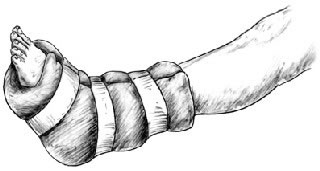
- Wrap a large soft pillow around ankle and foot. Reason: to support ankle and foot and keep bones from moving around.
- Use tape to hold the pillow in place.
Leg Pain
Is this your child's symptom?
- Pain in the legs (hip to foot)
- Includes hip, knee, ankle and toe joints
- Includes minor muscle strain from overuse
- Muscle cramps are also covered
- The pain is not caused by an injury
If NOT, try one of these:
Causes
- Main Causes. Muscle spasms (cramps) and strained muscles (overuse) account for most leg pain.
- Muscle Cramps. Brief pains (1 to 15 minutes) are often due to muscle spasms (cramps). Foot or calf muscles are especially prone to cramps that occur during sports. Foot or leg cramps may also awaken your child from sleep. Muscle cramps that occur during hard work or sports are called heat cramps. They often respond to extra fluids and salt.
- Muscle Overuse (Strained Muscles). Constant leg pains are often from hard work or sports. Examples are running or jumping too much. This type of pain can last several hours or up to 7 days. Muscle pain can also be from a forgotten injury that occurred the day before.
- Growing Pains. 10% of healthy children have harmless leg pains that come and go. These are often called growing pains (although they have nothing to do with growth). Growing pains usually occur in the calf or thigh muscles. They usually occur on both sides, not one side. They occur late in the day. Most likely, they are due to running or playing hard. They usually last 10 to 30 minutes.
- Low Calcium Level. Low calcium and vitamin D levels can cause minor bone pains. Pain is mainly in the legs and ribs. Children on a milk-free diet are at risk.
- Osgood Schlatter Disease. Pain, swelling and tenderness of the bone (tibia) just below the kneecap. The patellar tendon attaches to this bone. Caused by excessive jumping or running. Peak age is young teens. Harmless and goes away in 1 - 2 years.
- Viral Infections. Muscle aches in both legs are common with viral illness, especially influenza.
- Serious Causes. Fractures, deep vein thrombosis (blood clot in leg). Also, neuritis (a nerve infection) and arthritis (a joint infection).
- Septic Arthritis (Serious). A bacterial infection of any joint space is a medical emergency. The symptoms are severe joint pain, joint stiffness and a high fever.
- Toxic Synovitis of the hip is a harmless condition. It can imitate a septic arthritis of the hip. The symptoms are a limp, moderate pain and usually no fever. Toxic synovitis tends to occur in toddlers after jumping too much.
Pain Scale
- Mild: Your child feels pain and tells you about it. But, the pain does not keep your child from any normal activities. School, play and sleep are not changed.
- Moderate: The pain keeps your child from doing some normal activities. It may wake him or her up from sleep.
- Severe: The pain is very bad. It keeps your child from doing all normal activities.
When to Call for Leg Pain
Call 911 Now
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Self Care at Home
|
Call 911 Now
- Not moving or too weak to stand
- You think your child has a life-threatening emergency
Call Doctor or Seek Care Now
- Fever and pain in one leg only
- Can't move a hip, knee or ankle normally
- Swollen joint
- Calf pain on 1 side lasts more than 12 hours
- Numbness (loss of feeling) lasts more than 1 hour
- Severe pain or cries when leg is touched or moved
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Call Doctor Within 24 Hours
- Walking is not normal (has a limp)
- Fever and pain in both legs
- Bright red area on skin
- You think your child needs to be seen, but the problem is not urgent
Call Doctor During Office Hours
- Cause of leg pain is not clear
- Leg pain lasts more than 7 days
- Leg pains or muscle cramps are a frequent problem
- You have other questions or concerns
Self Care at Home
- Muscle cramps in the calf or foot
- Strained muscles caused by overuse (exercise or work)
- Growing pains suspected
- Cause is clear and harmless. (Examples are tight new shoes or a recent shot)
Care Advice for Leg Muscle Cramps, Strains, Growing Pains
-
What You Should Know About Leg Pain:
- Strained muscles are common after too much exercise or hard sports.
- Examples are hiking or running.
- Weekend warriors who are out of shape get the most muscle pains.
- Here is some care advice that should help.
-
Muscle Cramps Treatment:
- Muscle cramps in the feet or calf muscles occur in a third of children.
- Stretching. During attacks, stretch the painful muscle by pulling the foot and toes upward. Stretch as far as they will go to break the spasm. Stretch in the opposite direction to how it is being pulled by the cramp.
- Cold Pack. Use a cold pack. You can also use ice wrapped in a wet cloth. Put it on the sore muscle for 20 minutes.
- Water. Heat cramps can occur with hard sports on a hot day. If you suspect heat cramps, have your child drink lots of fluids. Water or sports drinks are good choices. Continue with stretching and using a cold pack.
- Prevention. Future attacks may be prevented by daily stretching exercises of the heel cords. Stand with the knees straight. Then, stretch the ankles by leaning forward against a wall. Place a pillow under the covers at the foot of the bed at night. This gives the feet more room to move at night. Also, be sure your child gets enough calcium in the diet. Daily vitamin D3 may also help.
-
Strained Muscles from Overuse - Treatment:
- Pain Medicine. To help with the pain, give an acetaminophen product (such as Tylenol). Another choice is an ibuprofen product (such as Advil). Use as needed.
- Cold Pack. For pain or swelling, use a cold pack. You can also use ice wrapped in a wet cloth. Put it on the sore muscles for 20 minutes. Repeat 4 times on the first day, then as needed. Caution: Avoid frostbite.
- Heat Pack. If pain lasts over 2 days, put heat on the sore muscle. Use a heat pack, heating pad or warm wet washcloth. Do this for 10 minutes, then as needed. Caution: Avoid burns. For stiffness all over, use a hot bath instead. Move the sore leg muscles under the warm water.
-
Growing Pains Treatment:
- Most often, the pains are mild and don't last long. No treatment is needed.
- Massage. Rub the sore muscles to help the pain go away.
- Pain Medicine. If the pain lasts more than 30 minutes, give a pain medicine. You can use either acetaminophen (such as Tylenol) or ibuprofen (such as Advil). Use as needed.
- Prevention. Research has shown that daily stretching can prevent most growing pains. Stretch the quads, hamstrings and calf muscles. Also, be sure your child gets enough calcium and vitamin D in their diet.
-
What to Expect:
- Muscle cramps usually last 5 to 30 minutes.
- Once they go away, the muscle returns to normal quickly.
- A strained muscle hurts for 3 to 7 days. The pain often peaks on day 2.
- Following severe overuse, the pain may last a week.
-
Call Your Doctor If:
- Muscle cramps occur often
- Fever, limp, or a swollen joint occurs
- Pain caused by work or sports lasts more than 7 days
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.
Lymph Nodes - Swollen
Is this your child's symptom?
- Increased size of one or more lymph nodes. Most are in the neck.
- Also, includes swollen lymph nodes in the armpit or groin
- It's larger than the same node on the other side of the body
- Normal nodes are usually less than ½ inch (12 mm) across. This is the size of a pea or baked bean.
If NOT, try one of these:
Causes of Swollen Lymph Nodes
- Neck Nodes. The cervical (neck) nodes are most commonly involved. This is because of the many respiratory infections that occur during childhood.
- Viral Throat Infection. This is the most common cause of swollen nodes in the neck. The swollen nodes are usually ½ to 1 inch (12 -25 mm) across. They are the same on each side.
- Bacterial Throat Infection. A swollen node with a bacterial throat infection is usually just on one side. It can be quite large; over 1 inch (25 mm) across. This is about the size of a quarter. Most often, it's the node that drains the tonsil.
- Tooth Decay or Abscess. This causes a swollen, tender node under the jawbone. Only one node is involved. The lower face may also be swollen on that side.
- Armpit Swollen Nodes. Causes include skin infections (such as impetigo). A rash (such as poison ivy) can do the same.
- Groin Swollen Nodes. Causes include skin infections (such as athlete's foot). A retained foreign object (such as a sliver) can be the cause.
- Shaving. Teen girls can cause low-grade infections when shaving the legs.
- Widespread Swollen Nodes. Swollen nodes everywhere suggest an infection spread in the blood. An example is infectious mono. Widespread rashes such as eczema can also cause all the nodes to enlarge.
- Normal Nodes. Lymph nodes can always be felt in the neck and groin. They are about the size of a bean. They never go away.
Lymph Nodes: What They Drain
- The lymph nodes are filled with white blood cells. They filter the lymph fluid coming from certain parts of the body. They fight infections.
- Neck Nodes in Front. These drain the nose, throat and lower face.
- Neck Nodes in Back. These drain the scalp.
- Armpit Nodes. These drain the arms and upper chest wall.
- Groin Nodes. These drain the legs and lower stomach wall.
Common Objects Used to Guess the Size
- Pea or pencil eraser: ¼ inch or 6 mm
- Dime: ¾ inch or 1.8 cm
- Quarter: 1 inch or 2.5 cm
- Golf ball: 1 ½ inches or 3.8 cm
- Tennis Ball: 2 ½ inches or 6.4 cm
When to Call for Lymph Nodes - Swollen
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Self Care at Home
|
Call Doctor or Seek Care Now
- Node in the neck causes trouble with breathing, swallowing or drinking
- Fever over 104° F (40° C)
- Skin over the node is red
- Node gets much bigger over 6 hours or less
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Call Doctor Within 24 Hours
- 1 or more inches (2.5 cm or more) in size by measurement
- Very tender to the touch
- Age less than 1 month old
- Node limits moving the neck, arm or leg
- Toothache with a swollen node under the jawbone
- Fever lasts more than 3 days
- You think your child needs to be seen, but the problem is not urgent
Call Doctor During Office Hours
- In the neck and also has a sore throat
- Large nodes at 2 or more parts of the body
- Cause of the swollen node is not clear
- Large node lasts more than 1 month
- You have other questions or concerns
Self Care at Home
- Mildly swollen lymph node
Care Advice for Small Lymph Nodes
-
What You Should Know About Normal Nodes:
- If you have found a pea-sized or bean-sized node, this is normal. Normal lymph nodes are smaller than ½ inch or 12 mm.
- Don't look for lymph nodes, because you can always find some. They are easy to find in the neck and groin.
-
What You Should Know About Swollen Nodes from a Viral Infection:
- Viral throat infections and colds can cause lymph nodes in the neck to get bigger. They may double in size. They may also become tender.
- This reaction is normal. It means the lymph node is fighting the infection and doing a good job.
- Here is some care advice that should help.
-
Pain Medicine:
- To help with the pain, give an acetaminophen product (such as Tylenol).
- Another choice is an ibuprofen product (such as Advil).
- Use as needed.
-
Fever Medicine:
- For fevers above 102° F (39° C), give an acetaminophen product (such as Tylenol).
- Another choice is an ibuprofen product (such as Advil).
- Note: Fevers less than 102° F (39° C) are important for fighting infections.
- For all fevers: Keep your child well hydrated. Give lots of cold fluids.
-
Do Not Squeeze:
- Don't squeeze lymph nodes.
- Reason: This may keep them from shrinking back to normal size.
-
Return to School:
- Swollen lymph nodes alone cannot be spread to others.
- If the swollen nodes are with a viral illness, your child can return to school. Wait until after the fever is gone. Your child should feel well enough to participate in normal activities.
-
What to Expect:
- After the infection is gone, the nodes slowly return to normal size.
- This may take 2 to 4 weeks.
- However, they won't ever completely go away.
-
Call Your Doctor If:
- Node gets 1 inch (2.5 cm) or larger in size
- Big node lasts more than 1 month
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.
Mental Health Problems
Is this your child's symptom?
- Mental health problems that often need urgent help
- Examples are anxiety attacks, depression, substance (drug) abuse and acting out
- Resources include hotlines, mental health experts and your child's doctor
Types of Serious Mental Health Problems
- Suicide thoughts, threats or attempts
- Homicide thoughts or threats
- Child abuse
- Drug or alcohol abuse
- Anxiety attacks or panic attacks
- Depression
Types of Non-Serious Behavior Problems
Many childhood behavior problems are common and not serious. Your child's doctor can often manage them. Pediatricians are often the first point of contact for these problems. Examples are:
- Temper tantrums
- Sleep problems
- Toilet training problems
- Eating problems
- Developmental delays
Behavior Scale: How to Judge Severity
- Mild Symptoms: Symptoms do not keep the child from any normal activities. School, play, relationships and sleep are not changed. Treatment: parenting groups or books.
- Moderate Symptoms: Symptoms keep the child from doing some normal activities. New behaviors mainly occur at home. They affect how the child and parent interact. They may also keep him or her from going to child care or school. Your child may not sleep well because of these symptoms. Treatment: Most often, brief counseling from a mental health provider or your child's doctor.
- Severe Symptoms: Symptoms keep the child from doing most normal activities. They affect the way the child acts with parents. Symptoms also impact relations with siblings and friends. Adults at child care or school may also be impacted by the child's actions. Treatment: These patients often need to be seen urgently by a mental health provider.
When to Call for Mental Health Problems
Call 911 Now
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Self Care at Home
|
Call 911 Now
- Physical harm or abuse is occurring now. Reason: police are needed.
- Child is threatening serious harm to others now. Reason: police are needed.
- Child has attempted or is threatening suicide now
Call Doctor or Seek Care Now
- Child abuse concerns and no physical findings. You can also call your local Child Protection Services.
- Needs mental health services and symptoms are urgent. You can also call a local mental health resource.
Call Doctor Within 24 Hours
- Substance abuse or alcohol abuse suspected, but no symptoms now
- Symptoms are constant and keep patient from doing their normal tasks of daily living
- Needs mental health services and symptoms are not urgent. You can also call a local mental health resource.
Call Doctor During Office Hours
- Common behavior problems (such as temper tantrums)
- Toilet training problems
- Sleep problems
- Eating problems
- School problems
- You have other questions or concerns
Self Care at Home
- Needs a resource or info on getting help for a mental health problem
Care Advice and Resources for Mental Health Problems
-
Threats of Harm to Self or Others - How to Respond:
- Children who threaten harm to self or other people need to be seen now. Emergent psych exams are done in the ER no matter the time of day.
- The risk assessment for suicide or homicide must be made in person. It should not be done by phone. It is usually made by a mental health expert. ER doctors may do the first screening.
- Some of these children may need to be in the hospital.
- If anyone is in danger, call the police (911). Examples are spouse abuse.
- For child abuse concerns, call the Child Protection Services (CPS) Hotline in your state.
-
Child or Teen Already In Treatment With A Mental Health Provider:
- Contact your mental health provider first.
- If can't reach your provider and problem is urgent, call another resource. See #3.
-
Local and National Mental Health Hotlines and Helplines (US numbers):
- Call your local mental health resource first, if you have the number. If not, call a national hotline for help. They often can refer you to the best local resource.
- National Suicide Prevention Lifeline: 1-888-784-2433
- Domestic Violence Hotline: 1-800-799-7233
- Child Abuse Hotline: 1-800-422-4453. Crisis counselors answer calls 24//7.
- Substance Abuse Hotline: 1-800-662-4357. This is a 24/7 substance abuse and mental health referral line. They can give you local treatment choices and numbers for support groups.
- Mental Health Helpline: 1-800-950-6264. This is an information and referral source for finding local mental health programs.
- Postpartum Depression Helpline: 1-800-944-4773
- National Poison Control Number: 1-800-222-1222
-
Website Resources for Mental Health Concerns:
- American Academy of Pediatrics parenting website: www.healthychildren.org.
- American Academy of Child and Adolescent Psychiatry: Talking to Children about Disasters.
-
Call Your Doctor If:
- You think your child needs to be seen
- Your child becomes worse
- You have other questions or concerns
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.
Molluscum
Is this your child's symptom?
- Small raised growths that have a smooth, waxy surface
- The medical name is molluscum contagiosum
- Viral infection of the skin
- A doctor has told you your child has molluscum or
- Your child has had close contact with another person who has it
Symptoms of Molluscum
- Small bumps with a waxy or pearl-colored, smooth surface
- May have a dimple (indent) in center
- Bumps are firm with a core of white material.
- Are many different sizes, from pinhead to ¼ inch (3 to 6 mm) across
- Can occur anywhere on the body, but usually stay in just one area
- Are sometimes itchy, but not painful
- Usually age 2 to 12 years
- Most infected children get 5 to 10 of them
Cause of Molluscum
- They are caused by a poxvirus. This is a different virus than the one that causes warts.
- Friction or picking at them causes them to increase in number.
To Treat or Not to Treat?
- Some doctors advise not treating them if there are only a few. Reason: They are harmless and painless.
- They have a natural tendency to heal and go away on their own.
When Special Treatment is Considered
- Your child picks at them
- They are in areas of friction (for example, the armpit)
- They are spreading quickly or
- You feel they are a cosmetic problem
Prevent Spread to Others
- Avoid baths or hot tubs with other children. Reason: Can spread in warm water.
- Also, avoid sharing washcloths or towels.
- Contact sports: Can spread to other team members. They should be covered or treated.
- Time it takes to get them: 4 to 8 weeks after close contact.
When to Call for Molluscum
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Self Care at Home
|
Call Doctor or Seek Care Now
- Redness or red streak spreading from molluscum with fever
- Your child looks or acts very sick
Call Doctor Within 24 Hours
- Redness or red streak spreading from molluscum without fever
- You think your child needs to be seen
Call Doctor During Office Hours
- Molluscum on the face
- 4 or more molluscum
- Your child can't stop picking at the molluscum
- Pus is draining from the molluscum (Apply antibiotic ointment 3 times per day until seen)
- On treatment more than 2 weeks and new molluscum appear
- On treatment more than 12 weeks and molluscum not gone
- You have other questions or concerns
Self Care at Home
- Molluscum: 3 or less
Care Advice for Molluscum
-
What You Should Know About Molluscum:
- They are harmless and painless.
- Wart-removing acids are not helpful.
- Duct tape treatment will make them go away faster.
- Here is some care advice that should help.
-
Duct Tape - Cover the Molluscum:
- Covering them with duct tape can irritate them. This turns on the body's immune system.
- Cover as many of them as possible. (Cover at least 3 of them.)
- The covered ones become red and start to die. When this happens, often all of them will go away.
- Try to keep them covered all the time.
- Remove the tape once per day, usually before bathing. Then replace it after bathing.
- Some children don't like the tape on at school. At the very least, tape it every night.
-
Prevent the Spread to Other Areas of Your Child's Body:
- Discourage your child from picking at them.
- Picking it and scratching a new area with the same finger can spread them. A new one can form in 1 to 2 months.
- Chewing or sucking on them can lead to similar bumps on the face.
- If your child is doing this, cover them. You can use a bandage (such as Band-Aid).
- Keep your child's fingernails cut short and wash your child's hands more often.
-
What to Expect:
- Without treatment, they go away in 6 to 18 months.
- If covered with duct tape, they may go away in 2 or 3 months.
- If picked at often, they can become infected with bacteria. If this happens, they change into crusty sores (impetigo).
-
Return to School:
- Your child doesn't have to miss any child care or school.
- There is a mild risk of spread to others.
-
Call Your Doctor If:
- Your child continues to pick at them
- New ones develop after 2 weeks of treatment
- They are still present after 12 weeks of treatment
- You think your child needs to be seen
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.

This shows an infection from the molluscum contagiosum virus. Molluscum is sometimes called a "water wart." The growths are pink, white or pearly-colored. They are firm, small and raised with a dimple in the middle.

This shows an eye with an infection from the molluscum contagiosum virus. The growths are pink, white or pearly-colored. They are firm, small and raised with a dimple in the middle.

This shows an infection from the molluscum contagiosum virus. Molluscum is sometimes called a "water wart." The growths are pink, white or pearly-colored. They are firm, small and raised with a dimple in the middle.
Mosquito Bite
Is this your child's symptom?
- Bites from a mosquito
- Cause itchy, red bumps
- Often they look like a hive
- West Nile Virus (WNV) questions are also covered
If NOT, try one of these:
Types of Reactions to Mosquito Bites
- Red Bumps. In North America, mosquito bites are mainly an annoyance. They cause itchy red skin bumps. Often, the bite looks like hives (either one large one or several small ones).
- When a mosquito bites, its secretions are injected into the skin. The red bumps are the body's reaction to this process.
- Suspect mosquito bites if there are bites on other parts of the body. Most bites occur on exposed parts such as face and arms.
- Swelling. Bites of the upper face can cause severe swelling around the eye. This can last for several days. With bites, the swelling can be pink as well as large (especially age 1-5 years).
- Disease. Rarely, the mosquito can carry a serious blood-borne disease. In the US and Canada, this is mainly West Nile Virus (WNV). In Africa and South America, they also carry malaria and yellow fever.
- Prevention. Insect repellents can prevent mosquito bites. Use DEET (applied to skin) and permethrin (applied to clothing).
Cause of Mosquito Bite Reaction
- The skin bumps are the body's reaction to the mosquito's saliva.
- While it's sucking blood, some of its secretions get mixed in.
Mosquito Life Cycle
- Only female mosquitoes bite. They need a blood meal to produce eggs. The female may bite 20 times before she finds a small blood vessel. She then sips blood for 90 seconds.
- Males eat flower nectar and plant juices.
- 170 species of mosquito are in North America.
- At a far distance, they are attracted by smell (breath odors, sweat and perfumes). They can smell up to 120 feet (36 meters). At a close distance, they are attracted by body heat and movement.
Risk Factors for Increased Mosquito Bites
- Warmer body temperature
- Male more than female
- Children more than adults
- Breath odors
- Sweating
- Perfumed soaps and shampoos
Complications of Insect Bites
- Impetigo. A local bacterial infection. Gives sores, soft scabs and pus. Caused by scratching or picking at the bites. More common in itchy bites.
- Cellulitis. The bacterial infection spreads into the skin. Gives redness spreading out from the bite. The red area is painful to the touch.
- Lymphangitis. The bacterial infection spreads up the lymph channels. Gives a red line that goes up the arm or leg. More serious because the infection can get into the bloodstream. (This is called sepsis.)
When to Call for Mosquito Bite
Call 911 Now
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Self Care at Home
|
Call 911 Now
- Life-threatening allergic reaction suspected. Symptoms include sudden onset of trouble breathing or swallowing.
- Can't wake up
- You think your child has a life-threatening emergency
Call Doctor or Seek Care Now
- Spreading red area or streak with fever
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Call Doctor Within 24 Hours
- Painful spreading redness started more than 24 hours after the bite. Note: any redness starting in the first 24 hours is a reaction to the bite.
- More than 48 hours since the bite and redness gets larger
- Unexplained fever and recent travel outside the country to high risk area
- You think your child needs to be seen, but the problem is not urgent
Call Doctor During Office Hours
- Pregnant and recently traveled to or lives in a place with a Zika outbreak
- Scab that looks infected (drains pus or gets bigger) not better with antibiotic ointment
- Severe itching not better after 24 hours of using steroid cream
- You have other questions or concerns
Self Care at Home
- Normal mosquito bite
- Questions about West Nile Virus
- Questions about insect repellents (such as DEET)
Care Advice
Treatment for Mosquito Bites
-
What You Should Know About Mosquito Bites:
- In the United States and Canada, mosquito bites rarely carry any disease.
- They cause itchy red skin bumps.
- Most of the time, the bumps are less than ½ inch (12 mm) in size. In young children, they can be larger.
- Some even have a small water blister in the center.
- A large hive at the bite does not mean your child has an allergy.
- The redness does not mean the bite is infected.
- Here is some care advice that should help.
-
Steroid Cream for Itching:
- To reduce the itching, use 1% hydrocortisone cream (such as Cortaid). No prescription is needed. Put it on 3 times a day until the itch is gone. If you don't have, use a baking soda paste until you can get some.
- If neither is available, use ice in a wet washcloth for 20 minutes.
- Also, you can put firm, sharp, direct, steady pressure on the bite. Do this for 10 seconds to reduce the itch. A fingernail, pen cap, or other object can be used.
-
Allergy Medicine for Itching:
- If the bite is still itchy, try an allergy medicine (such as Benadryl). No prescription is needed.
- Sometimes it helps, especially in allergic children.
-
Try Not to Scratch:
- Cut the fingernails short.
- Help your child not to scratch.
- Reason: Prevent a skin infection at the bite site.
-
Antibiotic Ointment:
- If the bite has a scab and looks infected, use an antibiotic ointment. An example is Polysporin.
- No prescription is needed. Use 3 times per day. (Note: Usually infection caused by scratching bites with dirty fingers).
- Cover the scab with a bandage (such as Band-Aid). This will help prevent scratching and spread.
- Wash the sore and use the antibiotic ointment 3 times per day. Do this until healed.
-
What to Expect:
- Most mosquito bites itch for 3 or 4 days.
- Any pinkness or redness lasts 3 or 4 days.
- The swelling may last 7 days.
- Bites of the upper face can cause severe swelling around the eye. This does not hurt the vision and is harmless.
- The swelling is often worse in the morning after lying down all night. It will improve after standing for a few hours.
-
Call Your Doctor If:
- Bite looks infected (redness gets larger after 48 hours)
- Bite becomes painful
- You think your child needs to be seen
- Your child becomes worse
West Nile Virus Questions
-
West Nile Virus (WNV) - What You Should Know:
- WNV is a disease carried by mosquitoes. It can be spread to humans through a mosquito bite.
- About 1% of mosquitoes carry WNV.
- Of people who get WNV, less than 1% get the serious kind.
- Here are some facts that should help.
-
Symptoms of WNV:
- No symptoms: 80% of WNV infections.
- Mild symptoms: 20% of infections. Symptoms include fever, headache, and body aches. Some have a skin rash. These symptoms last 3-6 days. They go away without any treatment. This is called WNV fever.
- Serious symptoms: less than 1% (1 out of 150) of WNV infections. Symptoms are high fever, stiff neck, confusion, coma, seizures, and muscle weakness. The muscle weakness is often just on one side. The cause is infection of the brain (encephalitis) or spinal cord (viral meningitis).
- Death: 10% of those who need to be in the hospital.
- Child cases are most often mild. Most serious cases occur in people over age 60.
-
Diagnosis of WNV:
- Mild symptom cases do not need to see a doctor. They do not need any special tests.
- Severe symptom cases (with encephalitis or viral meningitis) need to see a doctor right away. Special tests on the blood and spinal fluid will be done to confirm WNV.
- Pregnant or nursing women need to see a doctor if they have WNV symptoms.
-
Treatment of WNV:
- No special treatment is needed after a mosquito bite.
- There is no special treatment or anti-viral drug for WNV symptoms.
- People with serious symptoms often need to be in the hospital. They will be given IV fluids and airway support.
- There is not yet a vaccine to prevent WNV in humans.
-
WNV - Spread by Mosquitoes:
- WNV is spread by the bite of a mosquito. The mosquito gets the virus from biting infected birds.
- Even in an area where WNV occurs, less than 1% of mosquitoes carry the virus.
- Spread is mosquito-to-human.
- Person-to-person spread does not occur. Kissing, touching, or sharing a glass with a person who has WNV is safe.
- Mothers with mosquito bites can breastfeed (CDC 2003), unless they get symptoms of WNV.
- It takes 3-14 days after the mosquito bite to get WNV.
- In United States and Canada, the peak summers for WNV were 2002, 2003 and 2012.
Insect Repellent Questions
-
Prevention Tips:
- Wear long pants, a long-sleeved shirt and a hat.
- Avoid being outside when the bugs are most active. Mosquitoes are most active at dawn and dusk. Limit your child's outdoor play during these times.
- Get rid of any standing water. (Reason: It's where they lay their eggs.)
- Keep bugs out of your home by fixing any broken screens.
- Insect repellents containing DEET are very good at preventing mosquito bites. Read the label carefully.
-
DEET Products - Use on the Skin:
- DEET is a good mosquito repellent. It also repels ticks and other bugs.
- The AAP approves DEET use over 2 months old. Use 30% DEET or less. Use 30% DEET if you need 6 hours of protection. Use 10% DEET if you only need protection for 2 hours.
- Don't put DEET on the hands if your child sucks their thumb or fingers. (Reason: Prevent swallowing DEET)
- Warn older children who apply their own DEET to use less. A total of 3 or 4 drops can protect the whole body.
- Put on exposed areas of skin. Do not use near eyes or mouth. Don't use on skin that is covered by clothing. Don't put DEET on sunburns or rashes. (Reason: DEET can be easily absorbed in these areas.)
- Wash it off with soap and water when your child comes indoors.
- Caution: DEET can damage clothing made of man-made fibers. It can also damage plastics (eye glasses) and leather. DEET can be used on cotton clothing.
-
Permethrin Product - Use on Clothing:
- Products that contain permethrin (such as Duranon) work well to repel mosquitos and ticks.
- Unlike DEET, these products are put on clothing instead of on the skin.
- Put it on shirt cuffs, pant cuffs, shoes and hats. Can also put it on mosquito nets and sleeping bags.
- Do not put permethrin on the skin. (Reason: Sweat changes it so it does not work).
-
Picaridin Products:
- Picaridin is a repellent that is equal to 10% DEET.
- It can safely be put on skin or clothing.
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.
Mosquito-Borne Diseases from Travel
Is this your child's symptom?
- Tropical diseases spread by mosquitoes
- Includes malaria, yellow fever, dengue fever, chikungunya fever and Zika virus
- Your child has no symptoms of tropical disease. If your child has symptoms, use other guides. These diseases start with high fevers.
- Tropical diseases occur in people who travel to or live in high-risk countries. These mainly are developing countries near the Equator. You may have traveled to a high-risk country recently.
- West Nile Virus is not included in this guide. See the Mosquito Bite guide.
If NOT, try one of these:
How Tropical Mosquito-Borne Diseases are Detected by this Symptom Checker
- These diseases can't be diagnosed over the phone. But, they can be suspected based on their symptoms. They are then referred to a medical setting where a diagnosis can be made.
- Malaria will be picked up by the Fever guide. High fevers, prolonged fever and shaking chills will refer the child to be seen. The Headache or Leg Pain guides will also work. Reason: Malaria can also cause severe headache or muscle pain.
- Yellow fever will be picked up by the Fever guide. High fevers, prolonged fever and shaking chills will refer the child to be seen. The Headache or Leg Pain guides will also work. Reason: Yellow fever can also cause severe headache or muscle pains.
- Dengue fever will be picked up by the Fever guide. High fevers, prolonged fever and shaking chills will refer the child to be seen. The Headache or Leg Pain guides will also work. Reason: Dengue fever can also cause severe headache, joint pain or muscle pains.
- Chikungunya fever will be picked up by the Fever guide. High fevers, prolonged fever and shaking chills will refer the child to be seen. The Arm Pain or Leg Pain guides will also work. Reason: Joint pains in the hands and feet are common. So are muscle pains.
- Zika virus infection will be picked up by the Fever or Rash care guides.
- Travel to a high risk country should raise the concern. However, common diseases that cause fever (such as colds) also must be ruled out. They occur more commonly in these countries than the serious diseases. But, severe symptoms or symptoms that last too long make us think about these other diseases.
World-wide Causes of Death in Children Under Age 5
- 6.3 million children under the age of 5 died in 2013 worldwide.
- These 5 infections account for over 50% of all early child deaths:
- Pneumonia and other respiratory diseases 19%
- Diarrhea disease 18%
- Malaria 8%
- Measles 4%
- HIV/AIDS 3%
- Poor nutrition is a factor in over half who die older than one month of age.
- Over 80% of deaths occur in Africa and Southern Asia. India accounts for 21% of under-five deaths.
- More than half are due to diseases that we could prevent or treat.
- Resource: WHO report, September 2014
Tropical Countries
- Countries in the tropics are near the Equator. They have hot and humid climates.
- The tropics are also defined as regions without a cold season.
- Many diseases in these countries are spread by an insect bite.
- In the tropics, insects never hibernate. They are present in large numbers year round.
- Other diseases here are spread by germs that multiply in warm water. The water in the tropics usually stays warm.
- Tropical diseases occur in people who live in or travel to high-risk countries.
- Climate change is a factor that has allowed these diseases to spread.
Preventing Mosquito Bites During Travel
- Wear long pants, a long-sleeved short and a hat.
- Avoid being outside when the bugs are most active. Mosquitoes are most active at dawn and dusk. Limit your child's outdoor play at these times. The mosquito that transmits Zika is also active during the day.
- Get rid of any standing water. Reason: it's where mosquitoes lay their eggs.
- Keep bugs out of the home by fixing any broken screens.
- If exposed to outside air, use bed nets to protect you during sleep.
- To prevent mosquito bites, use insect repellents that have DEET. These products work well to protect you from bites. Read the label before using.
Preventing Bites - Use DEET on Skin and Permethrin on Clothing
- DEET is a good mosquito repellent. It also repels ticks and other bugs.
- The AAP approves DEET use for children more than 2 months old. Use 30% DEET or less. Use 30% DEET if you need 6 hours of protection. Use 10% DEET if you only need protection for 2 hours.
- Don't put DEET on the hands if your child sucks their thumb or fingers. Reason: prevent DEET from being swallowed.
- Warn older children who apply their own DEET to use less. A total of 3 or 4 drops can protect the whole body.
- Put on exposed areas of skin. Do not use near eyes or mouth. Don't use on skin that is covered by clothing. Don't put DEET on sunburns or rashes. Reason: DEET can be easily absorbed in these areas.
- Wash it off with soap and water when your child comes indoors.
- Caution: DEET can harm clothing made of man-made fibers. It can also harm plastics (eye glasses) and leather. DEET can be used on cotton clothing.
- Permethrin products can be applied to all types of clothing.
- See Mosquito Bite care guide for more info on how to prevent bites.
When to Call for Mosquito-Borne Diseases from Travel
Call 911 Now
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Self Care at Home
|
Call 911 Now
- You think your child has a life-threatening emergency
Call Doctor or Seek Care Now
- Tropical disease suspected and fever present
- Tropical disease has been diagnosed and getting worse
- Tropical disease has been diagnosed and fever returns after gone for several days
- Tropical disease has been diagnosed and shaking chills return
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Call Doctor Within 24 Hours
- Tropical disease suspected, but no fever
- You think your child needs to be seen, but the problem is not urgent
Call Doctor During Office Hours
- Pregnant and recently traveled to or lives in a place with a Zika outbreak
- You have other questions or concerns
Self Care at Home
- Questions about malaria
- Questions about yellow fever
- Questions about dengue fever
- Questions about Chikungunya fever
- Questions about Zika virus
Care Advice
Malaria Questions
-
What You Should Know About Malaria:
- It is a parasite disease spread by the bite of mosquitoes. The parasites enter red blood cells and destroy them.
- World Impact: There are over 200 million new cases per year. It is a leading cause of death in the world. In Africa, one child dies every minute from it. It causes almost 1 million deaths per year.
-
Symptoms:
- Bouts of high fever occur every 2 to 3 days.
- Shaking chills come before the fever.
- The fever is followed by profuse sweating.
- Severe headache, muscle pains and feeling very tired is common.
- Sometimes, jaundice (yellow skin) occurs.
-
Cause:
- Malaria is caused by a tiny parasite (protozoan) carried by some mosquitoes.
- Spread is mosquito to human.
- The disease is carried by an infected mosquito. The mosquito becomes infected when it bites a human infected with malaria. The parasite is then passed on to healthy humans in the spit from a bite. It then enters the person's red blood cells.
-
Time Period to Get Sick:
- The time from the bite to symptoms is 5-15 days.
-
Contagious Period:
- Person to person spread of the illness does not occur.
- Kissing or sharing a glass with a person who has malaria is safe.
-
Tests and Treatment:
- Blood smears and other blood tests are done to diagnose it.
- It is treated with anti-malaria drugs.
- For severe symptoms, patients will need care in a hospital.
-
What to Expect:
- Patients have good outcomes if treated early.
- Deaths are highest in infants: up to 3%.
-
How to Prevent:
- Use insect repellents (such as DEET).
- Bed nets can help protect you at night during sleep.
- Malaria drugs are often prescribed before travel to a high risk zone.
- There is no vaccine to prevent it.
-
Countries with Malaria:
- It occurs in Africa, lower Asia, Central and South America. Over 90% of cases occur in Africa.
- It does not occur in the US except in travelers coming back. This results in about 1500 US cases per year.
- For more info and for current high-risk countries, see the CDC website: Malaria.
-
Call Your Doctor If:
- You have other questions or concerns
Yellow Fever Questions
-
What You Should Know About Yellow Fever:
- It is viral disease spread by the bite of mosquitoes. The virus attacks the liver and kidneys.
- World Impact: Africa has 200,000 new cases each year. There are over 30,000 deaths each year. Now, it is rare in travelers because of the yellow fever vaccine.
-
Symptoms:
- High fevers with shaking chills occur.
- Other symptoms are severe headache, backache and muscle pains.
- Jaundice (yellow skin) is common. Hence, the name yellow fever.
- If the disease progresses, bleeding from the skin, nose, gums and gut will occur.
-
Cause:
- Spread is mosquito to human.
- The virus is carried by an infected mosquito. The mosquito becomes infected when it bites a human infected with yellow fever. The virus is passed on to healthy humans in spit from a bite.
-
Time Period to Get Sick:
- The time from the bite to symptoms is 3-6 days.
-
Contagious Period:
- Person to person spread of the illness does not occur.
- Kissing or sharing a glass with a person who has yellow fever is safe.
-
Tests and Treatment:
- Blood tests are needed to diagnose it.
- Patients need care in a hospital.
- There are no anti-viral drugs for treating it.
-
What to Expect:
- The death rate in people with complications can be high.
-
How to Prevent:
- Vaccine: There is a yellow fever vaccine to prevent the illness.
- Use insect repellents (such as DEET).
- Bed nets can help protect you at night during sleep.
-
Countries with Yellow Fever:
- Mostly occurs in Africa.
- Less common in South America (100 cases per year). Reason: Wide use of the vaccine.
- It does not occur in the US except in travelers coming back.
- For more info and for current high-risk countries, see the CDC website: Yellow Fever.
-
Call Your Doctor If:
- You have other questions or concerns
Dengue Fever Questions
-
What You Should Know About Dengue Fever:
- It is a viral disease spread by the bite of an infected mosquito.
- World Impact: 90 million new infections each year in the world. It causes 20,000 deaths per year.
-
Symptoms:
- High fever with shaking chills occurs.
- Patients can also have severe headache, eye pain, joint pain and muscle pains.
- Bone pain can be severe.
- A widespread pink rash is common.
- If the disease progresses, bleeding from the skin, nose, gums and gut can occur.
-
Cause:
- Spread is mosquito to human.
- The virus is carried by an infected mosquito. The mosquito becomes infected when it bites a human infected with dengue. The virus is passed on to healthy humans in spit from a bite.
-
Time Period to Get Sick:
- The time from the bite to symptoms is usually 3-7 days. Sometimes, it can be up to 14 days.
-
Contagious Period:
- Person to person spread of the illness does not occur.
- Kissing or sharing a glass with a person who has dengue is safe.
-
Tests and Treatment:
- Blood tests are needed for people with severe disease.
- Treatment consists of rest and lots of fluids.
- For severe symptoms, patients need care in a hospital.
- There are no anti-viral drugs for treating it.
-
What to Expect:
- Fever lasts up to 7 days.
- Symptoms last up to 2 weeks.
- Most people recover fully.
- If bleeding occurs, the death rate can be 1%.
-
How to Prevent:
- Use insect repellents (such as DEET).
- Bed nets can help protect you at night during sleep.
- There is no vaccine to prevent it.
-
Countries with Dengue Fever:
- It occurs in Asia, Africa, South America and the Caribbean islands.
- It does not occur in the US except in travelers coming back. A few cases have occurred in Florida and Texas.
- For more info and for current high-risk countries, see the CDC website: Dengue.
-
Call Your Doctor If:
- You have other questions or concerns
Chikungunya Fever Questions
-
What You Should Know About Chikungunya Fever:
- It is a viral disease spread by the bite of an infected mosquito.
- World Impact: It is a common disease, but rarely any deaths.
-
Symptoms:
- Most common symptoms are fever and joint pain.
- The joint pain starts in the hands and feet.
- This can progress to swollen joints.
- Other symptoms are headache and muscle pains.
- A widespread pink rash may occur.
-
Cause:
- Spread is mosquito to human.
- The virus is carried by an infected mosquito. The mosquito becomes infected when it bites a human infected with Chikungunya. The virus is passed on to healthy humans in spit from a bite.
-
Time Period to Get Sick:
- The time from the bite to symptoms is 3-7 days.
-
Contagious Period:
- Person to person spread of the illness does not occur.
- Kissing or sharing a glass with a person who has chikungunya is safe.
-
Tests and Treatment:
- Blood tests are done for people with severe disease.
- Treatment is mainly rest and lots of fluids.
- Medicines are given for pain and fever.
- For severe symptoms, patients will need care in a hospital.
- There are no anti-viral drugs for treating it.
-
What to Expect:
- Most symptoms are gone within a week.
- In some people, the joint pain can last for months.
- Deaths are very rare.
-
How to Prevent:
- Use insect repellents (such as DEET).
- Bed nets can help protect you at night during sleep.
- There is no vaccine to prevent it.
-
Countries with Chikungunya:
- It is common in Africa and Asia.
- In 2013, the disease was first reported in the Caribbean islands.
- It then spread to Central and South America.
- Does not occur in the US except in travelers coming back.
- No signs of the disease yet in US mosquitoes.
- For more info and current high-risk countries, see the CDC website: Chikungunya Virus.
-
Call Your Doctor If:
- You have other questions or concerns
Zika Virus Questions
-
What You Should Know About Zika Virus:
- Zika is a viral disease spread by the bite of mosquitoes.
- A major outbreak was reported in Brazil in May 2015. It then spread through the Americas and the Caribbean.
-
Zika Virus Symptoms:
- 80% of infections have no clinical symptoms.
- Mild illness: 20% of infections. Symptoms include fever, pink rash, joint pains, headache, body aches and red eyes. These symptoms last 3 to 6 days and go away without any treatment. Severe symptoms are not common.
-
Birth Defects and Zika Virus:
- A pregnant woman who gets a Zika infection can pass the virus to her baby. The baby may develop a severe birth defect called microcephaly. It causes babies to be born with a small head and brain damage. Eye defects have also been reported.
- The risk of microcephaly is 1-5% depending on the time of pregnancy. The first 3 months of pregnancy carries the greatest risk of causing this birth defect.
- Pregnant women who get Zika within 2 weeks of delivery can pass it to the newborn. The newborn will be ill, but not have birth defects.
- Babies who get Zika from a bite have the same mild symptoms as others. They cannot develop microcephaly after they are born.
-
Cause:
- Spread is usually from mosquito to human.
- The virus is carried by an infected mosquito. The mosquito becomes infected when it bites a human infected with Zika. The virus is passed on to healthy humans in spit from a bite.
- Pregnant women can pass the virus to their baby.
- Breastfeeding: it is not passed in breastmilk. Continue to breastfeed (CDC).
- Sexual intercourse: it can be transmitted through sex. If their partner is pregnant, males who have been in high-risk areas should use condoms. Use these until the baby is delivered. If a man or woman travels to a Zika risk area, use condoms. Avoid pregnancy for 8 weeks.
-
Time Period to Get Sick:
- The time from the bite to symptoms is 3 days to 2 weeks.
-
Tests and Treatment:
- Blood tests are needed to diagnose Zika virus.
- When do you need to get a blood test? Any pregnant woman who has recently traveled to or lives in a high-risk area for Zika virus. See CDC website. Blood tests are mainly available at CDC and some state public health labs. If you need a blood test, talk to your obstetrician (OB doctor).
- There are no anti-viral drugs for treating it. Treat the symptoms with increased fluids and pain medicine.
-
What to Expect:
- If symptoms occur, they usually last less than 1 week.
-
How to Prevent:
- Use insect repellents such as DEET.
- Bed nets can help protect you at night during sleep.
- There is no vaccine to prevent it.
-
Countries with Zika Virus:
- Current outbreak South America, Central America, Mexico and the Caribbean. Also in isolated areas of Africa and Asia.
- Until July 2016, mosquito transfer of Zika virus in the US did not occur. The disease only occurred in travelers coming back into the US. In 2016, there were more than 4,000 US cases associated with travel to high-risk countries.
- In August 2016, a small outbreak transmitted by local mosquitoes began in Florida. Predictions are that it will eventually occur in several southern US states.
- For up-to-date information and current high-risk areas, see the CDC website: Zika Virus.
-
Call Your Doctor If:
- You have other questions or concerns
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.
Motion Sickness
Is this your child's symptom?
- Dizziness or nausea from spinning or rolling motions
Symptoms of Motion Sickness
- Dizziness and unsteady walking
- Nausea and vomiting are also common
- Before age 6, the main symptom is dizziness and the need to lie down.
- After age 12, the main symptom is nausea (feeling sick to the stomach).
Causes of Motion Sickness
- Symptoms are mainly triggered by motion. Sea sickness or amusement park sickness are the most common types. Fun-park rides that spin or whirl are some of the main causes. The Tilt-a-whirl is a good example of a ride to avoid. Also seen during travel by train, aircraft and even car.
- The cause is a sensitive center in the inner ear. This center helps to maintain balance.
- As a car passenger driving on winding roads, 25% of people will have symptoms. Under extreme conditions (e.g., high seas) over 90% of people have symptoms.
- Strongly genetic: If one parent has it, 50% of the children will have it.
- It is not related to emotional problems. The child cannot control it with will power.
- Motion sickness symptoms are often worse in children.
When to Call for Motion Sickness
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Self Care at Home
|
Call Doctor or Seek Care Now
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Call Doctor Within 24 Hours
- Motion sickness symptoms last more than 8 hours
- You think your child needs to be seen, but the problem is not urgent
Call Doctor During Office Hours
- You have other questions or concerns
Self Care at Home
- Motion sickness symptoms
Care Advice for Motion Sickness
-
What You Should Know About Motion Sickness:
- Motion sickness is a common normal reaction that occurs in 25% of people.
- Caused by increased sensitivity of the inner ear.
- It is not related to emotional problems or any physical disease.
- In the future, take a special medicine ahead of time to prevent it.
- Here is some care advice that should help.
-
Rest - Lie Down:
- Have your child lie down and rest. If your child goes to sleep, all the better.
-
Fluids - Offer Sips:
- Give only sips of clear fluids. Water is best. Do this until the stomach settles down.
-
Vomiting:
- Prepare for vomiting. Keep a vomiting pan handy.
- Usually, children don't vomit more than once with motion sickness.
-
What to Expect:
- All symptoms of motion sickness usually go away in 4 hours after stopping the motion.
- As for the future, people usually don't outgrow motion sickness. Sometimes, it becomes less severe in adults.
-
Motion Sickness Medicine - Dramamine:
- Buy some dimenhydrinate tablets (such as Dramamine) at your drug store. No prescription is needed. In the future, give it to prevent motion sickness.
- It comes in 50 mg regular and chewable tablets or in 25 mg Kids chewable tablets.
- Dosage by age: do not use under age 2.
- 2 to 5 years (12.5 mg): ½ Kids chewable
- 6 to 11 years (25 mg): 1 Kids chewable
- 12 and older (50 mg): 1 regular tablet or chewable
- Give the medicine 1 hour before traveling or going to a fun-park.
- The tablets give 6 hours of protection and are very helpful.
- Benadryl can also be used to prevent motion sickness. Use this if you do not have any Dramamine.
-
Prevention Tips for Car Trips:
- If your child is over 12 years old, sit him in the front seat.
- Before age 12, have your child sit in the middle back seat. This should help him look out the front window.
- Have your child look out the front window, not the side one.
- Discourage looking at books or movies during car travel.
- Keep a window cracked to provide fresh air.
- Avoid exhaust fumes from other vehicles.
- Meals: Have your child eat light meals before trips. Some children can just tolerate crackers and water.
- Plastic Bags: Always carry a ziplock plastic bag for vomiting emergencies.
-
Wrist Bands - Prevention:
- Acupressure bands (such as Sea-Bands) are helpful for some adults.
- There is no reason they shouldn't work for some children.
- Put them on before car trips or other causes of motion sickness.
- The pressure button goes over the center of the wrist. Place ½ inch (1 cm) above the wrist crease.
-
Call Your Doctor If:
- Any symptoms last over 8 hours
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.
Mouth Injury
Is this your child's symptom?
- Injuries to the lips and mouth
- Includes inner cheeks and the roof of the mouth (hard and soft palate)
- Front of the mouth includes the tongue. Also, includes the flap under the upper lip (frenulum).
- Back of the mouth includes the tonsils and the throat
- Tooth injuries are not covered here
If NOT, try one of these:
Types of Mouth Injuries
- Tongue. Cuts of the tongue or inside of the cheeks are the most common mouth injury. Usually, due to accidentally biting them during eating. Bites of the tongue rarely need sutures. Even if they gape open a little, the cuts usually heal quickly. If the edges come together when the tongue is still, it needs no treatment.
- Upper Lip. Cuts and bruises of the upper lip are usually due to falls. The piece of tissue joining the upper lip to the gum is the frenulum. A tear of the upper frenulum is very common. It always heals without sutures. However, it will rebleed every time you pull the lip out to look at it.
- Lower Lip. Cuts of the lower lip are usually caused by the teeth. They occur when catching the lip between the upper and lower teeth while falling. Most of these cuts do not connect (don't go through the lip). These do not need sutures unless the outer cut is gaping.
- Serious injuries are those to the tonsil, soft palate, or back of the throat. Examples of these injuries include falling with a pencil or toothbrush in the mouth. Puncture wounds here can cause a deep space infection in the neck.
When to Call for Mouth Injury
Call 911 Now
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Self Care at Home
|
Call 911 Now
- Major bleeding that can't be stopped
- Trouble breathing
- You think your child has a life-threatening emergency
Call Doctor or Seek Care Now
- Gaping cut of tongue or inside the mouth that may need stitches
- Gaping cut of the lip that may need stitches
- Severe pain and not better 2 hours after taking pain medicine
- Trouble swallowing fluids or spit
- Can't fully open or close the mouth
- Fever and mouth looks infected. Signs are increasing pain or swelling after 48 hours. Note: it's normal for a healing wound in the mouth to be white.
- You think your child has a serious injury
- You think your child needs to be seen, and the problem is urgent
Call Doctor Within 24 Hours
- Mouth looks infected and no fever
- You think your child needs to be seen, but the problem is not urgent
Call Doctor During Office Hours
- You have other questions or concerns
Self Care at Home
- Minor mouth injury
Care Advice for Minor Mouth Injuries
-
Upper Lip and Frenulum Bleeding - How To Stop:
- Cuts of the inside of the upper lip are very common.
- Often, the piece of tissue that connects the upper lip to the upper gum is torn. This tissue is called the upper labial frenulum.
- The main symptom is oozing tiny amounts of blood.
- This cut always heals perfectly without sutures.
- For bleeding from the frenulum, use direct pressure. Press the outer lip against the teeth for 10 minutes.
- Caution: Once bleeding has stopped, don't pull the lip out to look at it. Reason: The bleeding will start up again.
- It's safe to look at it after 3 days.
-
Lower Lip Bleeding - How to Stop:
- Most children who fall and bite their lower lip have 2 cuts. They have cuts to both the outside and inside of the lip.
- Catching the lower lip between the upper and lower teeth causes the 2 cuts. This tends to happen in children with an overbite.
- Most of these small cuts do not connect with each other.
- For bleeding from the lip, use direct pressure. Press the outer lip against the teeth for 10 minutes.
-
Tongue Bleeding - How to Stop:
- Bites of the tongue rarely need sutures.
- Even if they gape open a little, tongue cuts usually heal quickly. If the edges come together when the tongue is still, it needs no treatment.
- For tongue bleeding, try to press on the bleeding site with a sterile gauze. You can also use a piece of clean cloth. Do this for 5 minutes if it's practical.
- Cuts of the tongue normally tend to ooze a little blood for several hours. This is due to the rich blood supply in the mouth.
- For constant oozing of blood, can use a moistened tea bag for 10 minutes. (Reason: tannic acid released from the tea bag may stop the oozing).
-
Cold for Pain:
- Put a piece of ice or popsicle on the spot that was injured.
- You can also use a cold wet washcloth.
- Do this for 20 minutes.
-
Pain Medicine:
- To help with the pain, give an acetaminophen product (such as Tylenol).
- Another choice is an ibuprofen product (such as Advil).
- Use as needed.
-
Soft Diet:
- Try to get your child to drink adequate fluids.
- Goal: Keep your child well hydrated.
- Cold drinks, milk shakes, popsicles, slushes, and sherbet are good choices.
- Solids. Offer a soft diet. Also avoid foods that need much chewing. Avoid citrus, salty, or spicy foods.
- Rinse the wound with warm water right away after meals.
-
What to Expect:
- Small cuts and scrapes inside the mouth heal up in 3 or 4 days.
- Infections of mouth injuries are rare.
-
Call Your Doctor If:
- Pain becomes severe
- Mouth looks infected (mainly increasing pain or swelling after 48 hours)
- Fever occurs
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.
Mouth Ulcers
Is this your child's symptom?
- Painful, shallow ulcers (sores) on the lining of the mouth
- Found on the gums, inner lips, inner cheeks, or tongue
- Sores only on the outer lips (such as cold sores) are not covered
If NOT, try one of these:
Causes of Mouth Ulcers or Sores
- Canker Sores. The main cause of 1 or 2 mouth ulcers after age 5.
- Hand-Foot-Mouth Disease. The most common cause of multiple ulcers in the mouth. These ulcers are mainly on the tongue and sides of the mouth. Most children also have small deep blisters on the palms and soles. Due to the Coxsackie virus. It is common between ages 1 to 5 years.
- Herpes Simplex Virus (Cold sore virus). The first infection can be severe. It can cause 10 or more ulcers on the gums, tongue and lips. Key findings are additional ulcers on the outer lips or skin around the mouth. Also, fever and difficulty swallowing. Usually occurs age 1 to 3. It usually follows contact with an adult who has active cold sores (fever blisters). Often they have kissed the child.
- Cold Sores (Fever Blisters). Sores are only found outside the mouth on the outer lip. They recur 2 or 3 times a year in the same place. There are no ulcers inside the mouth. Adult cold sores are the cause of Herpes Simplex infections in young children. Occurs in 20% of teens and adults.
- Mouth Injury. Common mouth injuries are biting the tongue or inside of the cheek. Others can be caused by a toothbrush. The lining of the mouth always looks white when it heals. So forgotten injuries can look like a canker sore.
- Mouth Burns. Hot foods (such as pizza) can cause mouth sores. They also turn white as they heal.
Causes of Canker Sores
- Canker sores have many causes.
- Minor injuries to the mouth can trigger a canker sore. Examples are from a rough food or a hard toothbrush. Biting oneself while chewing can start one.
- Food allergies or irritants may also be a trigger.
- Vitamin deficiencies can also be a cause. A vitamin deficiency can occur if your child is a picky eater.
- Canker sores can run in families (genetic).
- Often, the cause is unknown.
Symptoms of Canker Sores
- Small ulcers have a white center with a red border around them
- Size is usually less than ¼ inch (6 mm)
- Found on the inner lips and inner cheeks
- The sores are very painful, even when not eating
- Usually get 1 canker sore at a time. Sometimes get 2 or 3.
- No fever or other symptoms
When to Call for Mouth Ulcers
Call 911 Now
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Self Care at Home
|
Call 911 Now
- Not moving or too weak to stand
- You think your child has a life-threatening emergency
Call Doctor or Seek Care Now
- Chemical in the mouth could have caused ulcers
- Dehydration suspected. No urine in more than 8 hours, dark urine, very dry mouth and no tears.
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Call Doctor Within 24 Hours
- 4 or more ulcers
- Bloody crusts on the lips
- Red, swollen and tender gums
- Ulcers and sores also on the outer lip
- One ulcer on the gum near a tooth with a toothache
- Fever or swollen face
- Large lymph node under the jaw
- Began after starting a medicine
- You think your child needs to be seen, but the problem is not urgent
Call Doctor During Office Hours
- Cold sores suspected
- Mouth ulcers last more than 2 weeks
- You have other questions or concerns
Self Care at Home
- Canker sores suspected
Care Advice for Mouth Ulcers
-
What You Should Know About Mouth Ulcers:
- Canker sores are the most common cause of mouth ulcers.
- They are 1 - 3 painful, white ulcers of inner cheeks, inner lip or gums (no fever).
- Causes include injuries from rough food, tooth brushes, biting, or food irritants.
- Here is some care advice that should help.
-
Liquid Antacid for Mouth Pain (Age 1 Year and Older):
- For mouth pain, use a liquid antacid (such as Mylanta or the store brand). Give 4 times per day as needed. After meals often is a good time.
- Age 1 to 6 years. Put a few drops in the mouth. Can also put it on with a cotton swab.
- Age over 6 years. Use 1 teaspoon (5 mL) as a mouth wash. Keep it on the ulcers as long as possible. Then can spit it out or swallow it.
- Caution: Do not use regular mouth washes, because they sting.
-
Pain Medicine:
- To help with the pain, give an acetaminophen product (such as Tylenol).
- Another choice is an ibuprofen product (such as Advil).
- Use as needed.
-
Fluids and Soft Diet :
- Try to get your child to drink adequate fluids.
- Goal: keep your child well hydrated.
- Cold drinks, milk shakes, popsicles, slushes, and sherbet are good choices.
- Solid Foods. Offer soft, bland foods like macaroni and cheese. Other good ones are mashed potatoes, cereals with milk and ice cream.
- Avoid foods that need much chewing. Avoid citrus, salty, or spicy foods.
- Note: Fluid intake is more important than eating any solids.
- For infants, you may need to stop the bottle. Give fluids by cup, spoon or syringe instead. Reason: The nipple can increase the pain.
-
Return to School:
- Canker sores cannot be spread to others. Children with canker sores do not need to miss any school.
- Children with fever need to be checked before going back to school.
- Also, children with many mouth ulcers should be checked before going back.
-
What to Expect:
- They heal up in 1 to 2 weeks on their own.
- Once they occur, no treatment can shorten the illness.
- Treatment can help with the pain.
-
Call Your Doctor If:
- Mouth ulcers last more than 2 weeks
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.
Neck Pain or Stiffness
Is this your child's symptom?
- Pain or discomfort in the back, side or front of the neck
- Minor muscle strain from overuse and neck injury are included
- Pain in the front of the neck often is from a sore throat. It can also be from a swollen lymph node.
If NOT, try one of these:
Causes of Neck Pain
- Strained Neck Muscles. In teens, new neck pain is mostly from stretched neck muscles (muscle overuse). The most common modern cause is working with the head flexed down. Such head bending occurs with texting or looking at smartphones and mobile devices. Reading lying in bed or working on a computer for hours can trigger neck pain. The neck likes to keep the head in a neutral position. This is because the head is heavy (12 pounds or 5.4 kilograms). Other triggers are sleeping in an awkward position or fixing something on the ceiling.
- Infected Lymph Node. At all ages, it can be from a swollen lymph node. That can irritate and cause spasm of the neck muscle it lies against.
- Whiplash Injury. Caused by sudden movement of the head and neck. The head snaps back and forth. Neck muscles, nerves and ligaments are stretched. Can occur with a rear-end auto collision. Can also be from a sports injury. Needs to be examined.
- Major Neck Injury (Serious). The neck protects the spinal cord. A fracture or other injury of the neck can damage the cord. Therefore, all neck injuries need to on a spine board until they are cleared.
- Meningitis (Very Serious). A bacterial infection of the membrane that covers the spinal cord and brain. The main symptoms are a stiff neck, headache, confusion and fever. A stiff neck means your child can't touch the chin to the chest. Younger children are lethargic or so irritable that they can't be consoled. If not treated early, child can suffer brain damage.
Symptoms
- Neck pains due to strained muscles cause these symptoms:
- The head is often cocked to one side
- Can't bend the head backward or put the chin to each shoulder. Often, can still bend the neck forward (touch the chin to the chest).
- The neck muscles are often sore to the touch
Pain Scale
- Mild: Your child feels pain and tells you about it. But, the pain does not keep your child from any normal activities. School, play and sleep are not changed.
- Moderate: The pain keeps your child from doing some normal activities. It may wake him or her up from sleep.
- Severe: The pain is very bad. It keeps your child from doing all normal activities.
When to Call for Neck Pain or Stiffness
Call 911 Now
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Self Care at Home
|
Call 911 Now
- Pain starts after a major injury such as with contact sports or car crash
- Not moving or too weak to stand
- You think your child has a life-threatening emergency
Call Doctor or Seek Care Now
- Pain started after a minor injury
- Can't move neck normally with fever
- Severe pain
- Not alert when awake ("out of it")
- Acts or talks confused
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Call Doctor Within 24 Hours
- Can't move neck normally
- Headache without fever
- Fever lasts more than 24 hours
- Age less than 5 years old
- You think your child needs to be seen, but the problem is not urgent
Call Doctor During Office Hours
- Cause of neck pain is not clear (no history of overuse)
- Neck pain (from lots of turning) lasts more than 2 weeks
- Neck pains are a frequent problem
- You have other questions or concerns
Self Care at Home
- Strained neck muscles (from turning or overuse) present less than 2 weeks
Care Advice for Strained Neck Muscles
-
What You Should Know About Neck Pain:
- Most new neck pain is from stretching and turning the neck muscles too much. Muscle overuse causes strained neck muscles.
- Long periods of looking down is a common cause of neck pain. Seen mainly with texting or looking down at other mobile devices.
- When muscle pain starts without reason, it can be from sleeping in an awkward position.
- Here is some care advice that should help.
-
Pain Medicine:
- To help with the pain, give an acetaminophen product (such as Tylenol).
- Another choice is an ibuprofen product (such as Advil).
- Use as needed.
-
Cold Pack for Pain:
- During the first 2 days, use a cold pack or ice wrapped in a wet cloth.
- Put it on the sore muscles for 20 minutes.
- Repeat 4 times on the first day, then as needed.
- Reason: Reduces pain and any spasm.
- Caution: Avoid frostbite.
-
Use Heat After 48 Hours:
- If pain lasts over 2 days, put heat on the sore muscle.
- Use a heat pack, heating pad or warm wet washcloth.
- Do this for 10 minutes, then as needed.
- Reason: Increase blood flow and improve healing.
- Caution: Avoid burns.
-
Sleep Position:
- Sleep on the back or side, not the stomach.
- Sleeping with a neck collar helps some people.
- Use a foam neck collar (from a drug store). If don't have one, wrap a small towel around the neck.
- Reason: Keep the head from moving too much during sleep.
-
Activity:
- Protect the neck. Avoid any activity that increases the pain.
- Avoid any sports or work that increase the pain.
- After 48 hours, start a gentle stretching program.
-
Stretching Exercises:
- Do 3 minutes of gentle stretching exercises each day. Reason: improve the tone of the neck muscles.
- Touch the chin to each shoulder. Touch the ear to each shoulder. Move the head forward and backward.
- Don't apply any resistance during these stretching exercises.
-
What to Expect:
- New neck pain without a reason most often goes away in a few days.
- Neck pain from muscle overuse (strained neck muscles) goes away in 1 to 2 weeks.
-
Call Your Doctor If:
- Neck pain becomes severe
- Stiff neck occurs
- Pain starts to shoot into the arms, upper back or legs
- Pain lasts more than 2 weeks
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.
Newborn Appearance Questions
Is this your child's symptom?
- Normal appearance questions about newborns
If NOT, try one of these:
Newborn Appearance - Topics Covered
If your baby is healthy, skip the "What to Do" section. Go directly to the topic number that relates to your question for advice.
- Breast Questions
- Ear and Nose Questions
- Eye Questions
- Genital Questions (Female)
- Genital Questions (Male)
- Hair Questions
- Head Questions
- Leg and Feet Questions
- Mouth Questions
When to Call for Newborn Appearance Questions
Call 911 Now
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Self Care at Home
|
Call 911 Now
- Can't wake up
- Not moving or very weak
- Bluish (or gray) lips, tongue or face now
- You think your child has a life-threatening emergency
Call Doctor or Seek Care Now
- Age less than 1 month old and looks or acts abnormal in any way
- Hard to wake up
- Weak or absent cry and new-onset
- Age less than 12 weeks old with fever. Caution: do NOT give your baby any fever medicine before being seen.
- Swollen breast is red or tender to touch
- Soft spot on top of head looks swollen
- You think your child needs to be seen, and the problem is urgent
Call Doctor Within 24 Hours
- Urine color is pink, orange or peach
- Swelling on head from the birth process looks abnormal or too large
- You think your child needs to be seen, but the problem is not urgent
Call Doctor During Office Hours
- You have other questions or concerns
Self Care at Home
- Normal newborn's appearance
Care Advice for Newborn Appearance
-
Breast Questions: Swollen Breasts
- Swollen breasts are present during the first week of life in many babies. Breasts can be swollen in both girl and boy babies. The nipple area is always firm.
- Cause. The passage of the mother's estrogen across the placenta.
- Newborn Milk. Sometimes, the nipples leak a few drops of milkish discharge. This is normal and can last a few weeks.
- Normal Course. Swollen breasts often last for 2 to 4 weeks. In breastfed babies, some breast swelling can persist for 6 months.
- Caution: Never squeeze or massage the breast or nipple. (Reason: Can cause a serious infection.)
- Call your doctor if: Swollen breast develops any redness, streaking, or tenderness.
-
Ear and Nose Questions:
- Ear Folded Over. The ears of newborns are commonly soft and floppy. Sometimes one of the edges is folded over. The cartilage will slowly harden over the first few weeks. This will cause the outer ear to assume a normal shape.
- Flattened Nose. The nose can become misshapen during the birth process. It may be flattened or pushed to one side. It will look normal by 1 week of age.
-
Eye Questions:
- Bleeding in Eye. A flame-shaped red streak on the white of the eye is common. It's harmless and due to a birth canal injury. The blood will go away in 2 to 3 weeks.
- Swollen Eyelids. The eyes may be puffy due to pressure on the face during delivery. They may be puffy and reddened if silver nitrate eyedrops were used at birth. This irritation should clear in 3 days.
- Tear Duct, Blocked. A constantly watery eye may be a sign of a blocked tear duct. A channel normally carries tears from the eye to the nose. A blocked tear duct means this channel is blocked. See that care guide.
-
Genital Questions (Female):
- Vaginal Tags. The hymen can be swollen due to maternal estrogen. It can have smooth ½ inch (12 mm) projections of pink tissue. These normal vaginal (hymenal) tags occur in 10 percent of newborn girls. They slowly shrink over 2 to 4 weeks.
- Vaginal Discharge. As the maternal estrogen declines in your baby's blood, a vaginal discharge may occur. This discharge is usually clear or white. Sometimes, the discharge will become pink or blood-tinged (false menstruation). This normal discharge should not last more than 3 or 4 days. Discharge from the vagina can occur between 2 and 10 days of life.
-
Genital Questions (Male):
- Swollen Scrotum (Hydrocele). The newborn scrotum can be filled with clear fluid. This fluid is squeezed into the scrotum during the birth process. It slowly goes away over 6 to 12 months.
- No Testicle (Undescended). The testicle is not in the scrotum in about 4% of full-term newborns. Many of these testicles gradually descend into the normal position during the following months. By 1 year of age, less than 1% of all testicles are undescended. These need to be brought down surgically.
- Tight Foreskin. Most babies that aren't circumcised have a tight foreskin. Because of this, you can't see the head of the penis. This is normal in infants. The foreskin should not be pulled back.
- Circumcision. A circumcision is the removal of most of the male foreskin. For questions about circumcisions, see that care guide.
-
Hair Questions:
- Scalp Hair. Most hair at birth is dark-colored. This hair is temporary and begins to shed by 1 month of age. Some babies lose it slowly while the permanent hair is coming in. Others lose it quickly and become bald for a short time. The permanent hair will begin to appear by 6 months. It may be an entirely different color from the newborn hair.
- Body Hair (Lanugo). Lanugo is the fine, downy hair that is sometimes on the back and shoulders. It is more common in premature infants. It is rubbed off with normal friction by 2 to 4 weeks of age.
-
Head Questions:
- Caput is a swelling on top of the head or throughout the scalp. It is due to fluid squeezed into the scalp during the birth process. Caput is present at birth and clears in a few days. It's normal, harmless and painless.
- Cephalohematoma is a collection of blood on the outer surface of the skull. It is due to friction between the skull and the pelvis during birth. The lump is usually confined to one side of the head. It does not cross the midline. It first appears on the second day of life. It may increase in size for up to 5 days. It doesn't go away completely until 2 or 3 months of age. Call your doctor if: The swelling becomes large.
- Molding. Molding refers to the long, narrow, cone-shaped head. This is from passage through a tight birth canal. This compression of the head can temporarily hide the fontanel (soft spot). The head returns to a normal shape in a few days.
-
Soft Spot (Anterior Fontanel). The front "soft spot" is diamond-shaped. It is covered by a thick fibrous layer. Touching this area is quite safe. The purpose of the soft spot is to allow rapid growth of the brain. It closes over with bone between 12 and 18 months of age. (Normal range is 5 to 24 months of age.) The back "soft spot" is smaller and triangular-shaped. It closes between 2 and 3 months. The soft spot normally looks flat or a little sunken. It may pulsate with each beat of the heart. This is normal. The only abnormal soft spot is one that is bulging (swollen).
A sunken soft spot is not a sign of illness unless the baby is dehydrated. Then it would be very depressed and the baby would not act well.
-
Leg and Feet Questions:
- Bowed Legs. The lower legs (tibia) normally curve in. This is because of the cross-legged posture while in the womb. If you stand your baby up, the upper legs will be bowed. Both of these curves are normal. These curves will straighten out after the child has been walking for 6 to 12 months.
- Feet Turned In, Out or Up. Feet can turn any which way. This is due to the cramped quarters inside the womb. This is normal if the feet can be easily moved to a normal position. The feet should be flexible. The direction of the feet will become more normal between 6 and 12 months of age.
- "Ingrown" Toenails. Many newborns have soft nails that easily bend and curve. However, they are not truly ingrown because they don't cut into the flesh.
-
Mouth Questions:
- Tongue-Tie. A short, tight band that connects the tongue to the mouth in newborns. This band normally stretches with time, movement, and growth. Tongue-tie rarely causes any symptoms.
- Epithelial Pearls. Little white-colored cysts can occur in the mouth. Look along the gumline or on the hard palate. These are due to blockage of normal mucous glands from friction with sucking. They go away by 1 to 2 months of age.
-
Teeth:
- The presence of a tooth at birth is a rare event.
- About 10 percent of them are extra teeth without a root structure.
- The other 90 percent are prematurely erupted normal teeth. The distinction can be made with an X-ray.
- The extra teeth should be removed, usually by a dentist.
- The normal teeth need to be removed only if they become loose. Reason: Risk of choking. They should also be removed if they cause sores on the tongue.
-
For Newborns, Always Call Your Doctor If:
- Your baby starts to look or act abnormal in any way
- You think your child needs to be seen
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.
Newborn Illness - How to Recognize
Is this your child's symptom?
- How infections and other serious diseases can present in newborns
Why Newborns Need to be Watched Closely
- Newborns are at higher risk for infections. Infections may present at any time during the first month. Watch your baby carefully for signs of illness. This is especially crucial during the first 7 days of life.
- Newborns that get a blood infection (sepsis) can get very sick quickly.
- The symptoms of serious illness in newborns can be subtle. The question below deals with sick newborns:
- "Age under 1 month old (newborn) and starts to look or act abnormal in any way." Look for this question in the "Call Your Doctor Now" section. It is listed in at least 10 topics.
- Feeding is the one reliable measure of a newborn's well-being. Newborns should be eating machines. If your baby isn't feeding well, call your baby's doctor. Also, call if your baby has an abrupt change in his feeding pattern. (Exception: never a good feeder, but takes enough milk and nothing has changed).
- If how your baby looks or acts changes and it's not normal, call now. Don't wait to call your baby's doctor for expert advice.
When to Call for Newborn Illness - How to Recognize
Call 911 Now
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
|
Self Care at Home
|
Call 911 Now
- Can't wake up
- Not moving or very weak
- Bluish (or gray) lips, tongue or face now
- You think your child has a life-threatening emergency
Call Doctor or Seek Care Now
- Any symptoms of illness such as coughing, diarrhea or vomiting. Vomiting bile (green color) is always bad.
- Changes in feeding. Signs are having to wake up for feeds or can't finish feeds.
- Weak suck or can't suck for very long
- Sweating during feeds
- Sleeping more than normal
- Change in muscle tone (decreased or floppy)
- Decreased movement
- Change in color (such as pale, bluish or gray arms and legs)
- Age less than 12 weeks old with fever. Caution: do NOT give your baby any fever medicine before being seen.
- Low temperature below 96.8° F (36.0° C) rectally that does not go up with warming
- New moaning or grunting noises with each breath
- Change in cry, such as weak cry or strange cry
- You think your child needs to be seen, and the problem is urgent
Call Doctor Within 24 Hours
- Urine color is pink, orange or peach
- You think your child needs to be seen, but the problem is not urgent. (Has none of the urgent symptoms listed above)
- You have other questions or concerns
Self Care at Home
- Your baby is feeding, moving and sleeping normally
- There are no signs of illness
- Your newborn is well
Care Advice for Newborns Without Signs of Illness
-
What You Should Know About Newborn Illness:
- Based on this review, your baby doesn't have any signs of illness right now.
- The symptoms of serious illness in newborns can be subtle. Watch your baby carefully for signs of illness. If how your baby looks or acts changes and it's not normal, call now.
- During the early weeks of life, careful watching is always the best approach.
-
Call Your Doctor If:
- Your baby has a fever
- Your baby has any symptoms of illness
- Your baby starts to look or act abnormal in any way
- You think your child needs to be seen
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.
Newborn Rashes and Birthmarks
Is this your child's symptom?
- Normal skin rashes and birthmark questions about newborns
If NOT, try one of these:
Newborn Rashes - Topics Covered
If your baby is healthy, skip the "What to Do" section. Go directly to the topic number that relates to your question for advice.
- Acne. Small red bumps on the face (onset 2-4 weeks).
- Drooling or Spit-Up Rash. Rash around the mouth and on the chin (onset anytime).
- Erythema Toxicum. Red blotches with small white "pimple" in the center (onset 2-3 days).
- Skin Injury from Birth Process. From forceps, scalp electrode or birth canal (present at birth).
- Milia. Tiny white bumps on the nose and cheeks (present at birth).
- Mongolian Spots. Bluish-green birthmark, often on buttock (present at birth).
- Stork Bites (Pink Birthmarks). On back of neck or bridge of nose (present at birth).
- Strawberry Hemangiomas. Raised red birthmarks (onset 2-4 weeks).
- Port-wine Stains. Dark red or purple flat birthmarks (present at birth).
Newborn Face Rashes: Most Common Ones
- Erythema Toxicum 50% (onset day 2 or 3)
- Milia 40% (present at birth)
- Baby Acne 30% (onset week 2 to 4)
- Drooling or Spit-up Rash (common and onset any time)
- Heat Rash (common and onset any time)
Heat Rash
- Many newborn rashes that have no clear cause are heat rashes.
- Heat rashes are a pink blotchy area with tiny bumps.
- They mainly occur on the face, neck and chest.
- During hot weather, most temporary newborn rashes are heat rashes.
- Cause: blocked off sweat glands. The openings are so tiny in newborns, that any irritation can block them. Examples are getting any ointment on the skin, friction from clothing or being overheated. Being held against the mother's skin while nursing causes many face rashes.
Herpes Simplex: Serious Newborn Rash
- Appearance. Several water blisters or pimples grouped in a cluster. They look like the cold sores (fever blisters) that adults get on their lip. After several days, they crust over.
- Location. Just one part of the body, usually the scalp or face.
- Redness. The base can be pink. The pinkness does not extend beyond the cluster of vesicles.
- Onset. Within the first 2 weeks of life.
- Importance. Early treatment with anti-viral drugs can prevent serious problems. If you think your newborn's rash looks like herpes, call your child's doctor now.
- Imitator. Although herpes can be confused with erythema toxicum, they look very different.
When to Call for Newborn Rashes and Birthmarks
Call 911 Now
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Self Care at Home
|
Call 911 Now
- Not moving or very weak
- You think your child has a life-threatening emergency
Call Doctor or Seek Care Now
- Age less than 1 month old and looks or acts abnormal in any way
- Age less than 12 weeks old with fever. Caution: do NOT give your baby any fever medicine before being seen.
- Purple or blood-colored spots or dots not present at birth
- Tiny blisters (little bumps that contain clear fluid)
- Pimples (little bumps that contain pus). Exception: looks like erythema toxicum which occurs in half of newborns.
- Skin looks infected (such as spreading redness, sores or pus)
- Rash is painful to touch
- You think your child needs to be seen, and the problem is urgent
Call Doctor Within 24 Hours
- You think your child needs to be seen, but the problem is not urgent
Call Doctor During Office Hours
- Mild newborn rash, but cause is not clear
- You have other questions or concerns
Self Care at Home
- Normal newborn rashes or birthmarks
Care Advice for Newborn Rashes and Birthmarks
-
Acne:
- More than 30 percent of newborns develop baby acne of the face. Acne consists of small red bumps.
- This baby acne begins at 2 to 4 weeks of age. It lasts until 4 to 6 months of age.
- The cause appears to be the transfer of maternal hormones just prior to birth.
- Since it goes away on its own, no treatment is needed. Baby oil or ointments make it worse.
-
Drooling or Spit-up Rash:
- Many babies have a rash on the chin or cheeks that comes and goes. This is often due to contact with food. It's more common after starting baby foods. In newborns, it can also be from stomach acid that has been spit up. Prolonged contact with spit-up during sleep can cause the rash to get worse.
- Other temporary rashes on the face are heat rashes. These can occur in areas held against the mother's skin during nursing. Heat rashes are more common in the summertime.
- Rinse the face with water after all feedings or spitting up. During hot weather, change the baby's position more often. Also, put a cool wet washcloth on the rash. Do this for 10 minutes.
-
Erythema Toxicum:
- More than 50 percent of babies get a rash called erythema toxicum. It starts on the second or third day of life.
- It's a harmless baby rash that doesn't need to be seen.
- The rash is made up red blotches. They are ½ inch to 1 inch (1 to 2.5 cm). The blotches have a small white or yellow "pimple" in the center.
- They look like insect bites, but are not. Red blotches are the main feature.
- They can be numerous, keep occurring, and look terrible. They can occur anywhere on the body surface, except the palms and soles.
- Their cause is unknown, but they are not an infection.
- They go away by 1-2 weeks of age.
- No treatment is needed. Ointments or baby oil make it worse.
-
Skin Injury from Forceps, Scalp Electrode or Birth Canal:
- The pressure of a forceps on the skin can leave marks. You may see bruises or scrapes anywhere on the head or face.
- During birth, skin overlying bony prominences can become damaged. You might see this on the sides of the skull bone. This is from pressure from the birth canal. Even without a forceps delivery, you may see bruises or scrapes.
- Scalp electrodes can also cause scalp scrapes and scabs.
- The bruises and scrapes will be noted at birth. They will be more noticeable by day 2. They heal over or go away by 1 - 2 weeks of age.
- A fat tissue injury won't appear until day 5 to 10. Look for a firm coin-shaped lump. It will be under the skin and sometimes with a scab. This lump may take 3 or 4 weeks to go away.
- For any breaks in the skin, apply an antibiotic ointment (such as Polysporin). No prescription is needed. Use 3 times per day until healed.
- Call Your Doctor If:
- It becomes tender to the touch
- Becomes soft in the center
- Starts to looks infected
-
Milia:
- Milia are tiny white bumps that occur on the face. The nose and cheeks are most often involved. Milia can also be seen on the forehead and chin.
- Milia occur in 40 percent of newborn babies. Present at birth.
- Milia are many in number. They occur equally on both sides of the face.
- Although they look like pimples, they are much smaller (pinhead size). They are not infected.
- They do not look like water blisters.
- They are blocked-off skin pores. They will open up.
- Milia will go away by 1 to 2 months of age.
- No treatment is needed. Ointments or creams can make them worse.
-
Mongolian Spots:
- A Mongolian spot is a normal bluish-green or bluish-grey flat birthmark. They occur in over 90 percent of Native American, Asian, Hispanic, and African American babies. They are also seen in 10 percent of Caucasians, especially those of Mediterranean descent.
- They are present at birth.
- They occur most commonly over the back and buttocks. However, they can be present on any part of the body.
- They vary greatly in size and shape.
- They do not indicate illness or any disease.
- Most fade away by 2 or 3 years of age. A trace may persist into adult life.
-
Stork Bites (Pink Birthmarks):
- Flat pink birthmarks that occur over the bridge of the nose or the eyelids. You can also find them on the back of the neck ("stork bites"). The ones in front are often referred to as "an angel's kiss".
- They occur in more than 50 percent of newborns. They are present at birth.
- All the birthmarks on the bridge of the nose and eyelids clear completely. Those on the eyelids clear by 1 year of age. Those on the bridge of the nose may persist for a few more years. Those on the forehead from the nose up to the hairline usually persist into adulthood. Laser treatment during infancy should be considered. Most birthmarks on the nape of the neck also clear. But, 25 percent can persist into adult life.
-
Strawberry Hemangiomas:
- Strawberry hemangiomas are red birthmarks that are raised or increasing in size.
- Onset usually between 2-4 weeks of age. Most often, start after 3 weeks of age. Sometimes (although rare), they don't appear until the second month of life.
- They become larger for 1 year. Then, they fade away over 6 to 8 years without any treatment.
- They run a small risk of bleeding with trauma. Any bleeding should stop with 10 minutes of direct pressure.
- Discuss with your child's doctor on the next regular visit. Call sooner if you are concerned.
-
Port-Wine Stain Birthmarks:
- Present at birth in 1 out of 200 newborns
- Deeper in color (dark red or purple) than stork bites (salmon patches)
- Flat, smooth surface
- Natural course: Do not fade or disappear like stork bites. May become darker.
- Grow with the child, but cover the same area
- Treatment: May refer to dermatologist for laser treatments early in infancy
-
Call Your Doctor If:
- Your baby starts to look or act abnormal in any way
- You think your child needs to be seen
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.

This photo shows a monglian spot on the buttocks. This is a type of colored birthmark. These marks are blue-grey and flat. They are usually irregular shaped with wavy borders. Mongolian spots are not cancerous.

This photo shows a Strawberry Hemangioma on the abdominal wall. A hemangioma is a cluster of blood vessels that cause non-cancerous growths.

This shows a storkbite which is a birthmark often found in babies. These birthmarks usually go away on their own.
Some brief notes about capillary hemangiomas:
- Flat pink birthmark
- Present in 50% of newborns
- Also called salmon patches
- Most fade by 3 years, but 25% persist into adulthood

This is a three year old child with a strawberry hemangioma of the lower forehead.
Some brief notes about strawberry hemangioma:
- Raised red birthmark
- Often increases in size for first 1-2 years of life
- Then start to shrink down without any treatment
- Turns grayish when it shrinks down, as in this 3 year old child
- Usually flat and gone by 8 years old or sooner

Over 50 percent of babies get this rash around the second or third day of life.
The rash is composed of ½ inch (1.25 cm) to 1 inch (2.5 cm) red blotches with a small white or yellow lump in the center. The red blotches can be numerous and can occur anywhere on the body (except the palms and soles). They can look quite terrible.
The cause of erythema toxicum is unknown. However, it is harmless the rash goes away by 2 weeks of age.

This shows baby (neonatal) acne on the cheeks and side of the face. There are red and white raised bumps.
Newborn Reflexes and Behavior
Is this your child's symptom?
- Normal reflexes, noises and behavior questions in newborns
- These are normal and not signs of illness
- Flying and mountain travel with newborns is also covered
If NOT, try one of these:
Newborn Reflexes - Topics Covered
These harmless behaviors fall into 11 general groups. If your baby is healthy, skip the "What to Do" section. Go directly to the topic number that relates to your question for advice.
- Normal primitive reflexes from immature nervous system
- Normal jitteriness when crying
- Normal sleep movements
- Normal breathing sounds and noises
- Normal irregular breathing patterns
- Normal GI sounds and noises
- Normal sleep sounds and noises
- Normal feeding reflexes
- Normal protective reflexes
- Flying with newborns, safety of
- Mountain travel with newborns, safety of
When to Call for Newborn Reflexes and Behavior
Call 911 Now
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Self Care at Home
|
Call 911 Now
- Can't wake up
- Not moving or very weak
- Weak cry and new onset
- Severe trouble breathing (struggling for each breath)
- New moaning or grunting noises with each breath
- Bluish (or gray) lips, tongue or face now
- You think your child has a life-threatening emergency
Call Doctor or Seek Care Now
- Age less than 1 month old and looks or acts abnormal in any way. Examples are a poor suck or poor color.
- Hard to wake up
- Age less than 12 weeks old with fever. Caution: do NOT give your baby any fever medicine before being seen.
- Breathing stopped for more than 10 seconds and now it's normal
- Trouble breathing, but not severe
- Seizure suspected
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Call Doctor Within 24 Hours
- You think your child needs to be seen, but the problem is not urgent
Call Doctor During Office Hours
- You have other questions or concerns
Self Care at Home
- Normal newborn reflexes and behavior
- Flying or mountain travel with a newborn
Care Advice for Newborn Reflexes and Behavior
-
Normal Primitive Reflexes From Immature Nervous System:
- Startle Reflex (Moro or embrace reflex). Brief stiffening of the body, straightening of arms and opening of hands. Follows noise or abrupt movements. Frequent at birth. Slowly resolves by 4 months of age.
- Tonic-Neck Reflex (Fencer's Reflex). When head is turned to 1 side, the arm and leg on that side straightens. The opposite arm and leg flexes. Goes away by 4 months of age.
- Chin Trembling
- Lower Lip Quivering
- Jitters or Trembling (see Topic 2)
-
Normal Jitters or Trembling when Crying:
- Jitters or trembling of the arms and legs during crying is normal in newborns. It should stop by 1 to 2 months of age.
- If your baby is jittery when not crying, it could be abnormal. Give her something to suck on. (Reason: Normal trembling should stop with sucking.)
- Seizures are rare. During seizures, newborns are more than jittery. They have muscle jerking and blinking of the eyes. Babies can also make sucking movements of the mouth. They don't cry during seizures.
- Call Your Doctor If:
- The jitters get worse
- The jitters occur when your baby is calm
-
Normal Sleep Movements:
- Sleep is not quiet. Expect some of the following:
- Sudden jerks or twitches of the arms, hands or legs. If they only occur during sleep, they are most likely normal.
- How Long: last a few seconds, but can recur
- Timing: soon after falling asleep
- Normal at all ages, not just in newborns
- Suspect a seizure if: jerking occurs when awake or lasts more than 10 seconds
-
Normal Breathing Sounds and Noises:
- Throat Noises. Caused by air passing through normal saliva or refluxed milk. These gurgling noises are likely to build up during sleep. Slowly, the newborn learns to swallow more often.
- Nasal Noises are usually caused by dried mucus in the nose. Your baby most likely doesn't have a cold. A blocked or stuffy nose can interfere with feeding. This is because your baby can't breathe when the mouth is closed with feeding. Therefore, babies need help opening the nasal passages.
- Nasal Saline. Clean out the nose with saline (salt water) nose drops (such as store brand). If not available, can use bottled water. Use 1 drop at a time and do 1 side at a time. Repeat this several times. This will loosen up the dried mucus. Then, it can be sneezed out or swallowed. If needed, use a suction bulb. Avoid Q-tips which can injure the lining of the nose. Saline nose drops or spray can be bought in any drugstore. No prescription is needed.
- Tobacco Smoke. Avoid tobacco smoke which can cause nasal congestion or sneezing. Avoid dust or any strong odors for the same reason.
- Call Your Doctor If:
- Nasal washes don't work
- Breathing becomes hard
-
Normal Irregular Breathing Patterns:
- Transient Breathing Pauses of Less Than 10 Seconds. Also Called Periodic Breathing. Often, the pause is followed by some faster breathing to "catch-up." These breathing pauses are normal if the baby is comfortable during them. A normal rate should be less than 60 breaths per minute. Usually resolves by 1 month of age. Call your doctor if: Your baby is breathing fast or turned blue.
- Transient Rapid Breathing. Sometimes, newborns take rapid, progressively deeper breaths. This is so they can expand their lungs all the way. This is normal if the breathing slows to normal within a minute or so.
- Seesaw Breathing. With breathing, the chest seems to contract when the stomach expands. The cause is the soft rib cage of some newborns. It tends to pull in during normal downward movement of the diaphragm.
- Yawning or Sighing (off and on) to open up the lungs
- Call Your Doctor If:
- Breathing becomes hard
- Breathing pauses last more than 10 seconds
- You have other questions or concerns
-
Normal GI Sounds And Noises:
- Belching air from stomach
- Passing gas per rectum
- Note: Both of these are releasing swallowed air. They are normal, harmless and lifelong. They do not cause pain or crying.
- Gurgling or growling noises from the movement of food through the intestines
- Normal grunting with pushing out stools
- Hiccups. Hiccups are often caused by overeating. They can also be from a little acid irritating the lower esophagus. Give your baby a few swallows of water to rinse off the lower esophagus.
-
Normal Sleep Sounds And Noises: Normal sleep is not motionless or quiet. Expect some of the following:
- Moving during sleep transitions
- Occasional startle reflex or jerks
- Breathing noises - especially gurgling from secretions that sit in the throat.
- During light sleep, babies can normally whimper, cry, groan or make other strange noises.
- Parents who use a nursery monitor often become concerned about these normal sleep sounds.
- GI tract noises from normal movement of digested food
-
Normal Feeding Reflexes:
- Rooting Reflex. When the side of the mouth or cheek is touched, your baby turns to that side. He will open his mouth in preparation for nursing. Present until 6 months of age.
- Sucking Reflex. Will suck on anything placed in the mouth. This survival reflex does not imply hunger. It is even present right after a feeding. This reflex fades between 6 and 12 months of age.
-
Normal Protective Reflexes:
- Sneezing To Clear Nose of Any Irritant. Sneezing helps to open the nose. It's usually caused by dust, fuzz, tobacco smoke or other strong odors. If sneezing becomes frequent, use nasal washes. This is not caused by an allergy.
- Coughing to clear lower airway
- Blinking. After spending 9 months in darkness, newborns have light-sensitive eyes. At first, they prefer to keep their eyes closed. They blink often with light exposure.
-
Flying With Newborns:
- Never fly during the first 7 days of life. If flying is needed, it's safe to fly after 7 days of age.
- If your newborn is not healthy, do not fly. Your child's doctor should give medical clearance first before flying.
- Your baby can be exposed to infections aboard aircraft. Therefore, it is preferable not to fly before 2 or 3 months of age.
-
Mountain Travel With Newborns:
- Avoid mountain travel above 8,000 feet (2,438 meters) for the first month of life. (Exception: family lives there year-round)
- Travel to destinations below 8,000 (2,438 meters) feet is safe.
- Brief drives over higher mountain passes are safe.
- If your newborn is not healthy, don't travel above 8,000 feet (2,438 meters). Your child's doctor should give medical clearance first.
-
Call Your Doctor If:
- Your baby starts to look or act abnormal in any way
- You think your child needs to be seen
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.
Nose Allergy (Hay Fever)
Is this your child's symptom?
- An allergic reaction of the nose, usually from pollen
- An itchy nose, clear discharge and sneezing is common
If NOT, try one of these:
Triggers of Nasal Allergies
- Cause. An allergic reaction of the nose and sinuses to an inhaled substance. The medical name for this is allergic rhinitis. The allergic substance is called an allergen.
- Most allergens float in the air. That's how they get in the nose. Here are the common ones:
- Pollens. Trees, grass, weeds and molds are the most common pollens. Tree pollens come in the spring. Grass pollens come in the summer. Weed pollens come in the fall. Pollens cause seasonal allergies. You can't avoid pollens because they are in the air. Most nasal allergies continue through the pollen season. They can last 4 to 8 weeks. Pollens cause seasonal allergic rhinitis. This is also called hay fever.
- Pets. Allergens can also be from cats, dogs, horses, rabbits and other animals. Most people don't keep a pet that they are allergic to. They only have sporadic allergy symptoms when they are exposed to that specific animal. These symptoms will usually last a few hours. If someone with a cat visits you, they will bring cat dander with them. This will cause brief symptoms. If you own the pet, though, your child will have symptoms all the time.
- House Dust. House dust contains many allergens. It always contains dust mites. If your humidity is high, it will contain mold. House dust causes year round, daily symptoms. The medical name for this is perennial allergic rhinitis.
Symptoms of Nasal Allergies
- Clear nasal discharge with sneezing, sniffing, and itching of nose (100%)
- Eye allergies (itchy, red, watery and puffy) also can occur (70%)
- Ear and sinus congestion or fullness can occur
- Throat can also feel scratchy or have a tickly feeling at times
- Itchy ear canals, itchy skin or hoarse voice sometimes also occur
- Symptoms happen during pollen season
- Same symptoms during the same month of the last year
- Past diagnosis by a doctor is helpful
- No fever
How to Tell Seasonal Nasal Allergies from the Common Cold
- Symptoms happen during pollen season
- Had the same symptoms during the same month last year
- Hay fever symptoms last 6-8 weeks for each pollen. (Colds last 1-3 weeks).
- Allergies: itchy eyes and nose. Not seen with colds.
- Colds: fever and/or sore throat. Not seen with allergies
- Both: runny nose and watery eyes. Can also have a cough with both, but less common with allergies.
Nose and Eye Allergies: Age of Onset
- Seasonal pollen allergies usually begin at age 2 to 5 years.
- The symptoms peak in school age children, teens and young adults.
- Pollen symptoms are rare in children under age 2. They require at least 2 seasons of exposure to the pollen.
- Children under age 2 who have chronic nasal symptoms have other causes. Examples are recurrent colds, large adenoids or cow's milk allergy.
- Food allergies can start during the first year of life, but not pollen allergies.
When to Call for Nose Allergy (Hay Fever)
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Self Care at Home
|
Call Doctor Within 24 Hours
- You think your child needs to be seen
- Lots of coughing
- Sinus pain (not just congestion) does not go away with allergy medicines. Note: sinus pain is around the cheekbone or eyes.
Call Doctor During Office Hours
- Hay fever symptoms make it hard to go to school or do normal activities. Note: taking allergy medicine for 2 days has not helped.
- Diagnosis of hay fever has never been made by a doctor
- Year-round symptoms of nasal allergies
- Snoring is a frequent problem
- You have other questions or concerns
Self Care at Home
- Nasal allergy symptoms or hay fever
Care Advice for Nose Allergies or Hay Fever
-
What You Should Know About Nose Allergies or Hay Fever:
- Hay fever is very common. It happens in about 15% of children.
- Nose and eye symptoms can be controlled by giving allergy medicines.
- Pollens are in the air every day during pollen season. So, allergy meds must be given daily. They need to be used for 2 months or longer during pollen season.
- Here is some care advice that should help.
-
Allergy Medicines:
- Allergy medicines are called antihistamines. They are the drug of choice for nasal allergies.
- They will help control the symptoms. These include a runny nose, nasal itching and sneezing.
- You can give a short-acting allergy medicine (such as Benadryl). No prescription is needed. It needs to be given every 6 to 8 hours.
- The bedtime dosage is especially important for healing the lining of the nose.
- The key to control is to give allergy meds every day during pollen season.
-
Long-Acting Allergy Medicines:
- You can also use a long-acting allergy medicine (such as Zyrtec). No prescription is needed.
- Advantage: Causes less sedation than older allergy meds such as Benadryl. It is long-acting and last up to 24 hours.
- Dose:
- Age 2-5 years old, discuss with your child's doctor. If approved, give 2.5 mg (2.5 mL or ½ teaspoon) of liquid syrup. Use once daily in the morning.
- Age 6-11 years old, give 5 mg chewable tablet once daily in morning.
- Age 12 years and older, give 10 mg tablet once daily in morning.
- Downside: Doesn't control hay fever symptoms as well as older allergy medicines. Also, sometimes will have breakthrough symptoms before 24 hours. If that happens, you can give a single dose of Benadryl.
- Cost: ask the pharmacist for a store brand. Reason: Costs less than the brand name products.
-
Nasal Saline to Wash Out Pollen:
- Use saline (salt water) nose drops or spray (such as store brand). This helps to wash out pollen or to loosen up dried mucus. If you don't have saline, you can use a few drops of water. Use bottled water, distilled water or boiled tap water. Teens can just splash a little water in the nose and then blow.
- Step 1: Put 3 drops in each nostril.
- Step 2: Blow each nostril out while closing off the other nostril. Then, do the other side.
- Step 3: Repeat nose drops and blowing until the discharge is clear.
- How often: Do nasal saline rinses when your child can't breathe through the nose. Also, do them if the nose is very itchy.
- Saline nose drops or spray can be bought in any drugstore. No prescription is needed.
- Saline nose drops can also be made at home. Use ½ teaspoon (2 mL) of table salt. Stir the salt into 1 cup (8 ounces or 240 mL) of warm water. Use bottled water or boiled water to make saline nose drops.
- Other option: Use a warm shower to loosen mucus. Breathe in the moist air, then blow each nostril.
-
Eye Allergy Treatment:
- For eye symptoms, wash off the face and eyelids. This will remove pollen or any other allergic substances.
- Then put a cold wet washcloth on the eyes.
- Most often, an allergy medicine given by mouth will help the eye symptoms. Sometimes, eye drops are also needed. (See below # 6 and #7)
-
Antihistamine Eye Drops - Ketotifen (1st Choice) for Eye Allergy Symptoms:
- Ketotifen eye drops (such as Zaditor) are a safe and effective product. No prescription is needed.
- Dose: 1 drop every 12 hours.
- For severe allergies, use ketotifen eyedrops every day during pollen season. This will give the best control.
-
Antihistamine/Vasoconstrictive Eye Drops (2nd Choice) for Eye Allergy Symptoms:
- Ask your pharmacist to suggest a brand (such as Visine-A). The A stands for antihistamine. No prescription is needed.
- Dose: 1 drop every 8 hours
- Do not use for over 5 days. Reason: Will cause red eyes from rebound effect.
- Downside: Doesn't work as well as Ketotifen eye drops.
-
Wash Pollen Off Body:
- Remove pollen from the hair and skin with shampoo and a shower. This is especially important before bedtime.
-
What to Expect:
- Since pollen allergies recur each year, learn to control the symptoms.
-
Pollen - How to Reduce the Pollen Your Child Breathes:
- Pollen is carried in the air.
- Keep windows closed in the home, at least in your child's bedroom.
- Keep windows closed in car. Turn the air conditioner on recirculate.
- Avoid window fans or attic fans. They pull in pollen.
- Try to stay indoors on windy days. Reason: The pollen count is much higher when it's dry and windy.
- Avoid playing with the outdoor dog. Reason: Pollen collects in the fur.
- Pollen Count: You can get your daily pollen count from Pollen.com. Just type in your zip code.
-
Call Your Doctor If:
- Symptoms are not better in 2 days after starting allergy medicine
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.
Nosebleed
Is this your child's symptom?
- Bleeding from 1 or both nostrils
- Not caused by an injury
If NOT, try one of these:
Causes of Nosebleeds
Nosebleeds are common because of the rich blood supply of the nose. Common causes include:
- Spontaneous Nosebleed. Most nosebleeds start up without a known cause.
- Rubbing. Rubbing or picking the nose is the most common known cause. It's hard to not touch or rub the nose.
- Blowing. Blowing the nose too hard can cause a nose bleed.
- Suctioning. Suctioning the nose can sometimes cause bleeding. This can happen if the suction tip is put in too far.
- Sinus Infections. The main symptoms are lots of dry snot and a blocked nose. This leads to extra nose blowing and picking. The sinus infection is more often viral than bacterial.
- Nose Allergies. The main symptom is a very itchy nose. This leads to extra rubbing and blowing.
- Dry Air. Dryness of the nasal lining makes it more likely to bleed. In the winter, forced air heating often can dry out the nose.
- Allergy Medicines. These help the nasal symptoms, but also dry out the nose.
- Ibuprofen and Aspirin. These medicines increase the bleeding tendency. Aspirin is not used in children.
- Bleeding Disorder (Serious). This means the blood platelets or clotting factors are missing or not working right. A bleeding disorder should be suspected if the nosebleed can't be stopped. Excessive bleeding from the gums or with minor cuts is also a clue. Bleeding disorders are a rare cause of frequent nosebleeds.
When to Call for Nosebleed
Call 911 Now
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Self Care at Home
|
Call 911 Now
- Passed out (fainted) or too weak to stand
- You think your child has a life-threatening emergency
Call Doctor or Seek Care Now
- Nosebleed that won't stop after 10 minutes of squeezing the nose correctly
- Large amount of blood has been lost
- New skin bruises or bleeding gums not caused by an injury also present
- High-risk child (such as with low platelets or other bleeding disorder)
- You think your child needs to be seen, and the problem is urgent
Call Doctor Within 24 Hours
- You think your child needs to be seen, but the problem is not urgent
Call Doctor During Office Hours
- Age less than 1 year old
- New onset nosebleeds happen 3 or more times in a week
- Hard-to-stop nosebleeds are a frequent problem
- Easy bleeding is present in other family members
- You have other questions or concerns
Self Care at Home
- Mild nosebleed
Care Advice for Nosebleed
-
What You Should Know About Nosebleeds:
- Nosebleeds are common.
- You should be able to stop the bleeding if you use the correct technique.
- Here is some care advice that should help.
-
Squeeze the Lower Nose:
- Gently squeeze the soft parts of the lower nose together. Gently press them against the center wall for 10 minutes. This puts constant pressure on the bleeding point.
- Use the thumb and index finger in a pinching manner.
- If the bleeding continues, move your point of pressure.
- Have your child sit up and breathe through the mouth during this procedure.
- If rebleeds, use the same technique again.
-
Put Gauze into the Nose:
- If pressure alone fails, use a piece of gauze. Wet it with a few drops of water. Another option is to put a little petroleum jelly (such as Vaseline) on it.
- Insert the wet gauze into the side that is bleeding. Press again for 10 minutes. Reason it works: the gauze puts more pressure on the bleeding spot.
- Special nose drops: if your child has lots of nose bleeds, buy some decongestant nose drops. An example is Afrin. No prescription is needed. Put 3 drops on the gauze and press. The nose drops also shrink the blood vessels in the nose.
- Caution: don't use decongestant nose drops if your child is under 1 year of age.
- If you don't have gauze, use a piece of paper towel.
- Repeat the process of gently squeezing the lower soft parts of the nose. Do this for 10 minutes.
-
Prevent Recurrent Nosebleeds:
- If the air in your home is dry, use a humidifier to keep the nose from drying out.
- For nose blowing, blow gently.
- For nose suctioning, don't put the suction tip very far inside. Also, move it gently.
- Do not use aspirin and ibuprofen. Reason: Increases bleeding tendency.
- Bleeding areas in the front of the nose sometimes develop a scab. It may heal slowly and re-bleed. If that happens to your child, try this tip. Apply a small amount of petroleum jelly (Vaseline) to the spot. Repeat twice a day. Do not use for more than 1 week.
-
What to Expect:
- Over 99% of nosebleeds will stop if you press on the right spot.
- It may take 10 minutes of direct pressure.
- After swallowing blood from a nosebleed, your child may vomit a little blood.
- Your child may also pass a dark stool tomorrow from swallowed blood.
-
Call Your Doctor If:
- Can't stop bleeding with 10 minutes of direct pressure done correctly
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.
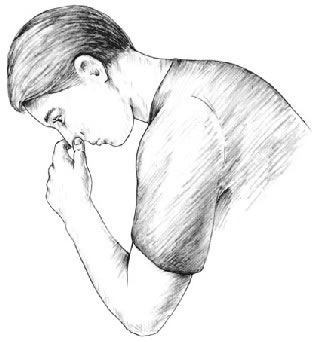
- Sit up and lean forward. This will keep the blood from running down the back of the throat.
- Apply Pressure. Gently squeeze the lower soft parts of the nose against the center wall for 10-15 minutes. Use your thumb and your index finger in a pinching manner.
- If the bleeding continues, move your point of pressure and repeat again for another 10-15 minutes.
Special Notes: The goal is to apply continuous pressure to the bleeding point inside the nose.
Penis-Scrotum Symptoms
Is this your child's symptom?
- Symptoms of the male genitals (penis or scrotum)
- Not caused by an injury
If NOT, try one of these:
Symptoms
- Penis symptoms include rash, pain, itching, and swelling. Discharge from the end of the penis is also included.
- Scrotum symptoms include rash, itching, pain and swelling.
- Any genital pain that is not due to an injury is covered.
Causes of Rashes on Penis or Scrotum
- Most rashes on the penis or scrotum are caused by skin irritants.
- Hand-to-penis contact is normal when passing urine. Therefore, the rash is most likely from an irritant that was on the hands.
- Examples are plants (such as weeds) or chemicals (such as bug spray). Fiberglass, pet saliva or even food can also be irritants.
- Rashes are more common in the summer. Reason: Children are outdoors and have more contact with plants and pollens.
Types of Foreskin Retraction Problems
- Paraphimosis. Forceful retraction can cause the foreskin to get stuck behind the glans. The glans is the head of the penis. This can cause severe pain and swelling. It's a medical emergency.
- Bleeding. If retraction is forceful, it can cause a small cut. This cut may cause a small amount of bleeding and pain.
- Foreskin Infection. This means an infection under the foreskin. The infection can start in a cut caused by forceful retraction. The main symptom is a red and tender foreskin. Pus may also ooze out to the foreskin opening. Passing urine is painful.
- Urine Retention (Serious). Can't pass urine or just dribbles urine, despite wanting to go.
Causes of Swollen Scrotum
- Torsion of the Testis (Serious). The testicle twists and cuts off its blood supply. It is always painful. Needs to be repaired within 6 to 12 hours to save the testicle. This is why seeing all males with a swollen scrotum is an emergency.
- Hydrocele. Present at birth and both sides usually involved. A hydrocele is a painless sac of fluid sitting on top of the testicle. Present at birth and harmless. It goes away by a year of age.
- Inguinal Hernia. A hernia is a loop of intestine that slides into the scrotum. Any new bulge that comes and goes is a hernia. All hernias need surgery to fix. Most of the time, the repair can be scheduled. If the hernia can't slide back into the abdomen, emergency surgery is needed.
- Varicocele. A clump of swollen veins above the testis, often on the left side. It becomes much smaller after lying down and draining. It is painless. It is also harmless and occurs in 10% of teens.
- Orchitis. This is an infection of the testicle. It is always painful. It's mainly caused by viruses, such as mumps.
- Hematoma (Blood Clot) of Scrotum. Blunt trauma can cause a large blood clot to form inside the scrotum. Sometimes, it needs to be drained. This can happen from being hit by a ball during sports.
When to Call for Penis-Scrotum Symptoms
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Self Care at Home
|
Call Doctor or Seek Care Now
- Scrotum is painful or swollen
- Scrotum changes to a blue or red color
- Severe pain
- Swollen foreskin (child not circumcised)
- Pain or burning when passing urine and fever
- Red rash or red foreskin with fever
- Could be from sexual abuse
- Erection is painful or lasts more than 1 hour
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Call Doctor Within 24 Hours
- Pus or bloody discharge from end of penis
- Pus from end of foreskin (child not circumcised)
- Pain or burning when passing urine, but no fever
- Rash is painful
- Rash has tiny water blisters
- Looks infected (such as draining sore, spreading redness) without fever
- You are worried about a sexually transmitted infection (STI)
- You think your child needs to be seen, but the problem is not urgent
Call Doctor During Office Hours
- Itching lasts more than 3 days
- Small lump or warts
- All other penis or scrotum symptoms. Exception: mild rash for less than 3 days.
- You have other questions or concerns
Self Care at Home
- Mild rash or itching of penis or scrotum present less than 3 days
- Purple head of the penis and healthy child. Reason: this is a normal color.
- Questions about smegma (whitish material) under the foreskin
- Questions about erections in young children
Care Advice
Treatment for Mild Rash or Itching of Penis or Scrotum
-
What You Should Know About Mild Penis or Scrotal Symptoms:
- Rashes can be caused by skin irritants. Hand-to-penis contact is normal when passing urine. Therefore, the rash is most likely from an irritant that was on the hands.
- Examples are a plant (such as an evergreen) or chemicals (such as bug repellents). Fiberglass, pet saliva or even food can also be irritants.
- Most small rashes can be treated at home.
- Here is some care advice that should help.
-
Clean the Area:
- Wash the area once with soap to remove any irritants.
-
Steroid Cream for Itching:
- For itchy rashes, use 1% hydrocortisone cream (such as Cortaid). No prescription is needed.
- Do this 2 times per day for a few days.
-
Antibiotic Ointment for Infection:
- For any cuts, sores or scabs that look infected, put on an antibiotic ointment. An example is Polysporin. No prescription is needed.
- Use 2 times per day until seen.
-
What to Expect:
- Small rashes from irritants should go away in 1 to 2 days with treatment.
-
Prevention of Recurrent Symptoms:
- Teach your son to wash his hands if they are dirty.
- Have him clean his hands before touching his penis.
-
Call Your Doctor If:
- Rash spreads or gets worse
- Rash lasts more than 3 days
- Fever occurs
- You think your child needs to be seen
- Your child becomes worse
Smegma Questions
-
Smegma - General Information:
- Smegma is the small pieces of whitish material found under the foreskin. It can build up under the foreskin. This happens if the foreskin is not pulled back and cleaned regularly. See Foreskin Care Questions care guide.
- Smegma also can occur before the foreskin becomes retractable. It lies under the foreskin that is still stuck to the head of the penis. It can't be removed.
- Smegma is made up of dead skin cells. These cells are shed from the lining of the foreskin and the penis. It becomes trapped under the foreskin.
- Smegma is normal and harmless. It is not a sign of an infection. It is produced in small amounts throughout life.
-
Smegma Before Age 1 Year:
- Sometimes, smegma can be seen through the foreskin. It looks like small whitish lumps.
- If it lies beyond the level of foreskin retraction, it should be left alone.
- Wait until normal separation exposes it.
- During the first year of life, do not make any attempts at foreskin retraction.
Erection Questions
-
Normal Erections
- Erections in boys can occur at any age. They start in the newborn period.
- They tell us the nerves to the penis are working.
- In young boys, some are caused by a full bladder. Most occur without a clear reason.
- In teens, frequent erections start in puberty.
- Normal erections should not cause any pain.
-
Call Your Doctor If:
- Erection lasts over 1 hour
- Erection becomes painful
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.
Pinworms
Is this your child's symptom?
- Tiny, harmless worms that can cause anal itching
- The pinworms live in the colon (large bowel)
Symptoms of Pinworms
- Itching and irritation of the anus and buttocks is the main symptom
- Sometimes, moves to the vagina and causes vaginal itching or discharge
Cause
- A white, very thin, threadlike worm, about ¼ inch (6 mm) long.
- It moves. If it doesn't wiggle, it's probably lint or a thread.
- The worm may be seen around the anus or on the child's bottom. It is especially active at night or early morning.
- Rarely, the pinworm is seen on the surface of a stool.
- The pinworm's secretions are a strong skin irritant and cause the itching.
When to Call for Pinworms
Call Doctor During Office Hours
|
Self Care at Home
|
Call Doctor During Office Hours
- Pinworm is seen. Reason: needs a pinworm medicine.
- Red and tender skin around the anus. Reason: could be Strep infection.
- Anal itching lasts more than 1 week
- You think your child needs to be seen
- You have other questions or concerns
Self Care at Home
- Anal itching without a pinworm being seen
- Questions about pinworm exposure or contact
Care Advice
Treatment for Pinworms
-
What You Should Know About Pinworm Treatment:
- Pinworms are the most common worm infection in the US.
- Pinworms can cause anal itching.
- Pinworms do not carry any diseases.
- Treatment is very helpful.
- Here is some care advice that should help.
-
Pinworm Medicine:
- If a pinworm was seen, your child's doctor will suggest a special pinworm medicine. Pinworm medicines are available without a prescription (such as Reese's Pinworm Medicine). There are also prescription medicines that treat pinworms. Your doctor will decide which one is best for your child. Take as directed.
- Give a repeat dose of the pinworm medicine in 2 weeks. Reason: To prevent the pinworms from coming back.
- The repeat dose is needed because eggs can live for 1 to 2 weeks. Temperature and humidity levels also affect how long the eggs can stay alive.
-
Treating Close Contacts:
- There is a slight risk that Pinworms may spread to others.
- Treat family members only if they have symptoms.
- If another child sleeps with the infected child, they also should be treated.
- If any of your child's friends have symptoms, be sure to tell their parents. These children should get tested or checked for pinworms.
-
Return to School:
- Children with pinworms do not need to miss any child care or school.
-
What to Expect:
- After taking the pinworm medicine, itching should stop in 5 to 7 days.
-
Prevention of Pinworms:
- Wash hands and fingernails well before meals and after using the toilet.
-
Call Your Doctor If:
- Anal symptoms last over 1 week after treatment
- You think your child needs to be seen
- Your child becomes worse
Treatment for Anal Itching Without Pinworm Being Seen
-
What You Should Know About Anal Itching:
- There are many causes of itching around the anus. Some are more common than pinworms.
- The most common cause is stool that has been left on the skin. Stool contains chemicals and germs that can cause itchy skin rashes. Try to prevent this by washing the skin off. After wiping off stool with toilet tissue, cleanse the skin with warm water.
- Bubble bath can also cause an itchy bottom. Children with dry skin are at increased risk. Avoid bubble bath or any soapy bath water.
- If these changes don't get rid of the anal itching, get a pinworm test.
-
Pinworm Checks: Check your child for pinworms.
- Examine the area around the anus, using a flashlight.
- Look for a ¼-inch (6 mm), white, threadlike worm that moves.
- Do this a few hours after your child goes to bed. Check him 2 nights in a row. Also, check him first thing in the morning for 2 days.
-
Scotch Tape Test:
- If no adult pinworm is seen, call your doctor's office. Ask for instructions on doing a Scotch-tape test for pinworm eggs. You can also use the technique below:
- Take a piece of clear Scotch tape with the sticky side down. Touch it to the skin on both sides of the anus. Do this in the morning soon after your child has awakened. Also, do this before any bath or shower.
- Put the sticky tape side that touched the skin on a slide. If you don't have a slide, put it on a second piece of tape.
- Do it 2 mornings in a row.
- Bring the 2 samples in to be looked at under a microscope.
-
Steroid Cream for Itching:
- For the itching, wash the skin around the anus with warm water.
- For severe itch, use 1% hydrocortisone cream (such as Cortaid) 2 times per day. Use for 1 or 2 days. No prescription is needed.
-
Call Your Doctor If:
- Pinworm is seen
- Skin around the anus gets red or tender
- Anal itching lasts more than 1 week
- You think your child needs to be seen
- Your child becomes worse
Treatment for Pinworm Exposure
-
Low Risk for Getting Pinworms:
- Your child has had contact with a child with pinworms, but no symptoms now. Your child probably won't get them. This is especially likely if over a month has passed.
- If contact is within the last month, your child may get pinworms. This risk is small.
- Pinworms are harmless. They are never present very long without being seen or causing anal itching.
-
Scotch Tape Test:
- If you're still worried, call your doctor's office. Ask for instructions on doing a Scotch tape test. This can be done to look for pinworm eggs.
- Do this about 1 month after contact.
- Reason: The swallowed egg will not become an adult pinworm for 3 or 4 weeks.
-
Call Your Doctor If:
- Pinworm is seen (white, ¼ inch or 6 mm, and moves)
- Anal itching lasts more than 1 week
- You think your child needs to be seen
Treatment for Reducing Reinfection or Spread to Others
-
Preventing Pinworm Infections:
- Infection is caused by swallowing pinworm eggs.
- A child can get pinworms no matter how carefully you clean.
- The following hygiene measures, however, can help to reduce the chances of reinfection. It also can reduce the chance of new infections in other people.
- Pets don't carry pinworms.
-
Wash Hands:
- Have your child scrub the hands and fingernails well before each meal. Also, wash the hands well after each use of the toilet.
- Keep the fingernails cut short, because eggs can collect here.
- Help your child give up thumb sucking and nail biting.
-
Shower:
- Each morning give your child a shower.
- Always rinse the anal area.
- Do this for 3 days after taking the pinworm medicine.
-
Vacuum:
- Vacuum or wet-mop your child's bedroom once a week.
- Any eggs left on the floor can still infect others for 1 or 2 weeks.
-
Wash Clothes:
- Wash clothes and bedding at a hot temperature. This will kill any eggs left in them.
-
Return to School:
- Children with pinworms do not need to miss any child care or school.
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.
Poison Ivy - Oak - Sumac
Is this your child's symptom?
- A very itchy rash with blisters
- Caused by contact with the poison ivy plant
If NOT, try one of these:
Symptoms of Poison Ivy
- Rash is shaped like streaks or lines.
- Red streaks with weeping blisters.
- Rash found on exposed body surfaces (such as the hands). Also, can be on areas touched by the hands. Areas that can be affected in this way are the face or genitals.
- Very itchy.
- Onset 1 or 2 days after child was in a forest or field.
Cause
- Caused by oil from poison ivy, poison oak, and poison sumac plants.
- The oil is found in the leaves, stems, berries and roots of the plant.
- Oil may be carried on pet's fur.
- The oil from the plant causes the skin to itch, turn red and blister.
When to Call for Poison Ivy - Oak - Sumac
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Self Care at Home
|
Call Doctor or Seek Care Now
- Fever and looks infected (spreading redness or pus)
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Call Doctor Within 24 Hours
- Looks infected (spreading redness or pus) and no fever
- Swelling is severe (such as the eyes are swollen shut)
- Severe poison ivy reaction in the past
- Rash covers more than one fourth of the body
- Face, eyes, lips or genitals have a rash
- Severe itching (such as can't sleep)
- Big blisters or sores
- Taking oral steroids for more than 24 hours and rash getting worse
- You think your child needs to be seen, but the problem is not urgent
Call Doctor During Office Hours
- Rash lasts more than 3 weeks
- You have other questions or concerns
Self Care at Home
- Mild poison ivy or sumac rash
Care Advice for Mild Poison Ivy
-
What You Should Know About Poison Ivy:
- Poison ivy is caused by skin contact with the oil from the plant.
- The oil can also come from the fur of outdoor pets.
- Most poison ivy rashes can be treated at home.
- Here is some care advice that should help.
-
Steroid Cream for Itching:
- To help with the itch, put 1% hydrocortisone cream (such as Cortaid) on the rash.
- No prescription is needed.
- Use 3 times per day.
-
Cold Soaks for Itching:
- Soak the involved area in cool water for 20 minutes.
- You can also rub the rash with an ice cube.
- Do as often as needed to help the itching and oozing.
-
Allergy Medicine for Itching:
- If itching persists, give an allergy medicine (such as Benadryl) by mouth.
- Use every 6 hours as needed.
- No prescription is needed.
-
Try Not to Scratch:
- Cut the fingernails short.
- Help your child not to scratch.
- Reason: Prevent a skin infection from bacteria.
-
More Poison Ivy - Prevention:
- New blisters may occur several days after the first ones. This means your child probably has ongoing contact with poison ivy oil.
- To prevent it from coming back, bathe all dogs or other pets.
- Wash all clothes and shoes that your child wore on the day of contact.
-
Return to School:
- Poison ivy or oak cannot be spread to others.
- The fluid from the blisters or rash can't cause poison ivy.
- No need to miss any school or child care.
-
What to Expect:
- Most often, the rash lasts 2 weeks.
- Treatment can reduce the severity of symptoms.
- Treatment does not change how long they last.
-
Call Your Doctor If:
- Poison ivy lasts for more than 3 weeks
- It looks infected
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.

The oil contained in the plant leaves irritates the skin.
The redness and blistering from the rash is often arranged in streaks or lines, because the leaf brushes across the body in a line as an individual walks past.

Leaves grouped in threes characterize poison ivy. The scientific name for this plant is Toxicodendron radicans.
Poison Ivy is common in the eastern and central United States

The leaves appear in groups of three.
Poison ivy grows as a small plant, as a bush, or as a vine.
Puncture Wound
Is this your child's symptom?
- The skin is punctured by a pointed narrow object
If NOT, try one of these:
Causes of Puncture Wounds
- Metal: nail, sewing needle, pin, tack
- Pencil: pencil lead is actually graphite (harmless). It is not poisonous lead. Even colored leads are not toxic.
- Wood: toothpick
Complications of Puncture Wounds
- Retained Foreign Object. This happens if part of the sharp object breaks off in the skin. The pain will not go away until it is removed.
- Wound Infection. This happens in 4% of foot punctures. The main symptom is spreading redness 2 or 3 days after the injury.
- Bone Infection. If the sharp object also hits a bone, the bone can become infected. Punctures of the ball of the foot are at greatest risk. The main symptoms are increased swelling and pain 2 weeks after the injury.
When to Call for Puncture Wound
Call 911 Now
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Self Care at Home
|
Call 911 Now
- Deep puncture on the head, neck, chest, back or stomach
- You think your child has a life-threatening emergency
Call Doctor or Seek Care Now
- Puncture into a joint
- Feels like something is still in the wound
- Won't stand (bear weight or walk) on punctured foot
- Needlestick from used needle (may have been exposed to another person's blood)
- Sharp object or setting was very dirty (such as a playground or dirty water)
- No past tetanus shots
- Dirt in the wound is not gone after 15 minutes of scrubbing
- Severe pain and not better 2 hours after taking pain medicine
- Wound looks infected (spreading redness, red streaks)
- Fever occurs
- You think your child has a serious injury
- You think your child needs to be seen, and the problem is urgent
Call Doctor Within 24 Hours
- Last tetanus shot was more than 5 years ago
- You think your child needs to be seen, but the problem is not urgent
Call Doctor During Office Hours
- You have other questions or concerns
Self Care at Home
- Minor puncture wound
Care Advice for Puncture Wound
-
What You Should Know About Puncture Wounds:
- Most puncture wounds do not need to be seen.
- Here is some care advice that should help.
-
Cleaning the Wound:
- First wash off the foot, hand or other punctured skin with soap and water.
- Then soak the puncture wound in warm soapy water for 15 minutes.
- For any dirt or debris, gently scrub the wound surface back and forth. Use a wash cloth to remove any dirt.
- If the wound re-bleeds a little, that may help remove germs.
-
Antibiotic Ointment:
- Use an antibiotic ointment (such as Polysporin). No prescription is needed.
- Then, cover with a bandage (such as Band-Aid). This helps to reduce the risk of infection.
- Re-wash the wound and put on antibiotic ointment every 12 hours.
- Do this for 2 days.
-
Pain Medicine:
- To help with the pain, give an acetaminophen product (such as Tylenol).
- Another choice is an ibuprofen product (such as Advil).
- Use as needed.
-
What to Expect:
- Puncture wounds seal over in 1 to 2 hours.
- Pain should go away within 2 days.
-
Call Your Doctor If:
- Dirt in the wound still there after 15 minutes of scrubbing
- Pain becomes severe
- Looks infected (redness, red streaks, pus, fever)
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.

This photo shows a puncture wound from a BB gun in left upper arm. Note the small hole in the arm where the BB struck and entered the skin.

- Wash the wound with soap and water for 5 minutes.
- Gently scrub out any dirt with a washcloth.
- Cover the wound with a sterile gauze or a clean cloth.
- Apply direct pressure for 10 minutes to stop any bleeding.
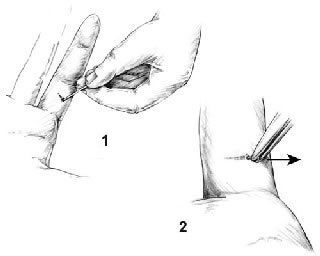
You can remove splinters, larger slivers, and thorns with a needle and tweezers. Check the tweezers beforehand to be certain the ends (pickups) meet exactly. (If they do not, bend them.) Sterilize the tools with rubbing alcohol or a flame.
Clean the skin surrounding the sliver briefly with rubbing alcohol before trying to remove it. Be careful not to push the splinter in deeper. If you don't have rubbing alcohol, use soap and water, but don't soak the area if FB is wood (Reason: can cause swelling of the splinter).
Remove the splinter:
- Step 1: Use the needle to completely expose the large end of the sliver. Use good lighting. A magnifying glass may help.
- Step 2: Then grasp the end firmly with the tweezers and pull it out at the same angle that it went in. Getting a good grip the first time is especially important with slivers that go in perpendicular to the skin or those trapped under the fingernail.
Rash or Redness - Localized
Is this your child's symptom?
- Red or pink rash on one small part of the body (localized)
- Small spots, large spots or solid redness
- Includes redness from skin irritation
If NOT, try one of these:
Causes of Localized Rash or Redness
- Irritants. A rash in just one spot is usually caused by skin contact with an irritant.
- Plants. Many plants cause skin reactions. Sap from evergreens can cause a red area.
- Pollen. Playing in the grass can cause a pink rash on exposed skin.
- Pet Saliva. Some people get a rash where a dog or cat has licked them.
- Food. Some children get a rash if a food is rubbed on the skin. An example could be a fresh fruit. Some babies get hives around the mouth from drooling while eating a new food.
- Chemicals. Many of the products used in the home can be irritating to the skin.
- Insect Bite. Local redness and swelling is a reaction to the insect's saliva. Can be very large without being an allergy. Kids often get mosquito bites without anyone noticing it.
- Bee Sting. Local redness and swelling is a reaction to the bee's venom. Can be very large without being an allergy.
- Cellulitis. This is a bacterial infection of the skin. The main symptom is a red area that keeps spreading. Starts from a break in the skin (such as a scratched insect bite). The red area is painful to the touch.
- Other Common Causes. Look at the "See Other Care Guide" section. 8 rashes that you may be able to recognize are listed there. If you suspect one of them, go there. If not, use this guide.
Localized Versus Widespread Rash: How to Decide
- Localized means the rash occurs on one small part of the body. Usually, the rash is just on one side of the body. An example is a rash on 1 foot. Exceptions: athlete's foot can occur on both feet. Insect bites can be scattered.
- Widespread means the rash occurs on larger areas. Examples are both legs or the entire back. Widespread can also be on most of the body surface. Widespread rashes always occur on matching (both) sides of the body. Many viral rashes are on the chest, stomach and back.
- The cause of a widespread rash usually goes through the blood stream. Examples are rashes caused by viruses, bacteria, toxins, and food or drug allergies.
- The cause of a localized rash usually is just from contact with the skin. Examples are rashes caused by chemicals, allergens, insect bites, ringworm fungus, bacteria or irritants.
- This is why it's important to make this distinction.
Contact Dermatitis
Contact dermatitis is a common cause of a rash in one area. This is especially true of a small rash that will not go away. Contact dermatitis usually starts as raised red spots. It can change to blisters, as in poison ivy. The rash is itchy. Contact dermatitis is an allergic skin rash. The location of the rash may suggest the cause:
- Poison ivy or oak: exposed areas, such as the hands.
- Nickel (metal): anywhere the metal has touched the skin. (Neck from necklaces, earlobe from earrings, or fingers from rings. Stomach from metal snap inside pants, wrist from watch, or face from eyeglass frames.)
- Tanning agents in leather: tops of the feet from shoes or hands from leather gloves
- Preservatives in creams, lotions, cosmetics, sunscreens, shampoos: where applied
- Neomycin in antibiotic ointment: where applied
When to Call for Rash or Redness - Localized
Call 911 Now
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Self Care at Home
|
Call 911 Now
- Not moving or too weak to stand
- You think your child has a life-threatening emergency
Call Doctor or Seek Care Now
- Purple or blood-colored spots or dots that's not from injury or friction
- Age less than 1 month old and tiny water blisters
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Call Doctor Within 24 Hours
- Bright red area or red streak (but not sunburn)
- Rash is very painful
- Fever is present
- Severe itching
- Looks like a boil, infected sore or other infected rash
- Teenager with a rash on the genitals
- Lyme disease suspected (bull's eye rash and tick bite or contact)
- You think your child needs to be seen, but the problem is not urgent
Call Doctor During Office Hours
- Blisters without a clear cause. Exception: Poison Ivy.
- Pimples (Use an antibiotic ointment until seen)
- Rash grouped in a stripe or band
- Peeling fingers
- Rash lasts more than 7 days
- You have other questions or concerns
Self Care at Home
- Mild localized rash or redness
Care Advice for Localized Rashes
-
What You Should Know About Localized Rashes:
- Most new localized rashes are due to skin contact with an irritating substance.
- Here is some care advice that should help.
-
Avoid the Cause:
- Try to find the cause.
- Consider irritants like a plant (such as evergreens or weeds). Also, chemicals (such as solvents or insecticides). Irritants also can include fiberglass or detergents. A new cosmetic or new jewelry (such as nickel) may also be the cause.
- A pet may carry the irritant, as with poison ivy or oak. Also, your child could react directly to pet saliva.
- Review the list of causes for contact dermatitis.
-
Do Not Use Soap:
- Wash the red area once with soap to remove any remaining irritants.
- Then, do not use soaps on it. Reason: Soaps can slow healing.
- Cleanse the area when needed with warm water.
-
Cold Soaks for Itching:
- Use a cold wet washcloth or soak in cold water for 20 minutes.
- Do this every 3 to 4 hours as needed. This will help with itching or pain.
-
Steroid Cream for Itching:
- If the itch is more than mild, use 1% hydrocortisone cream (such as Cortaid). Put it on the rash.
- No prescription is needed.
- Use it 3 times per day.
- Exception: Do not use for suspected ringworm.
-
Try Not to Scratch:
- Help your child not to scratch.
- Cut the fingernails short.
-
Return to School:
- Children with localized rashes do not need to miss any child care or school.
-
What to Expect:
- Most of these rashes go away in 2 to 3 days.
-
Call Your Doctor If:
- Rash spreads or gets worse
- Rash lasts for more than 1 week
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.

This shows a rash that was caused from a nickel allergy. The allergic rash is from the nickel (metal) in the earring. It is red, crusty and moist.

There is redness and puffiness of both cheeks; this is the first sign of Fifth's Disease.

This is a picture of ringworm. The area is round and pink. It has a raised, rough scaly border. The ring slowly grows in size. It is often slightly itchy.
This is caused by a fungus, not a worm. It can be passed from person to person. If you notice a rash like this, contact your doctor for treatment.

This shows impetigo on the face. Impetigo is a skin infection caused by bacteria. The infection causes a red sores which leak fluid. This area will then dry and become crusty as it heals.

This photo shows a red diaper rash in the area under the diaper.
Any diaper rash that lasts longer than a couple days can become infected with yeast. Note the red spots outside the main area of redness.
If a yeast infection is suspected, clotrimazole cream (such as Lotrimin; over-the-counter) should be applied 4 times per day.

This shows a rash that was caused from the skin touching the snap on the jeans. This person is allergic to the nickel in the snap. The area is red and crusty.

This shows a rash that was caused from the skin touching the snap on the jeans. This person is allergic to the nickel in the snap. The area is raised and crusty.
Rash or Redness - Widespread
Is this your child's symptom?
- Red or pink rash over large parts or most of the body (widespread)
- Sometimes, just on hands, feet and buttocks - but same on both sides of body
- Small spots, large spots or solid red skin
If NOT, try one of these:
Causes of Widespread Rash or Redness
- Viral Rash. Most rashes are part of a viral illness. Viral rashes usually have small pink spots. They occur on both sides of the chest, stomach and back. Your child may also have a fever with some diarrhea or cold symptoms. They last 2 or 3 days. More common in the summer.
- Roseola. This is the most common viral rash in the first 3 years of life. (See details below).
- Chickenpox. A viral rash with a distinctive pattern. (see that Care Guide)
- Hand-Foot and-Mouth Disease. A viral rash with a distinctive pattern. It starts with tiny red spots and blisters on the palms and soles. (see that Care Guide)
- Scarlet Fever. Scarlet Fever is a speckled, red rash all over. Caused by the Strep bacteria. Starts on upper chest and quickly spreads to lower chest and stomach. No more serious than a Strep throat infection without a rash.
- Drug Rash. Most rashes that start while taking an antibiotic are viral rashes. Only 10% turn out to be allergic drug rashes. (see details below)
- Hives. Raised pink bumps with pale centers. Hives look like mosquito bites. Rashes that are bumpy and itchy are often hives. Most cases of hives are caused by a virus. Hives can also be an allergic reaction. (See that Care Guide for details)
- Heat Rash. A fine pink rash caused by overheating. Mainly involves neck, chest and upper back.
- Insect Bites. Insect bites cause small red bumps. Flying insects can cause many bumps on exposed skin. Non-flying insects are more likely to cause localized bumps.
- Hot Tub Rash. Causes small red bumps that are painful and itchy. Mainly occurs on skin covered by a bathing suit. Rash starts 12-48 hours after being in hot tub. Caused by overgrowth of bacteria in hot tubs.
- Petechiae Rash (Serious). Petechiae are purple or dark red colored tiny dots. They come from bleeding into the skin. Scattered petechiae with a fever are caused by Meningococcemia until proven otherwise. This is a life-threatening bacterial infection of the bloodstream. Peak age is 3 to 6 months old. Unlike most pink rashes, petechiae don't fade when pressed on.
- Purpura Rash (Serious). Purpura means bleeding into the skin. It looks like purple or dark red larger spots. Widespread purpura is always an emergency. It can be caused by a bacterial bloodstream infection. Rocky Mountain Spotted Fever is an example.
- Blister Rash (Serious). Widespread blisters on the skin are a serious sign. It can be caused by infections or drugs. Stevens Johnson Syndrome is an example.
- Caution. All widespread rashes with fever need to be seen. They need to be diagnosed. Reason: some serious infections that can cause this type of rash.
Drugs and Rashes
- Prescription medicines sometimes cause widespread rashes. Some are allergic, but most are not.
- Non-prescription (OTC) medicines rarely cause any rashes.
- Most rashes that occur while taking an OTC medicine are viral rashes.
- Fever medicines (acetaminophen and ibuprofen) cause the most needless worry. Reason: most viral rashes start with a fever. Hence, the child is taking a fever medicine when the rash starts.
- Drug rashes can't be diagnosed over the phone.
Roseola - A Classic Rash
- Most children get Roseola between 6 months and 3 years of age.
- Rash: pink, small, flat spots on the chest and stomach. Then spreads to the face.
- Classic feature: 2 or 3 days of high fever without a rash or other symptoms.
- The rash starts 12 to 24 hours after the fever goes away.
- The rash lasts 1 to 3 days.
- By the time the rash appears, the child feels fine.
- Treatment: the rash is harmless. Creams or medicines are not needed.
Localized Versus Widespread Rash: How to Decide
- Localized means the rash occurs on one small part of the body. Usually, the rash is just on one side of the body. An example is a rash on 1 foot. Exceptions: athlete's foot can occur on both feet. Insect bites can be scattered.
- Widespread means the rash occurs on larger areas. Examples are both legs or the entire back. Widespread can also mean on most of the body surface. Widespread rashes always occur on matching (both) sides of the body. Many viral rashes are on the chest, stomach and back.
- The cause of a widespread rash usually spreads through the blood stream. Examples are rashes caused by viruses, bacteria, toxins, and food or drug allergies.
- The cause of a localized rash usually is just from contact with the skin. Examples are rashes caused by chemicals, allergens, insect bites, ringworm fungus, bacteria or irritants.
- This is why it's important to make this distinction.
When to Call for Rash or Redness - Widespread
Call 911 Now
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
|
Call 911 Now
- Purple or blood-colored spots or tiny dots with fever within the last 24 hours
- Trouble breathing or swallowing
- Not moving or too weak to stand
- You think your child has a life-threatening emergency
Call Doctor or Seek Care Now
- Purple or blood-colored spots or tiny dots without fever
- Bright red skin that peels off in sheets
- Large blisters on skin
- Bloody crusts on the lips
- Not alert when awake ("out of it")
- Taking a prescription medication within the last 3 days
- Fever
- Your daughter is having her period and using tampons
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Call Doctor Within 24 Hours
- Widespread rash, but none of the symptoms above. Reason: all widespread rashes need to be checked by a doctor.
Care Advice for Widespread Rashes
-
What You Should Know About Widespread Rashes:
- Most rashes with small pink spots all over are part of a viral illness.
- This is more likely if your child has a fever. Other symptoms (like diarrhea) also point to a viral rash.
- Here is some care advice that should help until you talk with your doctor.
-
Non-Itchy Rash Treatment:
- If you suspect a heat rash, give a cool bath.
- Otherwise, no treatment is needed.
-
Itchy Rash Treatment:
- Wash the skin once with soap to remove any irritants.
- Steroid Cream. For relief of itching, use 1% hydrocortisone cream (such as Cortaid). Put it on the most itchy areas. No prescription is needed. Do this 3 times per day.
- Cool Bath. For flare-ups of itching, give your child a cool bath. Do not use soap. Do this for 10 minutes. (Caution: Avoid any chill). Option: Can add 2 ounces (60 mL) of baking soda per tub.
-
Fever Medicine:
- For fevers above 102° F (39° C), give an acetaminophen product (such as Tylenol).
- Another choice is an ibuprofen product (such as Advil).
- Note: Fevers less than 102° F (39° C) are important for fighting infections.
- For all fevers: Keep your child well hydrated. Give lots of cold fluids.
-
Return to School:
- Most viral rashes can be spread to others (especially if a fever is present).
- If your child has a fever, avoid contact with other children. Also, avoid pregnant women until a diagnosis is made.
- For minor rashes, your child can return after the fever is gone.
- For major rashes, your child can return to school after the rash is gone. If your doctor has given medical clearance, your child can return sooner.
-
What to Expect:
- Most viral rashes go away within 48 hours.
-
Call Your Doctor If:
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.

The Chickenpox rash can occur on all body surfaces.
The rash is no longer contagious when all of the spots are crusted over and no new spots are appearing. This usually takes 7 days from the first appearance of the rash.

This child's right hand and wrist displays the characteristic spotted rash of Rocky Mountain spotted fever.
Rocky Mountain spotted fever is the most severe and most frequently reported rickettsial illness in the United States. The disease is caused by the bacteria Rickettsia rickettsii. The disease is spread by ticks.

This child with measles is showing the typical red blotchy rash on his buttocks and back during the 3rd day of the rash.
Measles is an acute, highly contagious viral disease. Symptoms include fever, conjunctivitis (red eyes), runny nose, cough, and spots on the inside cheeks.
A red blotchy rash appears around day 3 of the illness, first on the face, and then becoming generalized.

This patient had a widespread rash from an allergy to penicillin. The picture shows the arm.

This is a simple viral rash in a healthy young boy. The rash was caused by the Echovirus.

The photo shows the typical Scarlet Fever rash on the forearm.
The scarlet fever rash first appears as tiny red bumps on the chest and abdomen that may spread all over the body. Looking like a sunburn, it feels like a rough piece of sandpaper, and lasts about 2-5 days.
Scarlet fever is a disease caused by the same bacteria (Streptococcus) that causes strep throat. A person with Scarlet fever has a throat that is red and sore, usually a fever, usually swollen glands in the neck, and a Scarlet fever rash.

This photo shows a child with Measles.
Measles is an acute, highly contagious viral disease. Symptoms include fever, conjunctivitis (red eyes), runny nose, cough, and spots on the inside cheeks (inside of mouth). A red blotchy rash appears around day 3 of the illness, first on the face, and then becoming more widespread.

Chickenpox is an infectious disease caused by the varicella-zoster virus resulting in an itchy blister-like rash, tiredness and fever.
It appears first on the trunk and face, but can spread over the entire body causing between 250 and 500 itchy blisters.
Reflux (Spitting Up)
Is this your child's symptom?
- Spitting up small amounts of breastmilk or formula. Also called reflux.
- Spitting up 1 or 2 mouthfuls of milk at a time
- No effort or crying
- Normal symptom in half of young babies
If NOT, try one of these:
Symptoms of Spitting Up
- Smaller amounts often occur with burping ("wet burps")
- Larger amounts can occur after overfeeding
- Most often seen during or shortly after feedings
- Occurs mainly in children under 1 year of age
- Begins in the first weeks of life
- Caution: normal reflux does not cause any crying
Complications of Spitting Up (GERD)
- Most infants are "happy spitters." They have normal spitting up (normal reflux).
- If they develop complications, it's called GERD (gastro-esophageal reflux disease).
Symptoms of GERD
GERD problems occur in less than 1% of infants:
- Choking on spit up milk
- Heartburn from acid on lower esophagus. Infants with this problem cry numerous times per day. They also act very unhappy when they are not crying. They are in almost constant discomfort.
- Poor Weight Gain
Cause
- Poor closure of the valve at the upper end of the stomach (weak valve)
- Main trigger: overfeeding of formula or breastmilk
- More than half of all infants have occasional spitting up ("happy spitters")
Reflux Versus Vomiting: How to Tell
- During the first month of life, newborns with true vomiting need to be seen quickly. The causes of vomiting in this age group can be serious. Therefore, it's important to tell the difference between reflux and true vomiting.
Reflux
The following suggests reflux (normal spitting up):
- You've been told by a doctor your baby has reflux
- Onset early in life (85% by 7 days of life)
- Present for several days or weeks
- No pain or crying during reflux
- No effort with spitting up
- No diarrhea
- Your baby acts hungry, looks well and acts happy.
Vomiting
The following suggests vomiting:
- Uncomfortable during vomiting
- New symptom starting today or yesterday
- Forceful vomiting
- Contains bile (green color)
- Diarrhea is also present or
- Your baby looks or acts sick.
Pyloric Stenosis (Serious Cause)
- This is the most common cause of true vomiting in young babies.
- Onset of vomiting age 2 weeks to 2 months
- Vomiting is forceful. It shoots out of the baby's mouth. This is called projectile vomiting.
- Right after vomiting, the baby is hungry and wants to feed. ("hungry vomiter")
- Cause: the pylorus is the channel between the stomach and the gut. In these babies, it becomes narrow and tight.
- Risk: weight loss or dehydration
- Treatment: cured by surgery.
When to Call for Reflux (Spitting Up)
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Self Care at Home
|
Call Doctor or Seek Care Now
- Blood in the spit up
- Bile (green color) in the spit-up
- Choked on milk and turned blue or went limp
- Age less than 12 weeks and spitting up changes to vomiting (forceful or projectile)
- Age less than 1 month old and looks or acts abnormal in any way
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Call Doctor Within 24 Hours
- You think your child needs to be seen, but the problem is not urgent
Call Doctor During Office Hours
- Chokes a lot on milk
- Poor weight gain
- Frequent crying
- Spitting up is getting worse
- Age more than 12 months old
- Spitting up does not get better with this advice
- You have other questions or concerns
Self Care at Home
- Normal reflux (spitting up) with no problems
Care Advice for Spitting Up (Reflux)
-
What You Should Know About Spitting Up:
- Spitting up occurs in most infants (50%).
- Almost always doesn't cause any pain or crying.
- Spitting up does not interfere with normal weight gain.
- Infants with normal reflux do not need any tests or medicines.
- Reflux improves with age.
- Here is some care advice that should help.
-
Feed Smaller Amounts:
- Skip this advice if age less than 1 month or not gaining weight well.
- Bottlefed Babies. Give smaller amounts per feeding (1 ounce or 30 mL less than you have been). Keep the total feeding time to less than 20 minutes. Reason: Overfeeding or completely filling the stomach always makes spitting up worse.
- Breastfed Babies. If you have a good milk supply, try nursing on 1 side per feeding. Pump the other side. Switch sides you start on at each feeding.
-
Longer Time Between Feedings:
- Formula. Wait at least 2½ hours between feedings.
- Breastmilk. Wait at least 2 hours between feedings.
- Reason: It takes that long for the stomach to empty itself. Don't add more milk to a full stomach.
-
Loose Diapers:
- Do not put the diaper on too tight. It puts added pressure on the stomach.
- Don't put pressure on the stomach right after meals.
- Also, do not play too hard with your baby during this time.
-
Upright Position:
- After meals, try to hold your baby in the upright (vertical) position.
- Use a front-pack, backpack, or swing for 30 to 60 minutes after feedings.
- Decrease the time in a sitting position (such as infant seats).
- After 6 months of age, a jumpy seat is helpful. The newer ones are stable.
- During breast or bottle feeds, hold your baby at a slant. Try to keep your baby's head higher than the stomach.
-
Less Pacifier Time:
- Frequent sucking on a pacifier can pump the stomach up with swallowed air.
- So can sucking on a bottle with too small a nipple hole.
- The formula should drip 1 drop per second when held upside down. If it doesn't, the nipple hole may be clogged. Clean the nipple better. You can also make the nipple hole slightly bigger.
-
Burping:
- Burping is less important than giving smaller feedings. You can burp your baby 2 or 3 times during each feeding.
- Do it when he pauses and looks around. Don't interrupt his feeding rhythm in order to burp him.
- Burp each time for less than a minute. Stop even if no burp occurs. Some babies don't need to burp.
-
Add Rice Cereal to Formula:
- If your baby still spits up large amounts, try thickening the formula. Mix it with rice cereal.
- Start with 1 level teaspoon of rice cereal to each ounce of formula.
-
Acid Blocking Medicines:
- Prescription medicines that block acid production are not helpful for normal reflux.
- These medicines also can have side effects.
- They do not reduce excessive crying from colic.
- They are only useful for symptoms of heartburn.
-
What to Expect:
- Reflux gets better with age.
- After learning to sit well, many babies are better by 7 months of age.
-
Call Your Doctor If:
- Spitting up changes to vomiting (forceful or projectile)
- Your baby does not get better with this advice
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.
Ringworm
Is this your child's symptom?
- One or more ring-shaped spots caused by a fungus
- Has a rough edge and clearing of the center
If NOT, try one of these:
Symptoms of Ringworm
- Round pink patch
- Clearing of the center as the patch grows
- Raised, rough, scaly border
- Usually ½ to 1 inch (12 -25 mm) in size
- Ring slowly increases in size
- Often only on one side of the face or body
- Mildly itchy
Cause
- An infection of the skin caused by a fungus. It is not caused by a worm.
- Can often be spread to humans from puppies or kittens that have it. Pet rodents also can carry it.
- Rarely, can be spread human-to-human. It needs direct skin contact to be passed this way. An exception is that ringworm can occur often among wrestlers. This is because of close body contact during matches.
- Sometimes, caused by fungus in the soil.
When to Call for Ringworm
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Self Care at Home
|
Call Doctor Within 24 Hours
- Pus is draining from the rash
Call Doctor During Office Hours
- Scalp is involved
- More than 3 spots are present
- Child is a wrestler
- Rash gets bigger or spreads after 1 week on treatment
- Rash lasts more than 4 weeks
- You think your child needs to be seen
- You have other questions or concerns
Self Care at Home
- Mild ringworm
Care Advice for Ringworm
-
What You Should Know About Ringworm:
- Ringworm is a fungus infection of the skin.
- Often it's caught from puppies or kittens that have it.
- Here is some care advice that should help.
-
Anti-Fungal Cream:
- Use an anti-fungal cream (such as Lotrimin) 2 times per day. No prescription is needed.
- Put it on the rash and 1 inch (2.5 cm) beyond its borders.
- Keep using the cream for at least 7 days after the rash is cleared.
-
Return to School:
- Your child doesn't have to miss any child care or school for ringworm.
- Sometimes, ringworm of the skin can be passed on to others. It requires direct skin-to-skin contact.
- Ringworm from pets is not passed from human to human. It is only passed from animal to human.
- After 48 hours of treatment, ringworm does not spread to others at all.
- Wrestlers: Can return to wrestling after 3 days of treatment. Continue treatment until gone.
-
What to Expect:
- It goes away in 3 to 4 weeks.
- If it comes back, suspect the household puppy or kitten.
- Take your animal to the vet for an exam and treatment.
-
Call Your Doctor If:
- Rash gets bigger or spreads after 1 week on treatment
- Rash is not gone by 4 weeks
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.
Roseola
Is this your child's symptom?
- Widespread fine pink rash caused by Roseola virus
- Classic feature is that the rash is preceded by 2 or 3 days of high fever
- The fever goes away before the rash starts
- A doctor has told you that your child probably has Roseola or
- Rash occurs after several days of fever, but fever gone now
If NOT, try one of these:
Symptoms of Roseola
- Most children get Roseola between 6 months and 3 years of age.
- Rash: Pink, small, flat spots on the chest and stomach. Rash is the same on both sides of the body. Then spreads to the face.
- Classic feature: 2 or 3 days of high fever without a rash or other symptoms.
- The rash starts 12 to 24 hours after the fever goes away.
- The rash lasts 1 to 3 days.
- By the time the rash appears, the child feels fine.
Cause of Roseola
- Human herpes virus 6 (HHV6)
Viral Rashes and Drug Rashes
- Prescription drugs sometimes cause widespread rashes.
- Non-prescription (OTC) drugs rarely cause any rashes.
- Most rashes that occur while taking an OTC drug are viral rashes.
- Fever medicines (acetaminophen and ibuprofen) cause the most confusion. Reason: Most viral rashes start with a fever. Hence, the child is taking a fever med when the rash starts. But, the fever med had nothing to do with the rash.
- Drug rashes can't be diagnosed over the phone.
Prevention
- Good hand washing can prevent spread of infection.
When to Call for Roseola
Call 911 Now
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Self Care at Home
|
Call 911 Now
- You think your child has a life-threatening emergency
Call Doctor or Seek Care Now
- Rash becomes purple or blood-colored
- Large blisters on skin
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Call Doctor Within 24 Hours
- Fever comes back
- Rash becomes worse
- You think your child needs to be seen, but the problem is not urgent
Call Doctor During Office Hours
- Rash lasts more than 4 days
- You have other questions or concerns
Self Care at Home
- Roseola rash
Care Advice for Roseola
-
What You Should Know About Roseola:
- Most children get Roseola between 6 months and 3 years of age.
- It's the most common rash in this age group.
- By the time they get the rash, the fever is gone. The child feels fine.
- The rash is harmless and goes away on its own.
- Here is some care advice that should help.
-
Treatment:
- No treatment is needed.
- Creams or medicines are not helpful.
-
Moisturizing Cream for Itch:
- Roseola usually is not itchy. If your child's rash is itchy, here are some tips.
- Use a moisturizing cream (such as Eucerin) once or twice daily.
- Apply the cream after a 5 or 10-minute bath. (Reason: Water-soaked skin feels less itchy).
- Avoid all soaps. (Reason: Soaps, especially bubble bath, make the skin dry and itchy).
-
Fever Medicine:
- For fevers above 102° F (39° C), give an acetaminophen product (such as Tylenol).
- Another choice is an ibuprofen product (such as Advil).
- Note: Fevers less than 102° F (39° C) are important for fighting infections.
- For all fevers: Keep your child well hydrated. Give lots of cold fluids.
- Note: By the time the rash occurs, the fever should be gone. If your child has both, see Rash or Redness - Widespread care guide.
-
What to Expect:
- Roseola rash goes away in 2-3 days.
- Some children with Roseola just have 3 days of fever without a rash.
-
Return to Child Care:
- Once the rash is gone, the disease is no longer contagious.
- Your child can return to child care or school.
- Children exposed to your child earlier may come down with Roseola in 9-10 days.
-
Call Your Doctor If:
- Fever comes back
- Rash lasts more than 4 days
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.
Scabies
Is this your child's symptom?
- A very itchy rash caused by the scabies mite
- A mite is a tiny, invisible bug that burrows under the skin
- A doctor has told you your child has scabies or
- Your child has had close contact with another person who has it
Symptoms of Scabies
- Widespread little red, bumpy rash that mainly involves the skin folds.
- Intense itching is the main symptom. If it doesn't itch, it's not scabies.
- Appearance. The small red bumps are often in short straight or wavy lines. These are the burrows/tunnels of the mite. The bump or water blister is where the mite entered the skin.
- Location. Classic scabies is found in skin creases such as finger webs. Hands and wrists are the most common sites. Armpits, groin, scrotum, buttocks, navel, waist, and ankles can be involved.
- The face and neck are usually spared. In infants, the rash can involve the face and scalp.
- The rash usually looks the same on both sides of the body.
Cause of Scabies
- Scabies mite
- Scabies comes from skin-to-skin contact with someone who has scabies.
- After contact, a person will come down with scabies rash in 4 to 6 weeks.
- Itching is the first symptom.
- The rash and itching are the body's allergic reaction to mites in the skin.
- Can occur in anyone and does not mean poor hygiene.
- Scabies mites do not carry any disease.
Prevention of Spread to Others
- Scabies is very contagious and prevention is difficult.
- It's best to treat everyone who has had close contact.
When to Call for Scabies
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Self Care at Home
|
Call Doctor or Seek Care Now
- Spreading red area or streak with fever
- Your child looks or acts very sick
Call Doctor Within 24 Hours
- Spreading red area or streak, but no fever
- You think your child needs to be seen
Call Doctor During Office Hours
- Your child had close contact with someone with scabies and not treated
- Yellow soft scab that drains pus or gets bigger, not better with antibiotic ointment
- Severe itching not better after 48 hours of steroid cream and allergy medicine
- Rash goes away with treatment and then returns
- After 4 weeks, itch is still present
- You have other questions or concerns
Self Care at Home
- Scabies infection
Care Advice for Scabies
-
What You Should Know About Scabies:
- Scabies are easy to treat. Itching is the problem.
- The itching normally lasts for 2 weeks after the scabies mites are killed.
- Treatment with the anti-scabies cream does not help the itch.
- The itching is an allergic reaction. The body reacts to the dead mites and eggs in the skin. It continues until all the skin containing the dead mites is shed. This usually takes 2 weeks.
- Continuing to have the itch does not mean that the treatment didn't work. It also doesn't mean that it needs to be repeated.
- Here is some care advice that should help.
-
Treating Close Contacts:
- Scabies is easily spread to others. The symptoms don't start for an average of 30 days.
- Therefore, everyone living in the house should be treated before they develop a rash.
- Close contacts only need to be treated once with the scabies cream.
-
Anti-Scabies Medicine (Prescription):
- Scabies is treated with a prescription cream. (Currently, the most common product is Elimite).
- If applied correctly, it's almost 100% effective at curing scabies.
- Apply the cream from the chin to the toes. Cover every square inch of the body. Don't forget the navel, between the toes, under the fingernails and all the creases.
- Areas that don't seem infected still need to be covered with the cream.
- Caution: Infants less than 1 year old also need the cream applied to the head. Put it on the scalp, forehead, temples, ears and neck. Avoid putting it around the eyes and mouth.
- Bedtime is usually the best time to apply it.
- Eight to 12 hours later give your child a bath with warm water. This will remove the cream.
- One treatment is usually effective. For severe rashes, repeat the treatment 1 week later.
- Approved for as young as 2 months old.
-
Steroid Cream for Itching:
- For relief of itching, apply 1% hydrocortisone cream (such as Cortaid). No prescription is needed.
- Do this 3 times per day to the most itchy spots.
-
Allergy Medicine for Itching:
- For severe itching, an oral allergy medicine (such as Benadryl) should help.
- Age Over 1 Year: Give Benadryl 4 times per day. No prescription is needed.
- Age Over 2 Years: Another option is to give cetirizine (such as Zyrtec) each morning. Use Benadryl at bedtime. No prescription is needed.
-
Cool Baths for Itching:
- For flare-ups of itching, give your child a cool or lukewarm bath. Bathe for 10 minutes.
- Can add baking soda 2 ounces (60 mL) per tub.
- Avoid all soaps. Reason: Soaps make the itching worse.
-
Cut Nails for Itching:
- Discourage scratching.
- Cut the fingernails short. Reason: Prevents a skin infection from bacteria.
-
Cleaning the House:
- Live scabies mites are in clothing your child has worn in the last 3 days.
- Machine wash all your child's sheets, pillowcases, underwear, pajamas, and other recently worn clothing. Use hot water. High dryer temps also kill mites.
- Put items that can't be washed (such as blankets) into plastic bags. You need to keep them in the bags for 4 days to kill the mites. Scabies cannot live off the human skin for more than 3 days.
-
What to Expect:
- One treatment with a prescription anti-scabies cream usually helps. This usually kills all the scabies mites and eggs. Make sure you leave it on for 8-12 hours.
- The rash will heal up and go away in 2 weeks. There shouldn't be any new rash after treatment.
- The itching may last up to 4 weeks. Reason: It's an allergic reaction to the dead scabies.
-
Return to School:
- Your child can return 24 hours after one treatment with the anti-scabies cream.
-
Call Your Doctor If:
- Rash looks infected (draining pus, scabs become larger)
- Itching becomes worse or lasts over 4 weeks
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.
Scrape
Is this your child's symptom?
- Injuries to the skin anywhere on the body surface
- Includes cuts, scratches, scrapes, bruises and swelling
If NOT, try one of these:
Types of Skin Injury
- Cuts, lacerations, gashes and tears. These are wounds that go through the skin to the fat tissue. Caused by a sharp object.
- Scrapes, abrasions, scratches and floor burns. These are surface wounds that don't go all the way through the skin. Scrapes are common on the knees, elbows and palms.
- Bruises. These are bleeding into the skin from damaged blood vessels. Caused by a blunt object. They can occur without a cut or scrape.
When Sutures (Stitches) are Needed for Cuts
- Any cut that is split open or gaping needs sutures.
- Cuts longer than ½ inch (12 mm) usually need sutures.
- On the face, cuts longer than ¼ inch (6 mm) usually need to be seen. They usually need closure with sutures or skin glue.
- Any open wound that may need sutures should be seen as soon as possible. Ideally, they should be checked and closed within 6 hours. Reason: to prevent wound infections. There is no cutoff, however, for treating open wounds.
Cuts Versus Scratches: Helping You Decide
- The skin is about 1/8 inch (3 mm) thick.
- A cut (laceration) goes through it.
- A scratch or scrape (wide scratch) doesn't go through the skin.
- Cuts that gape open at rest or with movement need stitches to prevent scarring.
- Scrapes and scratches never need stitches, no matter how long they are.
- So this distinction is important.
When to Call for Scrape
Call 911 Now
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Self Care at Home
|
Call 911 Now
- Major bleeding that can't be stopped
- Deep cut to chest, stomach, head or neck (such as with a knife)
Call Doctor or Seek Care Now
- Skin is split open or gaping and may need stitches
- Severe pain and not better 2 hours after taking pain medicine
- Age less than 1 year old
- Dirt in the wound is not gone after 15 minutes of scrubbing
- Skin loss from bad scrape goes very deep
- Bad scrape covers large area
- Cut or scrape looks infected (redness, red streak or pus)
- Cut or scrape and no past tetanus shots
- You think your child has a serious injury
- You think your child needs to be seen, and the problem is urgent
Call Doctor Within 24 Hours
- Very large bruise after a minor injury
- Some bruises appear without any known injury
- You think your child needs to be seen, but the problem is not urgent
Call Doctor During Office Hours
- Dirty cut and no tetanus shot in more than 5 years
- Clean cut and no tetanus shot in more than 10 years
- Doesn't heal by 10 days
- You have other questions or concerns
Self Care at Home
- Minor cut, scrape or bruise (minor bleeding that stops)
Care Advice for Minor Cuts, Scrapes or Bruises
-
Cuts, Scratches and Scrapes - Treatment:
- Use direct pressure to stop any bleeding. Do this for 10 minutes or until the bleeding stops.
- Wash the wound with soap and water for 5 minutes. Try to rinse the cut under running water.
- Caution: Never soak a wound that might need sutures. Reason: It may become more swollen and harder to close.
- Gently scrub out any dirt with a washcloth.
- Use an antibiotic ointment (such as Polysporin). No prescription is needed. Then, cover it with a bandage (such as Band-Aid). Change daily.
-
Liquid Skin Bandage for Minor Cuts and Scrapes:
- Liquid skin bandage seals wounds with a plastic coating. It lasts up to 1 week.
- Liquid skin bandage has several benefits compared to other bandages (such as Band-Aid). Liquid bandage only needs to be put on once. It seals the wound and may promote faster healing and lower infection rates. Also, it's water-proof.
- Wash and dry the wound first. Then, put on the liquid. It comes with a brush or swab. It dries in less than a minute.
- You can get this product at a drugstore near you. There are many brands of liquid bandage. No prescription is needed.
-
Bruises - Treatment:
- Use a cold pack or ice bag wrapped in a wet cloth. Put it on the bruise once for 20 minutes. This will help to stop the bleeding.
- After 48 hours, use a warm wet wash cloth. Do this for 10 minutes 3 times per day. This helps to reabsorb the blood.
-
Pain Medicine:
- To help with the pain, give an acetaminophen product (such as Tylenol).
- Another choice is an ibuprofen product (such as Advil).
- Use as needed.
-
Tetanus Shot:
- A tetanus shot update may be needed for cuts and other open wounds.
- Check your vaccine records to see when your child got the last one.
- For Dirty Cuts and Scrapes. If last tetanus shot was given over 5 years ago, need a booster.
- For Clean Cuts. If last tetanus shot was given over 10 years ago, need a booster.
- See your child's doctor for a booster during regular office hours. It's safe to give it within 3 days or less.
-
What to Expect:
- Small cuts and scrapes heal up in less than a week.
-
Call Your Doctor If:
- Bleeding does not stop after using direct pressure to the cut
- Starts to look infected (pus, redness)
- Doesn't heal by 10 days
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.

This bruise is one day old.
Bruises (contusions) result from a direct blow or a crushing injury; there is bleeding into the skin from damaged blood vessels without an overlying cut or abrasion.

This picture shows a shallow abrasion on the left elbow.
First Aid Care Advice for Minor Abrasion:
- Apply direct pressure for 10 minutes to stop any bleeding.
- Wash the abrasion with soap and water.
- Gently scrub out any dirt with a washcloth.
- Apply an antibiotic ointment, covered by a Band-Aid or dressing. Change daily.
- Another option is to use a Liquid Skin Bandage that only needs to be applied once. Avoid ointments with this.

This scalp laceration (cut) is gaping open. It will require closure with sutures or medical staples.
First Aid Care Advice:
- Apply direct pressure for 10 minutes to stop any bleeding.
- Wash the cut with soap and water.

The photo shows 3-4 parallel scratches on the wrist caused by a cat.
First Aid Care Advice:
- Wash the scratches with soap and water.
- Apply an antibiotic ointment twice daily.
- Watch closely for signs of infection, especially the first 1-3 days.

- Wash the wound with soap and water for 5 minutes.
- Gently scrub out any dirt with a washcloth.
- Cover the wound with a sterile gauze or a clean cloth.
- Apply direct pressure for 10 minutes to stop any bleeding.

This abrasion near the elbow occurred 3 days ago. The picture shows an abrasion that is starting to crust over.
There are no signs of infection (e.g., spreading redness, pus).

- Apply direct pressure for 10 minutes to stop any bleeding.
- Wash the wound with soap and water.
- Cover the wound with a sterile gauze or a clean cloth until seen.

This photo shows a gaping laceration (cut) of the chin. It will require closure with either sutures or with skin glue (i.e., Dermabond).
First Aid Care Advice:
- Apply direct pressure for 10 minutes to stop any bleeding.
- Wash the cut with soap and water.
- Cover with a gauze dressing or adhesive bandage (e.g., Band-Aid).

This scalp laceration (cut) is gaping open. It will require closure with sutures or medical staples.
First Aid Care Advice:
- Apply direct pressure for 10 minutes to stop any bleeding.
- Wash the cut with soap and water.

This photo shows a scalp laceration after it has been closed with 4 metal medical staples.

The photograph shows a chin laceration that was closed with skin glue (i.e., Dermabond).
Dermabond (2-octylcyanoacrylate, Ethicon) is a tissue adhesive or "skin glue" which received FDA approval in the United States in 1998. It is used as an alternative to suturing for the repair of simple lacerations. The cosmetic outcome of wounds closed with tissue adhesive is comparable and in some cases superior to suturing.
To apply, the wound edges are held firmly together, and several coats of the glue are painted along the wound margins. The glue dries quickly, within 45-60 seconds. The glue will come off on its own as the wound heals and the top skin layer falls off, usually in about one week.
Sinus Pain or Congestion
Is this your child's symptom?
- Fullness, pressure or pain on the face over a sinus
- Sinus pain occurs above the eyebrow, behind the eye, and under the cheekbone
- Other common symptoms can be a blocked nose, nasal discharge, or postnasal drip
Symptoms
- Most often, the pain or pressure is just on one side of the face.
- Swelling around just one eye.
- Other common symptoms are a stuffy or blocked nose or nasal discharge. Your child may also have a nasal drip down the back of the throat. This is called a postnasal drip.
- Less common symptoms are bad breath or mouth breathing. Also, may have a sore throat and throat clearing from postnasal drip.
- Age Limit. Sinus pain is not a common symptom before 5 years of age.
Causes of Sinus Congestion
- Viral Sinus Infection. Part of the common cold. A cold infects the lining of the nose. It also involves the lining of all the sinuses.
- Bacterial Sinus Infection. A problem when the sinus becomes infected with bacteria. (Occurs in 5% of colds). It starts as a viral sinus infection. Main symptoms are increased sinus pain or return of fever. The skin around the eyelids or cheeks may become red or swollen. Thick nasal secretions that last over 14 days may point to a sinus infection. This can occur in younger children.
- Allergic Sinus Reaction. Sinus congestion often occurs with nasal allergies (such as from pollen). Sneezing, itchy nose and clear nasal discharge point to this cause.
Treatment of Sinus Congestion
- Viral Sinus Infection. Nasal washes with saline. Antibiotics are not helpful.
- Bacterial Sinus Infection. Antibiotics by mouth.
- Allergic Sinus Reaction. Treatment of the nasal allergy with allergy medicines also often helps the sinus symptoms.
- All Thick Nasal Drainage. Nasal secretions need treatment with nasal saline when they block the nose. Also, treat if they make breathing through the nose hard. If breathing is noisy, it may mean the dried mucus is farther back. Nasal saline rinses can remove it.
Color of Nasal Discharge with Colds
- The nasal discharge changes color during different stages of a cold. This is normal.
- It starts as a clear discharge and later becomes cloudy.
- Sometimes it becomes yellow or green colored for a few days. This is still normal.
- Colored discharge is common after sleep, with allergy medicines or with low humidity. Reason: all of these events decrease the amount of normal nasal secretions.
Bacterial Sinus Infections: When to Suspect
- Yellow or green nasal discharge is seen with both viral and bacterial sinus infections. Suspect a bacterial infection if the discharge becomes thick (like pus). But, it also needs one or more of these symptoms:
- Sinus Pain, not just normal sinus congestion. Pain occurs mainly behind the cheekbone or eye or
- Swelling or redness of the skin over any sinus or
- Fever lasts more than 3 days or
- Fever returns after it's been gone for over 24 hours or
- Nasal discharge and post-nasal drip lasts over 14 days without improvement
When to Call for Sinus Pain or Congestion
Call 911 Now
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Self Care at Home
|
Call 911 Now
- Not moving or too weak to stand
- Severe trouble breathing (struggling for each breath, can barely speak or cry)
- You think your child has a life-threatening emergency
Call Doctor or Seek Care Now
- Trouble breathing not gone after cleaning out the nose
- Redness or swelling on the cheek, forehead or around the eye
- Severe pain and not better after using care advice
- Weak immune system. Examples are: sickle cell disease, HIV, cancer, organ transplant, taking oral steroids.
- Fever over 104° F (40° C)
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Call Doctor Within 24 Hours
- Headache lasts more than 48 hours
- Fever lasts more than 3 days
- Fever returns after being gone more than 24 hours
- Earache occurs
- Sinus pain (not just pressure) and fever
- You think your child needs to be seen, but the problem is not urgent
Call Doctor During Office Hours
- Sinus pain (not just pressure or fullness) lasts more than 24 hours, after using nasal washes
- Thick yellow or green pus draining from nose and not improved by nasal washes. Exception: yellow or green tinged secretions are normal.
- Sinus congestion and fullness lasts more than 2 weeks
- Nasal discharge lasts more than 2 weeks
- You have other questions or concerns
Self Care at Home
- Normal sinus congestion as part of a cold
Care Advice for Sinus Congestion
-
What You Should Know About Sinus Congestion:
- Sinus congestion is a normal part of a cold.
- Nasal discharge normally changes color during different stages of a cold. It starts as clear, then cloudy, turns yellow-green tinged, then dries up.
- Yellow or green-tinged discharge. This is more common with sleep, antihistamines or low humidity. (Reason: decrease the amount of normal nasal secretions.)
- Usually, nasal washes can prevent a bacterial sinus infection.
- Antibiotics are not helpful for the sinus congestion that occurs with colds.
- Here is some care advice that should help.
-
Nasal Saline to Open a Blocked Nose:
- Use saline (salt water) nose spray (such as store brand). This helps to loosen up the dried mucus. If you don't have saline, you can use a few drops of water. Use bottled water, distilled water or boiled tap water. Teens can just splash a little water in the nose and then blow.
- Step 1: Put 3 drops in each nostril.
- Step 2: Blow each nostril out while closing off the other nostril. Then, do the other side.
- Step 3: Repeat nose drops and blowing until the discharge is clear.
- How often: Do saline rinses when your child can't breathe through the nose.
- Saline nose drops or spray can be bought in any drugstore. No prescription is needed.
- Saline nose drops can also be made at home. Use ½ teaspoon (2 mL) of table salt. Stir the salt into 1 cup (8 ounces or 240 mL) of warm water. Use bottled water or boiled water to make saline nose drops.
- Reason for nose drops: Suction or blowing alone can't remove dried or sticky mucus.
- Other option: use a warm shower to loosen mucus. Breathe in the moist air, then blow each nostril.
-
Fluids - Offer More:
- Try to get your child to drink lots of fluids.
- Goal: Keep your child well hydrated.
- It also will thin out the mucus discharge from the nose.
- It also loosens up any phlegm in the lungs. Then it's easier to cough up.
-
Humidifier:
- If the air in your home is dry, use a humidifier. Reason: Dry air makes nasal mucus thicker.
-
Decongestant Nose Spray (Age 12 years or Older):
- Use this only if the sinus still seems blocked up after nasal washes. Use the long-acting type (such as Afrin).
- Dose: 1 spray on each side. Do this 2 times per day.
- Always clean out the nose before using.
- Use for 1 day. After that, use only for symptoms.
- Don't use for more than 3 days. (Reason: Can cause rebound congestion).
- Decongestants given by mouth (such as Sudafed) are another choice. They can also open a stuffy nose and ears. Side effects: They may make a person feel nervous or dizzy. Follow the package directions.
-
Pain Medicine:
- To help with the pain, give an acetaminophen product (such as Tylenol).
- Another choice is an ibuprofen product (such as Advil).
- Use as needed.
-
Cold Pack for Pain:
- For pain or swelling, use a cold pack. You can also use ice wrapped in a wet cloth.
- Put it over the sinus for 20 minutes.
- Caution: Avoid frostbite.
-
Allergy Medicine:
- If the child also has nasal allergies, give an allergy medicine.
- Long-acting allergy medicines (such as Zyrtec) are a good first choice. Other options are Allegra or Claritin. Reason: these meds do not cause your child to act sleepy.
- Benadryl can be used if these products do not control symptoms.
- No prescription is needed.
-
What to Expect:
- With this advice, the viral sinus blockage goes away in 7 to 14 days.
- The main problem is a sinus infection from bacteria. This can occur if bacteria multiply within the blocked sinus. This leads to a fever and increased pain. It needs antibiotics. Once on treatment, the symptoms will improve in a few days.
-
Return to School:
- Sinus infections cannot be spread to others.
- Your child can return to school after the fever is gone. Your child should feel well enough to join in normal activities.
-
Call Your Doctor If:
- Sinus pain lasts more than 24 hours after starting treatment
- Sinus congestion lasts more than 2 weeks
- Fever lasts more than 3 days
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.
Skin Injury
Is this your child's symptom?
- Injuries to the skin anywhere on the body surface
- Includes cuts, scratches, scrapes, bruises and swelling
If NOT, try one of these:
Types of Skin Injury
- Cuts, lacerations, gashes and tears. These are wounds that go through the skin to the fat tissue. Caused by a sharp object.
- Scrapes, abrasions, scratches and floor burns. These are surface wounds that don't go all the way through the skin. Scrapes are common on the knees, elbows and palms.
- Bruises. These are bleeding into the skin from damaged blood vessels. Caused by a blunt object. They can occur without a cut or scrape.
When Sutures (Stitches) are Needed for Cuts
- Any cut that is split open or gaping needs sutures.
- Cuts longer than ½ inch (12 mm) usually need sutures.
- On the face, cuts longer than ¼ inch (6 mm) usually need to be seen. They usually need closure with sutures or skin glue.
- Any open wound that may need sutures should be seen as soon as possible. Ideally, they should be checked and closed within 6 hours. Reason: to prevent wound infections. There is no cutoff, however, for treating open wounds.
Cuts Versus Scratches: Helping You Decide
- The skin is about 1/8 inch (3 mm) thick.
- A cut (laceration) goes through it.
- A scratch or scrape (wide scratch) doesn't go through the skin.
- Cuts that gape open at rest or with movement need stitches to prevent scarring.
- Scrapes and scratches never need stitches, no matter how long they are.
- So this distinction is important.
When to Call for Skin Injury
Call 911 Now
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Self Care at Home
|
Call 911 Now
- Major bleeding that can't be stopped
- Deep cut to chest, stomach, head or neck (such as with a knife)
Call Doctor or Seek Care Now
- Skin is split open or gaping and may need stitches
- Severe pain and not better 2 hours after taking pain medicine
- Age less than 1 year old
- Dirt in the wound is not gone after 15 minutes of scrubbing
- Skin loss from bad scrape goes very deep
- Bad scrape covers large area
- Cut or scrape looks infected (redness, red streak or pus)
- Cut or scrape and no past tetanus shots
- You think your child has a serious injury
- You think your child needs to be seen, and the problem is urgent
Call Doctor Within 24 Hours
- Very large bruise after a minor injury
- Some bruises appear without any known injury
- You think your child needs to be seen, but the problem is not urgent
Call Doctor During Office Hours
- Dirty cut and no tetanus shot in more than 5 years
- Clean cut and no tetanus shot in more than 10 years
- Doesn't heal by 10 days
- You have other questions or concerns
Self Care at Home
- Minor cut, scrape or bruise (minor bleeding that stops)
Care Advice for Minor Cuts, Scrapes or Bruises
-
Cuts, Scratches and Scrapes - Treatment:
- Use direct pressure to stop any bleeding. Do this for 10 minutes or until the bleeding stops.
- Wash the wound with soap and water for 5 minutes. Try to rinse the cut under running water.
- Caution: Never soak a wound that might need sutures. Reason: It may become more swollen and harder to close.
- Gently scrub out any dirt with a washcloth.
- Use an antibiotic ointment (such as Polysporin). No prescription is needed. Then, cover it with a bandage (such as Band-Aid). Change daily.
-
Liquid Skin Bandage for Minor Cuts and Scrapes:
- Liquid skin bandage seals wounds with a plastic coating. It lasts up to 1 week.
- Liquid skin bandage has several benefits compared to other bandages (such as Band-Aid). Liquid bandage only needs to be put on once. It seals the wound and may promote faster healing and lower infection rates. Also, it's water-proof.
- Wash and dry the wound first. Then, put on the liquid. It comes with a brush or swab. It dries in less than a minute.
- You can get this product at a drugstore near you. There are many brands of liquid bandage. No prescription is needed.
-
Bruises - Treatment:
- Use a cold pack or ice bag wrapped in a wet cloth. Put it on the bruise once for 20 minutes. This will help to stop the bleeding.
- After 48 hours, use a warm wet wash cloth. Do this for 10 minutes 3 times per day. This helps to reabsorb the blood.
-
Pain Medicine:
- To help with the pain, give an acetaminophen product (such as Tylenol).
- Another choice is an ibuprofen product (such as Advil).
- Use as needed.
-
Tetanus Shot:
- A tetanus shot update may be needed for cuts and other open wounds.
- Check your vaccine records to see when your child got the last one.
- For Dirty Cuts and Scrapes. If last tetanus shot was given over 5 years ago, need a booster.
- For Clean Cuts. If last tetanus shot was given over 10 years ago, need a booster.
- See your child's doctor for a booster during regular office hours. It's safe to give it within 3 days or less.
-
What to Expect:
- Small cuts and scrapes heal up in less than a week.
-
Call Your Doctor If:
- Bleeding does not stop after using direct pressure to the cut
- Starts to look infected (pus, redness)
- Doesn't heal by 10 days
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.

This bruise is one day old.
Bruises (contusions) result from a direct blow or a crushing injury; there is bleeding into the skin from damaged blood vessels without an overlying cut or abrasion.

This picture shows a shallow abrasion on the left elbow.
First Aid Care Advice for Minor Abrasion:
- Apply direct pressure for 10 minutes to stop any bleeding.
- Wash the abrasion with soap and water.
- Gently scrub out any dirt with a washcloth.
- Apply an antibiotic ointment, covered by a Band-Aid or dressing. Change daily.
- Another option is to use a Liquid Skin Bandage that only needs to be applied once. Avoid ointments with this.

This scalp laceration (cut) is gaping open. It will require closure with sutures or medical staples.
First Aid Care Advice:
- Apply direct pressure for 10 minutes to stop any bleeding.
- Wash the cut with soap and water.

The photo shows 3-4 parallel scratches on the wrist caused by a cat.
First Aid Care Advice:
- Wash the scratches with soap and water.
- Apply an antibiotic ointment twice daily.
- Watch closely for signs of infection, especially the first 1-3 days.

- Wash the wound with soap and water for 5 minutes.
- Gently scrub out any dirt with a washcloth.
- Cover the wound with a sterile gauze or a clean cloth.
- Apply direct pressure for 10 minutes to stop any bleeding.

This abrasion near the elbow occurred 3 days ago. The picture shows an abrasion that is starting to crust over.
There are no signs of infection (e.g., spreading redness, pus).

- Apply direct pressure for 10 minutes to stop any bleeding.
- Wash the wound with soap and water.
- Cover the wound with a sterile gauze or a clean cloth until seen.

This photo shows a gaping laceration (cut) of the chin. It will require closure with either sutures or with skin glue (i.e., Dermabond).
First Aid Care Advice:
- Apply direct pressure for 10 minutes to stop any bleeding.
- Wash the cut with soap and water.
- Cover with a gauze dressing or adhesive bandage (e.g., Band-Aid).

This scalp laceration (cut) is gaping open. It will require closure with sutures or medical staples.
First Aid Care Advice:
- Apply direct pressure for 10 minutes to stop any bleeding.
- Wash the cut with soap and water.

This photo shows a scalp laceration after it has been closed with 4 metal medical staples.

The photograph shows a chin laceration that was closed with skin glue (i.e., Dermabond).
Dermabond (2-octylcyanoacrylate, Ethicon) is a tissue adhesive or "skin glue" which received FDA approval in the United States in 1998. It is used as an alternative to suturing for the repair of simple lacerations. The cosmetic outcome of wounds closed with tissue adhesive is comparable and in some cases superior to suturing.
To apply, the wound edges are held firmly together, and several coats of the glue are painted along the wound margins. The glue dries quickly, within 45-60 seconds. The glue will come off on its own as the wound heals and the top skin layer falls off, usually in about one week.
Skin Lump
Is this your child's symptom?
- A skin lump or bump covered by normal skin
- Skin swelling just in one spot (localized) is also included
If NOT, try one of these:
Causes of Skin Lumps
- Insect Bites. The most common cause of an itchy bump is a mosquito bite. Other insects can also cause little bumps.
- Stings. A bee sting can cause a painful bump. The swelling can become quite large.
- Lymph Nodes. Most common cause of a lump or mass felt under the skin. Commonly found in the neck or groin. Nodes have a boundary or edge and are movable. This is not the case for the swelling seen with insect bites. Lymph nodes become larger with infections.
- Scalp Hematoma. The most common cause of a lump on the head is a scalp hematoma (goose egg). In a child under 2 years of age the injury may not have been seen.
- Injuries. New lumps anywhere can be caused by an injury that wasn't observed. A bruise is often present with the swelling.
- Callus. Broken bones heal with new bone formation. The medical term is callus. The callus feels like a bony knot that is larger than the bone itself. A callus is most commonly felt after a collarbone fracture.
- Boils. A boil is a skin abscess. It causes a very painful red lump.
Lumps that are a Normal Part of the Body
- Breast Bud. A small disc-shaped lump felt under the nipple. It indicates the onset of puberty in 7-12 year old girls.
- External Occipital Protuberance. The bony lump felt at the base of the skull in back.
- Mastoid Process. The bony lump felt behind each lower ear.
- Xiphoid Process. A small hard lump felt at the lower end of the sternum (breastbone).
Common Objects Used to Guess the Size
- Pea or pencil eraser: ¼ inch or 6 mm
- Dime: ¾ inch or 1.8 cm
- Quarter: 1 inch or 2.5 cm
- Golf ball: 1 ½ inches or 3.8 cm
- Tennis Ball: 2 ½ inches or 6.4 cm
When to Call for Skin Lump
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Self Care at Home
|
Call Doctor or Seek Care Now
- Redness spreading from the lump with fever
- Groin swelling and painful
- Age less than 12 months and on scalp. Exception: normal bump in back at base of skull.
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Call Doctor Within 24 Hours
- Redness spreading from the lump without fever
- Boil suspected (painful, non-itchy, red lump)
- Age 12 months or older and on scalp. Exception: normal bump in back at base of skull.
- Can't move nearest joint normally (bend and straighten completely)
- Swelling is painful and cause not known
- You think your child needs to be seen, but the problem is not urgent
Call Doctor During Office Hours
- Large lump more than 1 inch (2.5 cm) and cause not known
- Small lump lasts more than 7 days and cause not known
- You have other questions or concerns
Self Care at Home
- Small lump present 7 days or less and cause not known. Reasonprobably due to insect bite not observed.
- Breast bud - normal lump under the nipple
- External occipital protuberance - normal lump on back of head
- Mastoid process - normal lump behind each lower ear
- Xiphoid process - normal lump at bottom of breastbone
Care Advice
Treatment for a Small Lump or Swelling
-
What You Should Know:
- Most new swellings are due to insect bites. Mosquito bites account for 90% of them. Your child may not even know that he got bit.
- Suspect an insect bite if there are bites on other parts of the body.
- While most insect bites cause a small red bump, some are larger (like a hive).
- This does not mean your child has an allergy or the bite is infected.
- Here is some care advice that should help.
-
Cold Pack for Swelling:
- Apply a cold pack or cold wet washcloth for 20 minutes.
-
Steroid Cream for Itching:
- If the swelling is itchy, use 1% hydrocortisone cream (such as Cortaid). No prescription is needed.
- Do this 3 times per day.
-
Allergy Medicine for Itching or Swelling:
- For severe itch or swelling, give an allergy medicine by mouth. No prescription is needed.
- Benadryl is best. Repeat every 6 hours as needed.
- If you only have another allergy medicine at home (but not Benadryl), use that. Follow the package directions.
-
What to Expect:
- Most insect bites itch or hurt for 1 or 2 days.
- The swelling usually peaks in 2 days, but may last a week.
- If the swelling becomes larger or doesn't go away, it needs to be examined.
-
Call Your Doctor If:
- Swelling becomes very painful
- Fever occurs
- Swelling becomes large (over 1 inch or 2.5 cm)
- Swelling lasts over 7 days
- You think your child needs to be seen
- Your child becomes worse
Lumps that are a Normal Part of the Body
-
Breast Buds - Normal Lump Under the Nipple:
- Breast buds are normal, small disc-shaped rubbery lumps felt under the nipple.
- Age. They normally occur in 8-12 year old girls and are the first sign of puberty. Sometimes, they are even normal in 7 year olds.
- One Side. They sometimes start just on one side. Don't worry about that. Within 2 or 3 months, a breast bud will also appear on the other side.
- Importance. The entire breast develops entirely from the breast bud, taking 2 or 3 years to completion.
- Symptoms. Breast buds normally can be somewhat tender.
- Caution: Never squeeze or massage breast buds. Reason: Can cause a serious infection.
- Risks. None. Breast buds have no risk of turning into cancer.
- Follow-up. You can have your child's doctor check the breast bud during the next regular office visit.
-
External Occipital Protuberance - Normal Lump on Back of Head:
- The lump you feel at the base of the skull in back is normal. It is a bony part of the skull that sticks out and feels hard.
- If you feel carefully, you will find one on yourself or other children.
- This is not caused by any injury.
-
Mastoid Process - Normal Lump Behind the Ear:
- The mastoid process is a bony lump you can feel behind the lower ear.
- Muscles that turn the neck attach to the mastoid process.
- The process is larger in men because of larger neck muscles.
- The mastoid is filled with air cells that connect to the inner ear.
-
Xiphoid Process - Normal Lump at Bottom of Breastbone:
- The small hard lump at the lower end of the sternum (breastbone) is normal. It is called the xiphoid process. You can feel it.
- It is more prominent in babies and slender children. Sometimes, it's more visible when breathing in.
- If you feel carefully, you will find one on yourself or other children.
- It's made of cartilage, but turns to bone in adults.
-
Call Your Doctor If:
- You have other questions or concerns
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.
Sliver or Splinter
Is this your child's symptom?
- A foreign object stuck in the skin
- Some examples are a wood splinter, fishhook, glass sliver or needle
Symptoms of a Foreign Object in the Skin
- Pain. Most tiny slivers in the top layer of skin do not cause much pain. An example of these tiny slivers is plant stickers. Objects that are deeper or go straight down are usually painful to pressure. Objects in the foot are very painful with standing or walking.
- Foreign Object Sensation. Older children may complain about something being in the skin. ("I feel something in there.")
Types of Foreign Bodies (Objects)
- Wood (Organic): splinters, cactus spines, thorns, toothpicks. These objects are irritating and become infected if not removed.
- Metallic: BBs, nails, sewing needles, pins, tacks
- Fiberglass slivers
- Fishhooks may have a barbed point that makes removal difficult
- Glass sliver
- Pencil lead (graphite, not lead)
- Plastic sliver
When to Call for Sliver or Splinter
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Self Care at Home
|
Call Doctor or Seek Care Now
- Object has a barb (such as a fish hook)
- Object is a BB
- Object is causing severe pain
- You want a doctor to take out the object
- You tried and can't get the object out
- Wound looks infected (spreading redness)
- Fever occurs
- You think your child has a serious injury
- You think your child needs to be seen, and the problem is urgent
Call Doctor Within 24 Hours
- Deep puncture wound and last tetanus shot was more than 5 years ago
- You think your child needs to be seen, but the problem is not urgent
Call Doctor During Office Hours
- You have other questions or concerns
Self Care at Home
- Tiny, pain-free slivers near the surface that don't need to be removed
- Tiny plant or cactus spines or fiberglass slivers that need to be removed
- Minor sliver, splinter or thorn that needs removal. You think you can do it at home.
Care Advice for Minor Slivers and Splinters
-
Tiny, Pain-Free Slivers - Treatment:
- Tiny, pain-free slivers near the skin surface can be left in.
- They will slowly work their way out with normal shedding of the skin.
- Sometimes, the body also will reject them by forming a little pimple. This will drain on its own. Or you can open up the pimple. Use a clean needle. The sliver will flow out with the pus.
-
Tiny Painful Plant Stickers - Treatment:
- Plant stickers or cactus spines are hard to remove. Fiberglass slivers may also be hard to get out. Reason: They are fragile. Most often, they break when pressure is applied with a tweezers.
- Tape. First, try touching the spot lightly with tape. The stickers should attach to the tape. You can use packaging tape, duct tape or another very sticky tape.
- Wax Hair Remover. If tape doesn't work, use wax hair remover. Put a thin layer on. Let it air dry for 5 minutes. You can also speed up the process with a hair dryer. Then peel it off with the stickers. Most will be removed. The others will usually work themselves out with normal shedding of the skin.
-
Needle and Tweezers for Slivers and Splinters:
- For larger splinters, slivers or thorns, remove with a needle and tweezers.
- Check the tweezers first. Be certain the ends (pickups) meet exactly. If they do not, bend them. Clean the tool with rubbing alcohol before using them.
- Clean the skin around the sliver briefly with rubbing alcohol. Do this before trying to remove it. If you don't have any, use soap and water. Caution: Don't soak the spot if the foreign object is wood. Reason: can cause swelling of the splinter.
- Use the needle to uncover the large end of the sliver. Use good lighting. A magnifying glass may help.
- Grasp the end firmly with the tweezers. Pull it out at the same angle that it went in. Get a good grip the first time. This is important for slivers that go straight into the skin. This is also important for those trapped under the fingernail.
- For slivers under a fingernail, sometimes part of the nail must be cut away. Use a fine scissors to expose the end of the sliver.
- Slivers (where you can see all of it) often can be removed at home. Pull on the end. If the end breaks off, open the skin with a sterile needle. Go along the length of the sliver and flick it out.
-
Antibiotic Ointment:
- Wash the area with soap and water before and after removal.
- Use an antibiotic ointment (such as Polysporin) once after sliver is taken out. No prescription is needed. This will help to decrease the risk of infection.
-
Call Your Doctor If:
- You can't get the object out
- Object is out, but pain gets worse
- Starts to look infected
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.
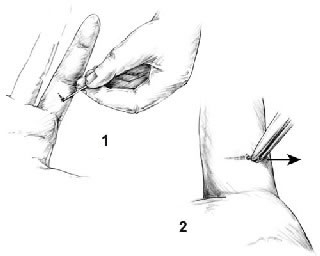
You can remove splinters, larger slivers, and thorns with a needle and tweezers. Check the tweezers beforehand to be certain the ends (pickups) meet exactly. (If they do not, bend them.) Sterilize the tools with rubbing alcohol or a flame.
Clean the skin surrounding the sliver briefly with rubbing alcohol before trying to remove it. Be careful not to push the splinter in deeper. If you don't have rubbing alcohol, use soap and water, but don't soak the area if FB is wood (Reason: can cause swelling of the splinter).
Remove the splinter:
- Step 1: Use the needle to completely expose the large end of the sliver. Use good lighting. A magnifying glass may help.
- Step 2: Then grasp the end firmly with the tweezers and pull it out at the same angle that it went in. Getting a good grip the first time is especially important with slivers that go in perpendicular to the skin or those trapped under the fingernail.
Sore Throat
Is this your child's symptom?
- Pain or discomfort of the throat
- Made worse when swallows
- Rare symptom before 2 years old
- Not caused by an injury to the throat
If Sore Throat occurs with a Cold, see
Causes of Sore Throat
- Colds. Most sore throats are part of a cold. In fact, a sore throat may be the only symptom for the first 24 hours. Then a cough and runny nose occur.
- Viral Pharyngitis. Some viruses cause a sore throat without other symptoms. A cough and runny nose don't become part of the illness. An antibiotic won't help.
- Strep Pharyngitis. Group A Strep is the most common bacterial cause. It accounts for 20% of sore throats without any cold symptoms. Pus is seen on the tonsils. Peak age is 5 to 15 years. An antibiotic is helpful.
- Mono. Infectious Mono mainly occurs in teens and young adults. The main symptoms are sore throat, fever and widespread swollen lymph nodes. Like Strep, Mono also has pus on the tonsils. Patients with Mono also may have a large spleen. It's located in the upper left side of the stomach. Mono is diagnosed with special blood tests.
- Post-nasal Drip. Drainage from a sinus infection can cause a sore throat. The throat clearing that goes with the drainage may cause most of the irritation. The sinus infection is more likely to be viral than bacterial.
- Mouth Breathing. Breathing with the mouth open during sleep can cause a sore throat. After eating breakfast, it often goes away.
- Abscess of Tonsil (Serious). A bacterial infection of the tonsil can spread to the surrounding tissues. The main symptoms are severe trouble swallowing, fever and one-sided throat pain. It's also hard to fully open the mouth. The peak age is teens.
- Epiglottitis (Very Serious). A bacterial infection of the flap of tissue above the vocal cords. It normally covers the windpipe during swallowing. The main symptoms are severe sore throat, drooling, spitting and fever. It can shut off the airway. Needs a 911 response.
Strep Throat: When to Suspect
- Symptoms include sore throat, fever, headache, stomach pain, nausea and vomiting.
- Cough, hoarseness, red eyes, and runny nose are usually not seen with Strep throat. These symptoms point more to a viral cause.
- Scarlet fever rash (fine, red, sandpaper-like rash) is highly suggestive of Strep throat.
- Peak age: 5 to 15 years old. Not common under 2 years old unless sibling has Strep.
- If you think your child has Strep, call your doctor.
- Your doctor will do a Strep test. If the test is positive, they will start treatment. There is no risk from waiting until a Strep test can be done.
- Standard treatment is with antibiotics by mouth.
Symptoms in Infants and Toddlers
- Children less than 2 years of age usually don't complain about a sore throat. A young child who does not want favorite foods may have a sore throat. They may also start to cry during feedings. Their symptoms are usually better covered using Drinking Fluids - Decreased care guide.
When to Call for Sore Throat
Call 911 Now
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Self Care at Home
|
Call 911 Now
- Severe trouble breathing (struggling for each breath, can barely speak or cry)
- You think your child has a life-threatening emergency
Call Doctor or Seek Care Now
- Trouble breathing, but not severe
- Great trouble swallowing fluids or spit
- Can't open mouth all the way
- Stiff neck or can't move neck like normal
- Dehydration suspected. No urine in more than 8 hours, dark urine, very dry mouth and no tears.
- Purple or blood-colored spots or dots on skin
- Weak immune system. Examples are: sickle cell disease, HIV, cancer, organ transplant, taking oral steroids.
- Fever over 104° F (40° C)
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent. Note: a Strep test alone is not urgent.
Call Doctor Within 24 Hours
- Sore throat pain is severe and not better 2 hours after taking ibuprofen
- Large lymph nodes in the neck
- Pink rash that's widespread
- Earache or ear drainage
- Sinus pain (not just congestion) around cheekbone or eyes
- Fever lasts more than 3 days
- Fever returns after being gone more than 24 hours
- Age less than 2 years old
- Close contact to a person with Strep within last 7 days
- Sores on the skin
- You think your child needs to be seen, but the problem is not urgent (or needs a Strep test)
Call Doctor During Office Hours
- Sore throat is the main symptom and lasts more than 48 hours
- Sore throat with cold/cough symptoms lasts more than 5 days
- You have other questions or concerns
Self Care at Home
- Viral throat infection suspected
Care Advice for Sore Throats
-
What You Should Know About Sore Throats:
- Most sore throats are just part of a cold and caused by a virus.
- A cough, hoarse voice or nasal discharge points to a cold as the cause.
- Most children with a sore throat don't need to see their doctor.
- Here is some care advice that should help.
-
Sore Throat Pain Relief:
- Age over 1 year. Can sip warm fluids such as chicken broth or apple juice. Some children prefer cold foods such as popsicles or ice cream.
- Age over 6 years. Can also suck on hard candy or lollipops. Butterscotch seems to help.
- Age over 8 years. Can also gargle. Use warm water with a little table salt added. A liquid antacid can be added instead of salt. Use Mylanta or the store brand. No prescription is needed.
- Medicated throat sprays or lozenges are generally not helpful.
-
Pain Medicine:
- To help with the pain, give an acetaminophen product (such as Tylenol).
- Another choice is an ibuprofen product (such as Advil).
- Use as needed.
-
Fever Medicine:
- For fevers above 102° F (39° C), give an acetaminophen product (such as Tylenol).
- Another choice is an ibuprofen product (such as Advil).
- Note: Fevers less than 102° F (39° C) are important for fighting infections.
- For all fevers: Keep your child well hydrated. Give lots of cold fluids.
-
Fluids and Soft Diet:
- Try to get your child to drink adequate fluids.
- Goal: Keep your child well hydrated.
- Cold drinks, milk shakes, popsicles, slushes, and sherbet are good choices.
- Solid Foods: Offer a soft diet. Also avoid foods that need much chewing. Avoid citrus, salty, or spicy foods. Note: Fluid intake is much more important than eating any solid foods.
- Swollen tonsils can make some solid foods hard to swallow. Cut food into smaller pieces.
-
Return to School:
- Your child can return to school after the fever is gone. Your child should feel well enough to join in normal activities.
- Most often, having just a sore throat is not a reason to miss school.
- Children with Strep throat need to be taking an antibiotic for 24 hours.
-
What to Expect:
- Most often, sore throats with a viral illness last 4 or 5 days.
-
Call Your Doctor If:
- Sore throat is the main symptom and lasts more than 48 hours
- Sore throat with a cold lasts more than 5 days
- Fever lasts more than 3 days or goes above 104° F (40° C)
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.

The photo shows the typical Scarlet Fever rash on the forearm.
The scarlet fever rash first appears as tiny red bumps on the chest and abdomen that may spread all over the body. Looking like a sunburn, it feels like a rough piece of sandpaper, and lasts about 2-5 days.
Scarlet fever is a disease caused by the same bacteria (Streptococcus) that causes strep throat. A person with Scarlet fever has a throat that is red and sore, usually a fever, usually swollen glands in the neck, and a Scarlet fever rash.
Spider Bite
Is this your child's symptom?
- Bite from a spider
If NOT, try one of these:
Symptoms of a Spider Bite
- Most spider bites cause local pain, redness and swelling. It's much like a bee sting reaction.
- A few spiders (such as the Black Widow) can cause a more severe reaction.
- Helpful if spider seen on the skin or around the child
Cause of Spider Bite Reactions
- Most spiders have tiny fangs. They inject venom into the skin.
- The venom is what causes all the symptoms.
Types of Spider Bites
Black Widow Spider Bite
- A shiny, jet-black spider with long legs (total size 1 inch or 25 mm).
- A red (or orange) hourglass-shaped marking on its under-side.
- Causes immediate local pain and swelling.
- Sometimes, you can see 2 fang marks at the bite site.
- Severe muscle cramps (especially stomach cramps) occur within 1 to 6 hours. These last 24 to 48 hours.
- Rarely causes death. Exception: bitten by several spiders or small child is bitten.
- Note: many are dry bites because the fangs are small.
- The brown widow spider is related to the black widow. It is found in southern US.
- Brown widow spider bites are treated the same as black widow bites.
Brown Recluse Spider Bite
- A brown spider with long legs (total size ½ inch or 12 mm).
- A dark violin shaped marking on top of its head.
- Causes pain at the bite. Blisters form within 4 to 8 hours.
- The center becomes bluish and depressed (crater-like) over 2 to 3 days.
- Skin damage may require skin grafting in 10% of cases.
- Other symptoms such as fever, vomiting, muscle pain can occur. No life-threatening symptoms occur.
- Brown recluse spiders are hard to identify. If you can, bring the spider along in a jar.
Non-dangerous Spider Bites
- More than 50 spiders in the U.S. have venom. Their bites cause reactions that are not serious. This includes pain or redness at the bite site.
- The bites are painful and swollen. This lasts for 1 or 2 days. They can feel and look like a bee sting.
- Some single, unexplained, tender bites that occur during the night are due to spiders.
When to Call for Spider Bite
Call 911 Now
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Self Care at Home
|
Call 911 Now
- Trouble breathing or wheezing
- Passed out (fainted) or too weak to stand
- You think your child has a life-threatening emergency
Call Doctor or Seek Care Now
- Fever and bite looks infected (spreading redness)
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Call Doctor Within 24 Hours
- New redness starts more than 24 hours after the bite. Note: any redness in the first 24 hours is due to venom.
- More than 48 hours since the bite and redness now getting larger
- Bite starts to look bad (such as skin damage, blister or purple color)
- Bite pain lasts more than 2 days
- You think your child needs to be seen, but the problem is not urgent
Call Doctor During Office Hours
- You have other questions or concerns
Self Care at Home
- Non-serious spider bite
Care Advice for Non-dangerous Spider Bites
-
What You Should Know About Spider Bites:
- Most spider bites look and feel like a bee sting.
- The main symptoms are pain and redness.
- Here is some care advice that should help.
-
Clean the Bite:
- Wash the bite well with soap and water.
-
Cold Pack for Pain:
- For pain or swelling, use a cold pack. You can also use ice wrapped in a wet cloth.
- Put it on the bite for 20 minutes.
-
Pain Medicine:
- To help with the pain, give an acetaminophen product (such as Tylenol).
- Another choice is an ibuprofen product (such as Advil).
- Use as needed.
-
What to Expect:
- The swelling and pain lasts for 1 to 2 days.
- It should not be any worse than a bee sting.
-
Call Your Doctor If:
- Severe bite pain lasts more than 2 hours after pain medicine
- Stomach pains or muscle cramps occur
- Bite pain lasts more than 2 days (48 hours)
- Bite starts to look infected
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.

This is a photo of the Black Widow spider (Lactrodectus)
- The black widow is shiny and black, with long legs (total width 1 inch).
- A red (or orange) hourglass-shaped marking may be on its underside. However, this marking is not present in all Lactrodectus species.

This is a photo of the Brown Recluse Spider (Loxosceles reclusa).
- It is a brown spider with long legs (total width 1/2 inch).
- There is a characteristic violin-shaped marking is visible on back.
Stomach Pain - Female
Is this your child's symptom?
- Pain or discomfort in the stomach or belly area
- Female
- Pain found between the bottom of the rib cage and the groin crease
- The older child complains of stomach pain
- The younger child points to or holds the stomach
- Before 12 months of age, use the Crying care guides
If NOT, try one of these:
Causes of Acute Stomach Pain
- Eating Too Much. Eating too much can cause an upset stomach and mild stomach pain.
- Hunger Pains. Younger children may complain of stomach pain when they are hungry.
- GI Virus (such as Rotavirus). A GI virus can cause stomach cramps as well as vomiting and/or diarrhea.
- Food Poisoning. This causes sudden vomiting and/or diarrhea within hours after eating the bad food. It is caused by toxins from germs growing in foods left out too long. Most often, symptoms go away in less than 24 hours. It often can be treated at home without the need for medical care.
- Constipation. The need to pass a stool may cause cramps in the lower abdomen.
- Strep Throat. A strep throat infection causes 10% of new onset stomach pain with fever.
- Bladder Infection. Bladder infections usually present with painful urination, urgency and bad smelling urine. Sometimes the only symptom is pain in the lower abdomen.
- Appendicitis (Serious). Suspect appendicitis if pain is low on the right side and walks bent over. Other signs are the child won't hop and wants to lie still.
- Intussusception (Serious). Sudden attacks of severe pain that switch back and forth with periods of calm. Caused by one segment of bowel telescoping into a lower piece of bowel. Peak age is 6 months to 2 years.
Causes of Recurrent Stomach Pains
- Stress or Worries. The most common cause of frequent stomach pains is stress. Over 10% of children have a "worried stomach." These children tend to be sensitive and too serious. They often are model children. This can make them more at risk to the normal stresses of life. Examples of these events are changing schools, moving or family fights. The pain is in the pit of the stomach or near the belly button. The pain is real.
- Abdominal Migraine. Attacks of stomach pain and vomiting with sudden onset and offset. Often occur in children who later develop migraine headaches. Strongly genetic.
- Functional Abdominal Pains. Functional means the stomach pains are due to a sensitive GI tract. The GI tract is free of any disease.
- School Avoidance. Stomach pains that mainly occur in the morning on school days. They keep the child from going to school.
Pain Scale
- Mild: Your child feels pain and tells you about it. But, the pain does not keep your child from any normal activities. School, play and sleep are not changed.
- Moderate: The pain keeps your child from doing some normal activities. It may wake him or her up from sleep.
- Severe: The pain is very bad. It keeps your child from doing all normal activities.
When to Call for Stomach Pain - Female
Call 911 Now
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Self Care at Home
|
Call 911 Now
- Not moving or too weak to stand
- You think your child has a life-threatening emergency
Call Doctor or Seek Care Now
- Pain low on the right side
- Could be pregnant
- Constant pain (or crying) for more than 2 hours
- Recent injury to the stomach
- High-risk child (such as diabetes, sickle cell disease, recent abdominal surgery)
- Age less than 2 years old
- Fever over 104° F (40° C)
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Call Doctor Within 24 Hours
- Moderate pain that keeps from some normal activities
- Mild pain that comes and goes (cramps), but lasts more than 24 hours
- Fever is present
- Bladder infection (UTI) suspected (passing urine hurts, new onset wetting)
- You think your child needs to be seen, but the problem is not urgent
Call Doctor During Office Hours
- Stomach pains are a frequent problem
- You have other questions or concerns
Self Care at Home
- Mild stomach pain
Care Advice for Stomach Pain
-
What You Should Know About Stomach Pain:
- Mild stomach pain can be caused by something simple. It could be from gas pains or eating too much.
- Sometimes, stomach pain signals the start of a viral infection. This will lead to vomiting or loose stools.
- Watching your child for 2 hours will help tell you the cause.
- Here is some care advice that should help.
-
Lie Down:
- Have your child lie down and rest until feeling better.
-
Clear Fluids:
- Offer clear fluids only (such as water, flat soft drinks or half-strength Gatorade).
- For mild pain, offer a regular diet.
-
Prepare for Vomiting:
- Keep a vomiting pan handy.
- Younger children often talk about stomach pain when they have nausea. Nausea is the sick stomach feeling that comes before they throw up.
-
Pass a Stool:
- Have your child sit on the toilet and try to pass a stool.
- This may help if the pain is from constipation or diarrhea.
- Note: For constipation, moving a warm wet cotton ball on the anus may help.
-
Do Not Give Medicines:
- Any drug (like ibuprofen) could upset the stomach and make the pain worse.
- Do not give any pain medicines or laxatives for stomach cramps.
- For fever over 102° F (39° C), acetaminophen (such as Tylenol) can be given.
-
What to Expect:
- With harmless causes, the pain is most often better or gone in 2 hours.
- With stomach flu, belly cramps may happen before each bout of vomiting or diarrhea. These cramps may come and go for a few days.
- With serious causes (such as appendicitis), the pain worsens and becomes constant.
-
Call Your Doctor If:
- Pain becomes severe
- Constant pain lasts more than 2 hours
- Mild pain that comes and goes lasts more than 24 hours
- You think your child needs to be seen
- Your child becomes worse
-
Extra Help: Worried Stomach:
- Help your child talk about events that trigger the stomach pain. Talk to your child about how to cope with these the next time around.
- Help your child worry less about things she can't control.
- To treat the pain, help your child get very relaxed. Lying down in a quiet place and taking slow deep breaths may help. Make the belly go up and down with each breath. Then try to relax all the muscles in the body. Think about something pleasant. Listening to audios that teach how to relax might also help.
- Make sure your child gets enough sleep.
- Make sure that your child doesn't miss any school because of stomach pains. Stressed children tend to want to stay home when the going gets rough.
- Caution: Your child should see her doctor for an exam. Do this before concluding frequent stomach pains are from worrying too much.
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.
Stomach Pain - Male
Is this your child's symptom?
- Pain or discomfort in the stomach or belly area
- Male
- Pain found between the bottom of the rib cage and the groin crease
- The older child complains of stomach pain
- The younger child points to or holds the stomach
- Before 12 months of age, use the Crying care guides
If NOT, try one of these:
Causes of Acute Stomach Pain
- Eating Too Much. Eating too much can cause an upset stomach and mild stomach pain.
- Hunger Pains. Younger children may complain of stomach pain when they are hungry.
- GI Virus (such as Rotavirus). A GI virus can cause stomach cramps as well as vomiting and/or diarrhea.
- Food Poisoning. This causes sudden vomiting and/or diarrhea within hours after eating the bad food. It is caused by toxins from germs growing in foods left out too long. Most often, symptoms go away in less than 24 hours. It often can be treated at home without the need for medical care.
- Constipation. The need to pass a stool may cause cramps in the lower abdomen.
- Strep Throat. A strep throat infection causes 10% of new onset stomach pain with fever.
- Bladder Infection. Bladder infections usually present with painful urination, urgency and bad smelling urine. Sometimes the only symptom is pain in the lower abdomen.
- Appendicitis (Serious). Suspect appendicitis if pain is low on the right side and walks bent over. Other signs are the child won't hop and wants to lie still.
- Intussusception (Serious). Sudden attacks of severe pain that switch back and forth with periods of calm. Caused by one segment of bowel telescoping into a lower piece of bowel. Peak age is 6 months to 2 years.
Causes of Recurrent Stomach Pains
- Stress or Worries. The most common cause of frequent stomach pains is stress. Over 10% of children have a "worried stomach." These children tend to be sensitive and too serious. They often are model children. This can make them more at risk to the normal stresses of life. Examples of these events are changing schools, moving or family fights. The pain is in the pit of the stomach or near the belly button. The pain is real.
- Abdominal Migraine. Attacks of stomach pain and vomiting with sudden onset and offset. Often occur in children who later develop migraine headaches. Strongly genetic.
- Functional Abdominal Pains. Functional means the stomach pains are due to a sensitive GI tract. The GI tract is free of any disease.
- School Avoidance. Stomach pains that mainly occur in the morning on school days. They keep the child from going to school.
Pain Scale
- Mild: Your child feels pain and tells you about it. But, the pain does not keep your child from any normal activities. School, play and sleep are not changed.
- Moderate: The pain keeps your child from doing some normal activities. It may wake him or her up from sleep.
- Severe: The pain is very bad. It keeps your child from doing all normal activities.
When to Call for Stomach Pain - Male
Call 911 Now
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Self Care at Home
|
Call 911 Now
- Not moving or too weak to stand
- You think your child has a life-threatening emergency
Call Doctor or Seek Care Now
- Pain low on the right side
- Pain or swelling in the scrotum
- Constant pain (or crying) for more than 2 hours
- Recent injury to the stomach
- High-risk child (such as diabetes, sickle cell disease, recent abdominal surgery)
- Age less than 2 years old
- Fever over 104° F (40° C)
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Call Doctor Within 24 Hours
- Moderate pain that keeps from some normal activities
- Mild pain that comes and goes (cramps), but lasts more than 24 hours
- Fever is present
- Bladder infection (UTI) suspected (passing urine hurts, new onset wetting)
- You think your child needs to be seen, but the problem is not urgent
Call Doctor During Office Hours
- Stomach pains are a frequent problem
- You have other questions or concerns
Self Care at Home
- Mild stomach pain
Care Advice for Stomach Pain
-
What You Should Know About Stomach Pain:
- Mild stomach pain can be caused by something simple. It could be from gas pains or eating too much.
- Sometimes, stomach pain signals the start of a viral infection. This will lead to vomiting or loose stools.
- Watching your child for 2 hours will help tell you the cause.
- Here is some care advice that should help.
-
Lie Down:
- Have your child lie down and rest until feeling better.
-
Clear Fluids:
- Offer clear fluids only (such as water, flat soft drinks or half-strength Gatorade).
- For mild pain, offer a regular diet.
-
Prepare for Vomiting:
- Keep a vomiting pan handy.
- Younger children often talk about stomach pain when they have nausea. Nausea is the sick stomach feeling that comes before they throw up.
-
Pass a Stool:
- Have your child sit on the toilet and try to pass a stool.
- This may help if the pain is from constipation or diarrhea.
- Note: For constipation, moving a warm wet cotton ball on the anus may help.
-
Do Not Give Medicines:
- Any drug (like ibuprofen) could upset the stomach and make the pain worse.
- Do not give any pain medicines or laxatives for stomach cramps.
- For fever over 102° F (39° C), acetaminophen (such as Tylenol) can be given.
-
What to Expect:
- With harmless causes, the pain is most often better or gone in 2 hours.
- With stomach flu, belly cramps may happen before each bout of vomiting or diarrhea. These cramps may come and go for a few days.
- With serious causes (such as appendicitis), the pain worsens and becomes constant.
-
Call Your Doctor If:
- Pain becomes severe
- Constant pain lasts more than 2 hours
- Mild pain that comes and goes lasts more than 24 hours
- You think your child needs to be seen
- Your child becomes worse
-
Extra Help: Worried Stomach:
- Help your child talk about events that trigger the stomach pain. Talk to your child about how to cope with these the next time around.
- Help your child worry less about things he can't control.
- To treat the pain, help your child get very relaxed. Lying down in a quiet place and taking slow deep breaths may help. Make the belly go up and down with each breath. Then try to relax all the muscles in the body. Think about something pleasant. Listening to audios that teach how to relax might also help.
- Make sure your child gets enough sleep.
- Make sure that your child doesn't miss any school because of stomach pains. Stressed children tend to want to stay home when the going gets rough.
- Caution: Your child should see his doctor for an exam. Do this before concluding frequent stomach pains are from worrying too much.
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.
Stools - Blood In
Is this your child's symptom?
- Blood in or on the stool
- Blood can also be passed alone
- Blood in the stools is mostly bright red
- Blood from bleeding in the stomach comes out tar-black
- Included: Blood from constipation and anal fissure (tear)
Causes of Blood in Stool
- Anal Fissure. If no diarrhea, most of these children have a small tear in the anus. This is called an anal fissure. Anal fissures usually are caused by passage of a large or hard stool. This is the cause in 90% of children with blood in the stools.
- Strep Skin Infection. A Strep skin infection around the anus can also cause blood-streaked stools.
- Bacterial Diarrhea. If also has bloody diarrhea, a gut bacterial infection may be the cause. Examples are Shigella, Salmonella, E.Coli 0157 or Campylobacter.
- Cow's Milk Colitis. Starts within the first 2 months of life. Causes loose, slimy stools. Can be blood-streaked. Treatment: need to avoid cow's milk formulas.
- Blood spreads rapidly and widely in water. Passing a stool with a few blood streaks often turns the toilet water pink. It doesn't mean a large blood loss.
Causes of Red Stools, but not Blood
The things listed below can also cause red-colored stools that look like blood:
- Certain foods (such as tomatoes or beets)
- Certain drinks (such as red Kool-Aid)
- Certain medicines (such as amoxicillin or omnicef)
Anal Fissure or Tear
- An anal fissure is the most common cause of blood in the stools.
- It causes blood on the surface of a stool. Blood may also be found on toilet tissue after wiping.
- The blood is always bright red.
- Only a few streaks or flecks are seen.
- You may see a shallow tear at 6 or 12 o'clock on the anus.
- Caused by passing a large or hard stool.
When to Call for Stools - Blood In
Call 911 Now
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
|
Call 911 Now
- Passed out (fainted) or too weak to stand
- You think your child has a life-threatening emergency
Call Doctor or Seek Care Now
- Tarry or black-colored stool (not dark green)
- Blood with diarrhea
- Pink or tea-colored urine
- Stomach pain or crying also present
- Skin bruises not caused by an injury
- Age less than 12 weeks
- After an injury to anus or rectum
- High-risk child (such as with bleeding disorder or Crohn's disease)
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Call Doctor Within 24 Hours
- Small amount of blood in the stools. None of the symptoms above. Reason: most likely an anal fissure or tear. This needs a doctor's input.
- Note: try to save a sample of the "blood" for testing.
Care Advice for Anal Fissure
-
What You Should Know About Anal Fissures:
- An anal tear is the most common cause of blood in the stools.
- This is called an anal fissure.
- It causes blood on the surface of a stool.
- Blood may also be found on toilet tissue after wiping.
- It is caused by passing a hard or large stool.
- Here is some care advice that should help until you talk with your doctor.
-
Warm Saline Baths:
- Give a warm salt water bath for 20 minutes.
- Add 2 ounces (60 mL) of table salt to a tub of warm water. You can also use baking soda.
- Do 2 times per day for 1 day to cleanse the area and to help healing.
-
Steroid Ointment:
- If the anus seems red, use 1% hydrocortisone ointment (such as Cortaid). No prescription is needed.
- Put a little around the anus.
- Use 2 times per day for 1 day to help healing.
-
High-Fiber Diet:
- For children more than 1 year old, change the diet.
- Increase fruits, vegetables and grains (fiber).
- Reduce milk products to 3 servings per day.
- If Constipation is the cause, see that care guide.
-
What to Expect:
- Most often, anal tears heal up quickly with home treatment.
-
Call Your Doctor If:
- Bleeding gets worse
- Small bleeding occurs more than 2 times
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.
Stools - Unusual Color
Is this your child's symptom?
- Stool color that is strange or different than normal
- Normal stool colors are any shade of brown, tan, yellow or green
- The only colors that may be caused by a disease are red, black and white
- Dark green may look like black, but dark green is a normal color
If NOT, try one of these:
Causes of Unusual Stool Color
- Almost always due to food coloring or food additives.
- Stool color relates more to what is eaten than to any disease.
- In children with diarrhea, the gastrointestinal (GI) passage time is very rapid. Stools often come out the same color as the fluid that went in. Examples are Kool-Aid or Jell-O.
- The only colors we worry about are red, black (not dark green) and white.
Clues to Unusual Stool Colors
Red:
- "Bloody stools": 90% of red stools are not caused by blood
- Blood from lower GI tract bleeding
- Medicines. Red medicines (like Amoxicillin). Sometimes, other medicines that turn red in the GI tract (such as Omnicef)
- Foods. See list below.
Foods That Can Cause Red Stools:
- Red Jell-O, red or grape Kool-Aid
- Red candy, red licorice
- Red cereals
- Red frosting
- Red food coloring
- Beets
- Cranberries
- Fire Cheetos
- Paprika
- Red peppers
- Rhubarb
- Tomato juice or soup, tomato skin
Black:
- Blood from stomach bleeding (stomach acid turns blood to a dark, tar-like color)
- Foods. Licorice, Oreo cookies, grape juice
- Medicines. Iron, bismuth (Pepto-Bismol)
- Other. Cigarette ashes, charcoal
- Bile. Dark green stools from bile may look black under poor lighting. Smear a piece of stool on white paper. Look at it under a bright light. This often confirms that the color is really dark green.
Green:
- Green stools are always normal, but they can be mistaken for black stools.
- Bile. Most dark green stools are caused by bile.
- Green stools are more common in formula fed than breastfed infants. It can be normal with both.
- Green stools are more common with diarrhea. This is due to a fast transit time through the gut. However, formed stools can also be green.
- Dark green stools may look black under poor lighting. Eating spinach can cause dark green stools.
- Medicines. Iron (such as in formula)
- Foods. See list below.
Foods That Can Cause Green Stools:
- Green Jell-O
- Grape-flavored Pedialyte (turns bright green)
- Green fruit snacks
- Spinach or other leafy vegetables
White or Light Gray:
- Foods. Milk-only diet
- Medicines. Aluminum hydroxide (antacids), barium sulfate from barium enema
- Liver disease. Babies with blocked bile ducts have stools that are light gray or pale yellow.
When to Call for Stools - Unusual Color
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Self Care at Home
|
Call Doctor or Seek Care Now
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Call Doctor Within 24 Hours
- You think your child needs to be seen, but the problem is not urgent
Call Doctor During Office Hours
- Stool is light gray or white and occurs 2 or more times
- Strange color without a cause lasts more than 24 hours. Exception: green stools.
- Suspected food is stopped and strange color lasts more than 48 hours
- You have other questions or concerns
Self Care at Home
- Strange stool color most likely from food or medicine
- Green stools
Care Advice for Stools - Unusual Color
-
What You Should Know About Unusual Stool Color:
- Strange colors of the stool are almost always due to food coloring.
- The only colors that may relate to disease are red, black and white.
- All other colors are not due to a medical problem.
- Here is some care advice that should help.
-
Green Stools:
- Green color of the stools is always normal. Most often, green stools are caused by bile.
- Green stools are more common in formula fed than breastfed infants. But, they can be normal with both.
- Green stools are more common with diarrhea. This is due to a fast transit time through the gut. However, formed stools may also be green. This is normal and nothing to worry about.
- If your child takes iron, be sure your child is not taking too much.
-
Avoid Suspected Food or Drink:
- Don't eat the suspected food.
- Don't drink the suspected drink.
- The strange stool color should go away within 48 hours.
-
Save a Sample:
- If the strange stool color doesn't go away, bring in a sample.
- Keep it in the refrigerator until you leave.
-
What to Expect:
- Remove the cause of the unusual color from the diet.
- Then the stool should change back to normal color.
- This should happen within 48 hours or 2 stools later.
-
Call Your Doctor If:
- Strange color without a cause lasts more than 24 hours
- Suspected food is stopped and strange color lasts more than 48 hours
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.
Strep Throat Exposure
Is this your child's symptom?
- Close contact with someone who has a Strep throat infection.
- Close contact means living in the same house with the infected person. It also includes close physical contact such as having a kissing relationship.
If NOT, try one of these:
Strep Exposure (Close Contact)
- Household Close Contact. Lives with a person whose Strep test was positive. This can be a sibling, parent, or other household member.
- Kissing relationship with someone (boyfriend, girlfriend) who has a positive Strep test.
- Close contact should be within 10 days of onset of symptoms in exposed child. Reason: time from contact to Strep symptoms usually is 2 to 5 days.
- Throat cultures and rapid Strep tests aren't urgent. Most can be done in your doctor's office.
Types of Limited Contact with Strep
- Contact with someone outside the home with a positive Strep test. This type of contact occurs at school.
- Sometimes, the contact is with someone who was treated for Strep without testing.
- Children taking antibiotics for over 24 hours do not spread Strep to others.
When to Call for Strep Throat Exposure
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Self Care at Home
|
Call Doctor or Seek Care Now
- Stiff neck or can't move neck like normal
- Great trouble swallowing fluids or spit
- Trouble breathing or working hard to breathe
- Fever over 104° F (40° C)
- Dehydration suspected. No urine in more than 8 hours, dark urine, very dry mouth and no tears.
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent. Note: a Strep test alone is not urgent.
Call Doctor Within 24 Hours
- Sore throat pain is severe and not better 2 hours after taking ibuprofen
- Age less than 1 year old
- Earache or sinus pain (not just congestion)
- Mild symptoms that could be from Strep throat. (Some are sore throat, cries during feeds, large lymph nodes in the neck, fever)
- You think your child needs to be seen, but the problem is not urgent (or needs a Strep test)
Call Doctor During Office Hours
- You have other questions or concerns
Self Care at Home
- Strep contact but no symptoms
Care Advice
Treatment for Contacts With Symptoms (Pending a Strep Test)
-
What You Should Know About Strep Exposure and Sore Throats:
- A Strep test is not urgent.
- It could be a Strep throat or just a viral infection of the throat.
- A sore throat is often part of a cold.
- Until you get a Strep test, here is some care advice that should help.
-
Sore Throat Relief:
- Age over 1 year. Can sip warm fluids such as chicken broth or apple juice. Some children prefer cold foods such as popsicles or ice cream.
- Age over 6 years. Can also suck on hard candy or lollipops. Butterscotch seems to help.
- Age over 8 years. Can also gargle. Use warm water with a little table salt added. A liquid antacid can be added instead of salt. Use Mylanta or the store brand. No prescription is needed.
- Medicated throat sprays or lozenges are generally not helpful.
-
Pain Medicine:
- To help with the pain, give an acetaminophen product (such as Tylenol).
- Another choice is an ibuprofen product (such as Advil).
- Use as needed.
-
Fever Medicine:
- For fevers above 102° F (39° C), give an acetaminophen product (such as Tylenol).
- Another choice is an ibuprofen product (such as Advil).
- Note: Fevers less than 102° F (39° C) are important for fighting infections.
- For all fevers: Keep your child well hydrated. Give lots of cold fluids.
-
Fluids and Soft Diet:
- Try to get your child to drink adequate fluids.
- Goal: keep your child well hydrated.
- Cold drinks, milk shakes, popsicles, slushes, and sherbet are good choices.
- Solids. Offer a soft diet. Also avoid foods that need much chewing. Avoid citrus, salty, or spicy foods. Note: Fluid intake is much more important than eating any solids.
- Swollen tonsils can make some solid foods hard to swallow.
-
Return to School:
- Your child may have a Strep throat infection. Wait for the result of the rapid Strep test. If it is negative, your child can go back to school.
-
Call Your Doctor If:
- Your child becomes worse
Treatment for Contacts Without Symptoms
-
What You Should Know About Strep Exposure Without Symptoms:
- Many children have contact with someone with Strep throat. Most will not come down with an infection. This is especially true if the contact occurs outside the home.
- Strep tests are not needed for children without any symptoms.
-
Time It Takes to Get Strep Throat:
- Time from contact to Strep symptoms usually is 2 to 5 days.
-
Return to School:
- If your child has no symptoms, he does not need to miss any school.
-
Call Your Doctor If:
- Your child gets any Strep symptoms in the next 7 days
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.
Strep Throat Infection
Is this your child's symptom?
- Your child was diagnosed with a Strep throat infection
- A doctor has told you your child probably has Strep throat or
- Your child has a positive Strep test
- Your child is taking an antibiotic for Strep throat and you have questions
- You are worried that the fever or sore throat is not getting better fast enough
If NOT, try one of these:
Symptoms of Strep Throat Infection
- Pain, discomfort or raw feeling of the throat
- Pain is made worse when swallows
- Children less than 2 years of age usually can't complain about a sore throat. A young child who does not want favorite foods may have a sore throat. They may also start to cry during feedings.
- Other symptoms include sore throat, fever, headache, stomach pain, nausea and vomiting.
- Cough, hoarseness, red eyes, and runny nose are not seen with Strep throat. These symptoms point more to a viral cause.
- Scarlet fever rash (fine, red, sandpaper-like rash) is highly suggestive of Strep throat.
- If you look at the throat with a light, it will be bright red. The tonsil will be red and swollen, often covered with pus.
- Peak age: 5 to 15 years old. Not common under 2 years old unless sibling has Strep.
Cause of Strep Throat
- Group A Strep is the only common bacterial cause of a throat infection. The medical name is Strep pharyngitis.
- It accounts for 20% of sore throats with fever.
- Any infection of the throat usually also involves the tonsils. The medical name is Strep tonsillitis.
Diagnosis of Strep Throat
- Diagnosis can be confirmed by a Strep test on a sample of throat secretions.
- There is no risk from waiting until a Strep test can be done.
- If your child has cold symptoms too, a Strep test is usually not needed.
Prevention of Spread to Others
- Good hand washing can prevent spread of infection.
When to Call for Strep Throat Infection
Call 911 Now
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Self Care at Home
|
Call 911 Now
- Severe trouble breathing (struggling for each breath, can barely speak or cry)
- Fainted or too weak to stand
- You think your child has a life-threatening emergency
Call Doctor or Seek Care Now
- Trouble breathing, but not severe
- Great trouble swallowing fluids or spit
- Stiff neck or can't move neck like normal
- Dehydration suspected. No urine in more than 8 hours, dark urine, very dry mouth and no tears.
- Purple or blood-colored spots or dots on skin
- Fever over 104° F (40° C)
- Will not drink or drinks very little for more than 8 hours
- Can't open mouth all the way
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Call Doctor Within 24 Hours
- Urine is pink or tea (brown) color
- Taking antibiotic more than 24 hours, and sore throat pain is severe. (The pain is not better 2 hours after taking pain medicines)
- Taking antibiotic more than 48 hours and fever still there or comes back
- Taking antibiotic more than 3 days and other Strep symptoms not better
- You think your child needs to be seen, but the problem is not urgent
Call Doctor During Office Hours
- You have other questions or concerns
Self Care at Home
- Strep throat infection on antibiotic with no other problems
Care Advice for a Strep Throat Infection
-
What You Should Know About Strep Throat:
- Strep causes 20% of throat and tonsil infections in school age children.
- Viral infections cause the rest.
- Strep throat is easy to treat with an antibiotic.
- Complications are rare.
- Here is some care advice that should help.
-
Antibiotic by Mouth:
- Strep infections need a prescription for an antibiotic.
- The antibiotic will kill the bacteria that are causing the Strep throat infection.
- Give the antibiotic as directed.
- Try not to forget any of the doses.
- Give the antibiotic until it is gone. Reason: To stop the Strep infection from flaring up again.
-
Sore Throat Pain Relief:
- Age over 1 year. Can sip warm fluids such as chicken broth or apple juice. Some children prefer cold foods such as popsicles or ice cream.
- Age over 6 years. Can also suck on hard candy or lollipops. Butterscotch seems to help.
- Age over 8 years. Can also gargle. Use warm water with a little table salt added. A liquid antacid can be added instead of salt. Use Mylanta or the store brand. No prescription is needed.
- Medicated throat sprays or lozenges are generally not helpful.
-
Pain Medicine:
- To help with the pain, give an acetaminophen product (such as Tylenol).
- Another choice is an ibuprofen product (such as Advil).
- Use as needed.
-
Fever Medicine:
- For fevers above 102° F (39° C), give an acetaminophen product (such as Tylenol).
- Another choice is an ibuprofen product (such as Advil).
- Note: Fevers less than 102° F (39° C) are important for fighting infections.
- For all fevers: Keep your child well hydrated. Give lots of cold fluids.
-
Fluids and Soft Diet:
- Try to get your child to drink adequate fluids.
- Goal: Keep your child well hydrated.
- Cold drinks, milk shakes, popsicles, slushes, and sherbet are good choices.
- Solids. Offer a soft diet. Also avoid foods that need much chewing. Avoid citrus, salty, or spicy foods. Note: Fluid intake is much more important than eating any solids.
- Swollen tonsils can make some solid foods hard to swallow. Cut food into smaller pieces.
-
What to Expect:
- Strep throat responds quickly to antibiotics.
- The fever is usually gone by 24 hours.
- The sore throat starts to feel better by 48 hours.
-
Return to School:
- Your child can return to school after the fever is gone.
- Your child should feel well enough to join in normal activities.
- Children with Strep throat need to be taking an antibiotic for 24 hours.
-
Call Your Doctor If:
- Trouble breathing or drooling occurs
- Dehydration suspected
- Fever lasts more than 2 days after starting antibiotics
- Sore throat lasts more than 3 days after starting antibiotics
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.
Sty
Is this your child's symptom?
- A red lump or pimple on the edge of an eyelid
- It starts at the bottom of an eyelash
Symptoms of a Sty
- A tender, red lump on the eyelid at the base of an eyelash
- Turns into a small pimple on the eyelid
- A sty is tender to touch
- A sty causes mild swelling of the eyelid
- A sty can cause a watery eye
Causes
- A bacterial infection of the hair follicle of an eyelash.
- The most common germ that causes this is Staph.
- Risk factors. Rubbing the eyes (especially after picking the nose.) The nose is the most frequent home of Staph. Also, more common when using eye makeup.
When to Call for Sty
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Self Care at Home
|
Call Doctor or Seek Care Now
- Eyelid is very red or very swollen
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Call Doctor Within 24 Hours
- Sty gets larger than ¼ inch (6 mm)
- You think your child needs to be seen, but the problem is not urgent
Call Doctor During Office Hours
- 2 or more styes are present now
- Styes have occurred in the past 3 or more times
- Sty has come to a head (pimple), but has not drained after 3 days
- Sty lasts for more than 10 days
- You have other questions or concerns
Self Care at Home
- One sty
Care Advice for a Sty
-
What You Should Know About a Sty:
- A sty is a minor infection of an eyelash.
- A sty usually comes to a head and forms a pimple in 3 to 5 days.
- Most often, it drains and heals in a few more days.
- Most styes can be treated at home.
- Here is some care advice that should help.
-
Apply Heat to Bring to a Head:
- Put a warm, wet washcloth to the eye. Do this for 10 minutes 3 times a day. Reason: This helps the sty come to a head.
- Continue the warm wet cloth even after the sty begins to drain. Reason: To help remove the discharge and heal the sty.
- Caution: Do not rub the eye. Reason: Rubbing can cause more styes.
-
Open the Pimple:
- Age limit: Your child is over 5 years old and cooperative.
- When the center of the sty becomes yellow, you can open it. Do this by using tweezers. Pull out the eyelash that goes through the pimple. This will start drainage and healing.
- Another option is to wait for drainage to start on its own. Most often, this occurs in another 1-2 days.
- Caution: Do not squeeze the red lump. Reason: This can cause an eyelid infection.
-
Antibiotic Eye Medicine:
- Most single styes respond to the treatment with heat. They don't need prescription antibiotic eyedrops.
- If there is more than one sty, your child may need antibiotic eyedrops. Also, antibiotics may be needed if styes keep coming back. This usually happens to children who rub their eyes often.
-
Contact Lenses:
- Children who wear contact lenses need to switch to glasses until the sty heals.
- Reason: To prevent damage to the cornea.
- Disinfect the contacts before wearing them again.
- Discard them if they are disposable.
-
What to Expect:
- A sty usually comes to a head and forms a pimple in 3 to 5 days.
- Most often, it drains and heals in a few more days.
-
Return To School:
- Children with a sty usually do not need to miss any school.
-
Call Your Doctor If:
- Eyelid gets red or swollen
- Sty comes to a head, but does not drain by 3 days
- More styes occur
- Sty is not gone by 10 days
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.
Sunburn
Is this your child's symptom?
- Red or blistered skin from too much sun
- The redness, pain and swelling starts at 4 hours after being in the sun
- It peaks at 24 hours, and starts to get better after 48 hours
If NOT, try one of these:
Severity of Sunburn
- Most sunburn is a first-degree burn that turns the skin pink or red.
- Prolonged sun exposure can cause blistering and a second-degree burn.
- Sunburn never causes a third-degree burn or scarring.
Causes of Sunburn
- Direct sun exposure. Warning: clouds don't help. 70% of UV light still gets through on cloudy days.
- Reflected sun rays. From snow 80% is reflected, from sand 20%, from water only 5%.
- Tanning lamp or sun lamp.
- Tanning bed. A common cause in teens.
Ibuprofen to Reduce Pain and Other Symptoms
- Sunburn is an inflammatory reaction of the skin.
- Ibuprofen is a drug that can block this reaction. It can reduce the redness and swelling. But, it needs to be started early.
- Sunburns are sneaky. Many parents are surprised when their child gets a sunburn. Reason: there are no warning signs while the burn is occurring.
- Redness (sunburn) often is not seen until 4 hours after being in the sun. The pain and redness keep getting worse. They don't peak for 24 to 36 hours.
- Lesson: if you think your child got too much sun, start ibuprofen then. Give it 3 times per day for 2 days. Don't wait for redness.
When to Call for Sunburn
Call 911 Now
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Self Care at Home
|
Call 911 Now
- Passed out (fainted) or too weak to stand
- You think your child has a life-threatening emergency
Call Doctor or Seek Care Now
- Fever over 104° F (40° C)
- Can't look at lights because of eye pain
- Fever and looks infected (spreading redness more than 48 hours after the sunburn)
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Call Doctor Within 24 Hours
- Sunburn pain is severe and not better after using care advice
- Large blisters (more than ½ inch or 12 mm)
- Many small blisters at the burn site
- Blisters on the face
- Swollen feet make it hard to walk
- Looks infected (draining pus, red streaks, worse pain after day 2) and no fever
- You think your child needs to be seen, but the problem is not urgent
Call Doctor During Office Hours
- Itchy rashes in sun-exposed skin occur many times
- You have other questions or concerns
Self Care at Home
- Mild sunburn
Care Advice
Treating Mild Sunburn
-
What You Should Know About Sunburns:
- Most sunburns do not blister.
- Most blisters can be treated without needing to see a doctor.
- Here is some care advice that should help.
-
Ibuprofen for Pain:
- For pain relief, give an ibuprofen product (such as Advil). Start this as soon as you can.
- Give every 6-8 hours.
- Reason: If started within 6 hours, it can greatly limit the pain and swelling. Must give for 2 days.
- Caution: Not approved for age under 6 months.
-
Steroid Cream for Pain:
- Use 1% hydrocortisone cream (such as Cortaid) as soon as possible. No prescription is needed.
- Put it on 3 times per day.
- If used early and continued for 2 days, it may reduce swelling and pain.
- Use a moisturizing cream or aloe vera cream until you can get some.
- Use creams only. Avoid putting ointments on red skin. Reason: They can block the sweat glands.
- Burned skin can be very painful. Covering it with a cream can give great relief.
-
Cool Baths for Pain:
- Use cool wet washcloths to the burned area. Do this several times a day to reduce pain and burning.
- For larger sunburns, give cool baths for 10 minutes. Caution: Avoid any chill. Can add 2 ounces (60 mL) baking soda per tub.
- Do not use soap on the sunburn.
-
Fluids - Offer More:
- Offer extra water on the first day.
- This helps to replace the fluids lost into the sunburn.
- This will also help to prevent dehydration and dizziness.
-
Blisters - Don't Open:
- Caution: Leave closed blisters alone. Reason: To prevent infection.
- For broken blisters, trim off the dead skin. Use a fine scissors cleaned with rubbing alcohol.
-
Antibiotic Ointment for Open Blisters:
- For any large open blisters, use an antibiotic ointment (such as Polysporin). No prescription is needed.
- Remove it with warm water. Then, reapply it 2 times a day for 3 days.
-
What to Expect:
- Pain stops after 2 or 3 days.
- Peeling occurs day 5-7.
-
Call Your Doctor If:
- Pain becomes severe
- Sunburn looks infected
- You think your child needs to be seen
- Your child becomes worse
Preventing Sunburn
-
Sunscreens:
- Use a sunscreen with an SPF of 15 or higher. Fair-skinned children need a sunscreen with an SPF of 30. This is especially true if your child has red or blond hair.
- Put sunscreen on 30 minutes before exposure to the sun. This gives it time to get down into the skin. Give special attention to the areas most likely to become sunburned. Examples are the nose, ears, cheeks, and shoulders.
- Put sunscreen back on every 3 to 4 hours. Apply often while swimming or if sweating a lot. A "waterproof" sunscreen stays on for about 30 minutes in water.
- Most people use too little sunscreen. The average adult requires 1 ounce (30 mL) of sunscreen at a time.
- The best way to prevent skin cancer is to prevent sunburns.
-
Infants and Sunscreens:
- The skin of infants is thinner than the skin of older children. It is more sensitive to the sun.
- Sun avoidance is best for children under 6 months. Stay in the shade.
- Sun avoidance or sun proof clothing are best for children 6 months to 3 years. That means clothes that fully cover the arms and legs. Also, have your child wear a hat with a brim.
- When a sunscreen is needed, infants can use adult sunscreens. The FDA hasn't approved their use under 6 months old. However, the AAP supports their use at this age. There are no reported harmful side effects from today's sunscreens.
-
Protect Lips, Nose and Eyes:
- To prevent sunburned lips, apply a lip coating that contains sunscreen.
- If the nose or some other area has been burned often, protect it completely. Use zinc oxide or titanium oxide ointment.
- Protect your child's eyes from the sun's rays and cataracts with good sunglasses.
-
High-Risk Children:
- Some children are at higher risk for sunburn. If your child has red or blond hair, he is at higher risk. Fair-skinned children and children who never tan are also at higher risk.
- These children need to use a sunscreen even for brief exposures.
- They should avoid sun exposure whenever possible.
-
High-Risk Time of Day:
- Avoid exposure to the sun during the hours of 11:00 AM to 3:00 PM. This is when the sun's rays are most intense.
- Caution: When overcast, over 70% of the sun's rays still get through the clouds.
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.

This shows a second degree burn on the face. The area is red, raised and blistered.
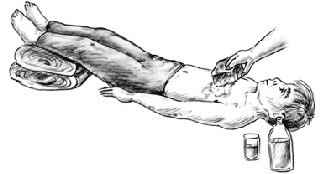
- Move the victim to a cool shady area. If possible, move into an air-conditioned place.
- The victim should lie down. Elevate the feet.
- Undress victim (except for underwear) so the body surface can give off heat.
- Sponge the entire body surface continuously with cool water. Fan the victim to increase evaporation.
- Give as much cold water or sports drink (e.g., Gatorade, Powerade) as the victim can tolerate. An adult or teen with heat exhaustion should drink 2-3 cups (480-720 ml) of liquids right away to replace what was lost. Then the adult or teen should drink approximately 1 cup (240 ml) every 15 minutes for the next 1-2 hours.

This shows a first-degree sunburn on the chest. It is red without blistering.
Suture Questions
Is this your child's symptom?
- Sutures or stitches questions
- Stapled wounds are treated the same as sutured wounds
- Skin glue (Dermabond) questions are also covered
If NOT, try one of these:
When Sutures (Stitches) are Needed for Cuts
- Any cut that is split open or gaping needs sutures.
- Cuts longer than ½ inch (12 mm) usually need sutures.
- On the face, cuts longer than ¼ inch (6 mm) usually need to be seen. They usually need closure with sutures or skin glue.
- Any open wound that may need sutures should be seen as soon as possible. Ideally, they should be checked and closed within 6 hours. Reason: to prevent wound infections. There is no cutoff, however, for treating open wounds.
When Sutures (Stitches) Should be Removed
- Stitches and staples are used to keep wounds together during healing.
- They need to be removed within 4-14 days.
- The specific removal date depends on the location of the stitches or staples.
- Removal should not be delayed. Reason: will leave skin marks.
Wounds That Re-Open After Closure
- Sutures that come out early cause the most concern.
- For open cuts, call your child's doctor now. General guidelines for re-suturing or re-gluing are listed below:
- Face Cuts. If a face wound has re-opened, call your doctor now. The cut may need to be re-glued or re-stitched. It does not matter how long it's been since sutures (or glue) were placed.
- Body Cuts and Less Than 48 Hours. If the wound is elsewhere on the body, call your doctor now. The cut may need restitched (or glued) if gaping open. This is sometimes done if suturing was less than 48 hours ago.
- Body Cuts and Over 48 Hours Ago. Call your doctor now for advice. After 48 hours, re-suturing is rarely done (except on the face). After 48 hours, the sutured wound can be reinforced with tape.
- Cut Is Closed, but suture has come out early. The wound should heal up fine without any further treatment. Check with your child's doctor within the next 24 hours.
When to Call for Suture Questions
Call 911 Now
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Self Care at Home
|
Call 911 Now
- Not moving or too weak to stand
- You think your child has a life-threatening emergency
Call Doctor or Seek Care Now
- Stitch (or staple) came out early and wound has opened up
- Wound looks infected (spreading redness, pus)
- Fever occurs
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Call Doctor Within 24 Hours
- Suture came out early but wound is still closed
- Suture removal is overdue
- You think your child needs to be seen, but the problem is not urgent
Call Doctor During Office Hours
- You have other questions or concerns
Self Care at Home
- Stitched or stapled wound with no other problems
Care Advice for Sutures
-
Care for a Normal Sutured or Stapled Wound:
- Keep sutured wounds completely dry for first 24 hours. (4 hours for Dermabond skin glue). If needed, use a sponge bath.
- After 24 hours, can take brief showers.
- Avoid swimming, baths or soaking the wound until sutures are removed. Avoid getting Dermabond skin glue wet until it has fallen off. Reason: Water in the wound can interfere with healing.
- Use an antibiotic ointment (such as Polysporin) 3 times a day. No prescription is needed. Reason: To prevent infection and a thick scab. (Caution: Don't apply any ointments or creams to Dermabond skin glue.)
- Cleanse surface with warm water once daily or if becomes dirty.
- Change wound dressing when wet or dirty.
- A dressing is no longer needed when edge of wound is closed. This takes about 48 hours. Exception: Dressing is needed to prevent sutures from catching on clothing.
-
Pain Medicine:
- To help with the pain, give an acetaminophen product (such as Tylenol).
- Another choice is an ibuprofen product (such as Advil).
- Use as needed.
-
Suture (or Staple) Removal Date. Here are some guidelines for when sutures (stitches) should be removed:
- Scalp: 7-10 days (same for staples)
- Face: 4-5 days
- Neck: 7 days
- Chest, abdomen or back: 7-10 days
- Arms and back of hands: 7 days
- Legs and top of feet: 10 days
- Palms, soles, fingers or toes: 12-14 days
- Overlying a joint: 12-14 days
-
Suture (or Staple) Removal Delays:
- Don't miss your appointment for removing sutures.
- Leaving sutures in too long can leave skin marks. Sometimes, it can cause scarring.
- It also makes taking the sutures out harder.
-
Suture (or Staple) Out Early:
- If the sutures come out early, close the wound with tape. You can also use a butterfly bandage (such as Band-Aid).
- Do this until the office visit.
-
Wound Protection After Sutures (or Staples) Out:
- Protect the wound from injury during the month after.
- Avoid sports that could re-injure the wound. If a sport is essential, cover with tape before playing.
- Allow the scab to fall off on its own. Do not try to pick it off. (Reason: Prevents scarring.)
-
Call Your Doctor If:
- Starts to looks infected
- Fever occurs
- Sutures come out early
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.
Swallowed Harmless Substance
Is this your child's symptom?
- Swallows an unusual but harmless, non-solid substance
- Swallows a bad-looking, bad-smelling, or bad tasting food
- Swallows a non-food substance
If NOT, try one of these:
Types of Harmless Substances
- Spoiled food. Small risk of vomiting or diarrhea.
- Raw or undercooked meat or eggs. Small risk of vomiting or diarrhea.
- Pet food. Safe if the pet food is fresh. Usually safe even if some of it has been eaten by the pet.
- Reptile food (such as mealworms or other small insects). Usually safe.
- Dead insects, spiders or worms found outside. Usually safe.
- Dirty water from toilet, fish tank, pond, stream. Small risk of vomiting and/or diarrhea.
- Dirt or sand. Small risk of swallowed germs from animal feces (poop).
- Human feces (poop). Usually, this is safe unless stool is diarrhea
- Animal feces (poop). Small risk of vomiting and/or diarrhea. Rare risk of worms.
- Cat litter. Harmless. It's sterilized earth or clay. Usually safe even if in a used cat box.
Spoiled Foods and Mold on Foods
- Main cause of spoiled food. Chilled food or drink left out at room temp over 2 hours. If food sits out all night (or power goes off to fridge), you should throw it away. Some examples of spoiled food are:
- Moldy cheese or bakery goods
- Curdled milk
- Rotten fruit
- Food scraps taken out of trash
- Eating a spoiled food is often harmless. Sometimes, it can cause mild vomiting or diarrhea. Serious symptoms are rare.
- Safest plan: Throw out spoiled or moldy foods.
Types of Harmless Products
The products below are harmless if tasted or swallowed:
- Soaps. Hand soaps (liquid or bar), shampoo
- Skin products. Corn starch baby powder is harmless. Talcum powder can be harmful if inhaled, but it is harmless if eaten. Hand lotions (creams or ointments), petroleum jelly and shaving cream are also safe. Creams and ointments that have over-the-counter (OTC) medicines in them are safe. OTC means you can buy them without a prescription. Examples are antibiotic, steroid, anti-fungal, anti-yeast, and diaper rash creams and ointments. A small taste of sunscreen is also safe. See next section.
- Make-up such as lipstick, blush, mascara. Deodorants and hair sprays are often also harmless, unless they have alcohol in them. Perfumes always have alcohol in them and can be harmful. See next section.
- Mouth products such as breath mints, chewing gum, small amount of toothpaste. Mouth washes may have alcohol in them and can be harmful. See below.
- Writing products. Includes chalk, crayons, paper, pen and marker ink. Lead pencils (which are really graphite) are also safe.
- Paints/Glue. White glue and arts-and-crafts glue are safe. Water color paints and water-based paints are also safe.
- Pets. Dog or cat food, cat litter (earth or clay) are safe.
- Other harmless items. Candles, cooking lard or grease, dirt, glow products (glow sticks), play dough, yard grass. Mercury in glass thermometers is safe if swallowed, but harmful if inhaled. Silica granules (in desiccant packets) are also safe.
Harmless Products, but Only if Swallowed in Small Amounts
The items listed below when eaten are usually safe and not a problem. But, there are exceptions. If a larger amount is swallowed, call the Poison Center.
- Deodorants. Exception: liquid type deodorant and more than a taste. Reason: may have alcohol in it.
- Hairspray. Exception: more than a taste. Reason: often has alcohol in it.
- Hand sanitizer. Exception: more than a taste. Reason: has 60% alcohol in it.
- Hydrogen peroxide 3%. Exception: more than 3%. Industrial strength solutions use 10 to 30%.
- Mouth washes. Exception: more than a taste. Reason: may have alcohol in it.
- Paper matches. Exception: 10 or more are eaten.
- Perfumes. Exception: more than a taste. Reason: perfumes have more than 90% alcohol.
- Sunscreens. Exception: eats more than 1 ounce (2 Tablespoons or 30 ml). Reason: Some sunscreens have aspirin-like products in them.
- Toothpaste. Exception: large amount, such as more than a mouthful (2 ounces or 60 mL).
Honey if Babies Under 12 Months Old
- If your baby has eaten honey (or another honey product), don't panic!
- Risk. In infants, honey has a very small link to a disease called infantile botulism. It is an illness that causes weak muscles. But, the good news is that it is rare. The risk to your baby is very small. Here are some facts and what to watch for.
- How honey can affect infants. Botulinum spores may be present in some honey products. These spores can lead to growth of bacteria in the gut. If this happens, the bacteria can release toxin. The toxin affects the muscles and cause weakness.
- Disease onset. 3-30 days after eating botulinum spores
- Infantile botulism symptoms. Usually starts with constipation. Other symptoms are trouble swallowing with lots of drooling and a poor suck. Your baby will have a hard time feeding. It can cause weakness such as a floppy head or limp arms and legs. Your baby may also have droopy eyes, a weak cry and seem more tired.
- Call your doctor. Call your doctor now if your baby has any of these symptoms. If caught early, treatment is usually successful without long-term effects.
- Prevention. Children under 1 year should not be given honey or liquid honey products. Children over 1 year and adults have more stomach acid than babies. The acid in the gut destroys the spores. This is why honey is safe after 1 year.
Food Poisoning
- What is it? Symptoms from eating a food with bacteria or toxins in it. Also known as a food-borne illness.
- Food poisoning outbreak. Defined as when 2 or more people come down with like symptoms. Happens after eating a common food at the same restaurant or outing. This finding helps to confirm food poisoning.
- Symptoms. Vomiting, nausea (upset stomach), stomach cramps and/or diarrhea. Fever is uncommon in cases of toxin-induced food poisoning.
- What to expect. Symptoms from toxins usually begin within 1 to 12 hours. They go away on their own and last less than 1 day. Symptoms from bacterial infections usually begin in 1 to 5 days. They can vary in severity and last a week or longer.
- Causes. It is caused by toxins from germs growing in foods left out too long. High-risk for Staph toxins are moist food dishes using milk, eggs or meat. Examples are potato salad, egg salad, homemade ice cream, turkey dressing. Another type of toxin food poisoning is from rice dishes. A common one is fried rice. The bacterial causes of food poisoning are often from under-cooked meats. Spoiled foods are rarely the cause. This is because people know they should throw them out and not eat them.
Dogs and Cats: Prevent Infections
- Keep regular visits with your pet's vet and get them de-wormed.
- Don't let your pet lick your child's face.
- Fact: Pets have many more harmful germs in their mouths than humans. Dogs like to smell and lick other dogs, animal feces (poop), and trash.
- Don't let your child kiss a pet.
- Clean up pet waste in your yard at least 3 times weekly.
- If your pet has diarrhea, take extra steps.
- Don't clean litter boxes if you are pregnant or have a weak immune system.
Petting Zoos: Prevent Infections
- Don't take children who suck their thumb or put items in their mouths.
- Don't take pacifiers or toys with you that can become dirty with germs.
- Watch children during the visit.
- Wash hands right after the visit.
- No eating or drinking during the visit.
Pica
- What is it? Pica is a chronic habit of eating non-food items.
- Age range. 18 months to adult
- Imitator. From 6 to 18 months old, young kids tend to put things in their mouths. This is a way to explore their world using their mouths. It's normal.
- Common items. Dirt, clay, paper, ice, crayons
- Complications. Lead poisoning from eating paint chips, other poisoning, worms from eating animal poop
- Cause. Anemia (low red blood cell count) from low iron is a major cause. When iron medicine is started, pica often goes away in 1 week. Other causes are obsessive-compulsive disorder, stress or modeling a parent.
- Treatment of pica. If not due to low iron, a psychologist should be able to help.
When to Call for Swallowed Harmless Substance
Call 911 Now
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Self Care at Home
|
Call 911 Now
- You think your child has a life-threatening emergency
Call Doctor or Seek Care Now
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Call Doctor Within 24 Hours
- Weak immune system. (Such as sickle cell disease, HIV, cancer, spleen removed, organ transplant, taking oral steroids). And your child also eaten spoiled food or feces (poop).
- Ate raccoon feces (poop). Reason: may need a prescription med.
- You think your child needs to be seen, but the problem is not urgent
Call Doctor During Office Hours
- Eating non-food items is a chronic problem (pica)
- You have other questions or concerns
Self Care at Home
- Ate food or drink that is spoiled or has set out at room temp
- Ate raw meat or eggs
- Ate human or animal feces (poop)
- Ate dirt, sand, or dirty water
- Ate other product or substance on the Harmless List. See lists in Causes section if unsure.
Care Advice
Spoiled Food or Drink Swallowed
-
What You Should Know About Swallowed Spoiled Food:
- Eating a spoiled food or drink shouldn't cause any problems. Your child should do fine.
- Your child may vomit once, just from the taste.
- A few children may vomit or have loose stools within the next 5 days.
- The illness is often mild and goes away on its own.
-
Treatment:
- No tests or cultures are needed.
- No treatment is needed or helpful.
- Antibiotics are not helpful.
- Feed your child a normal diet.
-
Call Your Doctor If:
- Your child vomits or has diarrhea in the next 5 days
- You have other questions or concerns
Raw Meat or Egg Swallowed
-
What You Should Know About Swallowed Undercooked Food:
- Eating undercooked/raw meat or eggs shouldn't cause any symptoms. Your child should do fine.
- A few children may vomit or have loose stools within the next 5 days.
- The illness is often mild and goes away on its own.
-
Treatment:
- No tests or cultures are needed.
- No treatment is needed or helpful.
- Antibiotics are not helpful.
- Feed your child a normal diet.
-
Call Your Doctor If:
- Your child vomits or has diarrhea in the next 5 days
- You have other questions or concerns
Feces (or Poop) Swallowed
-
What You Should Know About Swallowed Human Feces (Poop):
- Eating your own feces is always harmless. All of these germs are already in the child's body and digestive tract. Some young children in diapers may do this at some point. This will not cause illness. Only the parent is bothered by it.
- Eating another human's feces is probably harmless if that person is healthy now. If the other person has diarrhea, your child may also develop it.
-
What You Should Know About Swallowed Animal Feces (Poop):
- Eating feces from an animal is usually harmless.
- Many swallowed germs are destroyed by the acid in the stomach.
- Your child may vomit once, just from the taste.
- There's a small risk of getting diarrhea.
- There's a very small risk of getting worms.
- Write down the date your child ate the feces and the type of animal.
- If your child has any symptoms, this information may help your doctor. He can decide which tests would be helpful.
-
Treatment:
- No tests or cultures are needed.
- No treatment is needed or helpful.
- Antibiotics are not helpful.
- Feed your child a normal diet.
-
Prevent Your Child from Eating Animal Feces (Poop):
- Clean up animal waste from your yard before letting your child play there.
- Raccoon feces are high-risk for serious disease. If you have raccoons in your yard, call a pest control expert.
- Watch your child closely if they put non-food items in their mouth.
-
Call Your Doctor If:
- Your child vomits or has diarrhea in next month
- You have other questions or concerns
Dirt or Dirty Water Swallowed
-
What You Should Know About Swallowed Dirt:
- Dirt, sand or water outside can be dirty with animal feces (poop).
- Most all people swallow some dirt.
- Most children will do fine.
- There's a very small risk of getting diarrhea.
-
Dirty City Water:
- If the public water supply becomes dirty with germs, boil it.
- Bring the water to a boil. Then keep it boiling for 3 minutes. Reason: Should kill all the germs.
- Could also drink bottled water until the problem is fixed.
-
Treatment:
- No tests or cultures are needed.
- No treatment is needed or helpful.
- Antibiotics are not helpful.
- Feed your child a normal diet.
-
Call Your Doctor If:
- Your child vomits or has diarrhea in the next 3 weeks
- You have other questions or concerns
Other Items or Products on the Swallowed Harmless List
-
What You Should Know About Other Swallowed Harmless Items:
- Your child should do fine.
- Try to teach your child to only put food in their mouth.
-
Treatment:
- No tests or cultures are needed.
- No treatment is needed or helpful.
- Antibiotics are not helpful.
- Feed your child a normal diet.
-
Call Your Doctor If:
- Your child has any symptoms in the next 5 days
- You have other questions or concerns
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.
Tear Duct - Blocked
Is this your child's symptom?
- Blocked tube that normally carries tears from the eye to the nose
- It's blocked in 10% of newborns
- Use this guide only if a doctor has told you it's a blocked tear duct
Symptoms of a Blocked Tear Duct
- A constant watery eye
- Tears fill the eye and run down the face. This happens even when not crying.
- The eye is not red and the eyelid is not swollen.
- Both sides are blocked in 30% of these children.
Cause of a Blocked Tear Duct
- Caused by blockage of the lacrimal duct. This duct carries tears from the corner of the eye to the nose.
- A watery eye may not be noticed until 1 or 2 months old. Reason: that's when the eye starts making more tears.
When to Call for Tear Duct - Blocked
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Self Care at Home
|
Call Doctor or Seek Care Now
- Eyelid is very red or very swollen
- Clear part in the middle of the eye (cornea) is cloudy
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Call Doctor Within 24 Hours
- Red lump at inner corner of eyelid
- Eyelid is red or swollen
- Pus in the eye
- You think your child needs to be seen, but the problem is not urgent
Call Doctor During Office Hours
- Diagnosis has never been made by a doctor
- Age more than 12 months old
- You have other questions or concerns
Self Care at Home
- Blocked tear duct
Care Advice for Blocked Tear Duct
-
What You Should Know About Blocked Tear Ducts:
- A blocked tear duct is common. It happens in 10% of newborns.
- Both sides are blocked 30% of the time.
- A blocked tear duct does not need treatment unless it becomes infected.
- Here is some care advice that should help.
-
Antibiotic Eyedrops for Pus in the Eye:
- Pus in the eye or eyelids stuck together means the eye is infected.
- This is common with blocked tear ducts. It should clear up in a few days with antibiotic eyedrops.
- For pus in the eye, call your child's doctor for a prescription.
- In the meantime, here is some advice that should help.
-
Remove Pus:
- Remove the dried and liquid pus from the eyelids with warm water and wet cotton balls.
- Do this each time you see pus.
- Also, clean the eyes before you use the prescription eyedrops. The eyedrops will not work unless the pus is removed first.
-
Massage of Lacrimal Sac - Do it Carefully:
- Some doctors suggest massage of the lacrimal sac (where tears collect). Other doctors do not. Massage is not required. The tear duct will open without any massage. If massage is advised, do it this way:
- The lacrimal sac is in the inner corner of the lower eyelid. This sac can be massaged to empty it of old fluids.
- A cotton swab works much better than a finger. Reason: The swab is smaller.
- Start at the inner corner of the eye and press upward. Be very gentle. Do this twice a day.
- Fluid and mucus should come out of the lacrimal sac.
-
What to Expect:
- Over 90% of tear ducts open up on their own.
- This should happen by the time the child is 12 months of age.
- If your child is over 12 months old, talk to your child's doctor. Your child may need to see an eye doctor.
-
Call Your Doctor If:
- Eye looks infected
- Eyelid becomes red or swollen
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.
Teething
Is this your child's symptom?
- The normal process of new teeth working their way through the gums
- Questions about teething
- Baby teeth come in between 6 and 24 months of age
- Caution: At least one tooth should be seen before using this care guide
If NOT, try one of these:
Proven Symptoms of Teething
Teething has been researched in-depth. Kids who are teething are little different from kids who are not teething. Here are the main symptoms that have been proven:
- Drooling. Increased spit and drooling.
- Rash. Face rash from drooling. The drool contains little bits of food that are irritating to the skin.
- Chewing. Increased need to chew on things.
- Gum Pain. Gum pain is mild and not always present. May be due to mouth germs getting into the new break in the gum. Most often, your baby just acts a little more fussy. There's not enough discomfort to cause crying. It also doesn't hurt enough to cause sleep problems.
False Symptoms of Teething
- Teething does not cause fever, diarrhea, diaper rash or runny nose.
- It does not cause a lot of crying.
- It does not cause your baby to be more prone to getting sick.
- Caution about Fevers. Blaming teething for fevers can lead to a delay in seeking care for infections. Examples are ear and urinary tract infections. Another example is meningitis.
- There are 2 reasons why infections start between 6 and 12 months of age. One is the loss of antibodies transferred to baby from the mother at birth. The other is the developmental milestone of chewing on everything.
- Caution about Crying. Blaming teething for crying can lead to a delay of care for other illnesses. Examples are ear infections or other causes of pain.
When to Call for Teething
Call Doctor or Seek Care Now
|
Call Doctor During Office Hours
|
Self Care at Home
|
Call Doctor or Seek Care Now
- Your child looks or acts very sick
Call Doctor During Office Hours
- You think your child needs to be seen
- You have other questions or concerns
Self Care at Home
- Normal teething
Care Advice for Teething
-
What You Should Know About Teething:
- Teething is a natural process.
- It's harmless and it may cause a little gum pain.
- The main symptoms of teething are drooling and rubbing the gums.
- It does not cause fever or crying. If these are present, look for another cause.
- Here is some care advice that should help.
-
Gum Massage:
- Find the irritated or swollen gum.
- Rub it with your clean finger for 2 minutes.
- Do this as often as needed.
- Putting pressure on the sore gum can decrease pain.
- Age over 12 months. You can use a piece of ice wrapped in a wet cloth to rub the gum.
-
Teething Rings (Teethers):
- Babies rub their own sore gums by chewing on smooth, hard objects.
- Offer a teething ring, pacifier or wet washcloth that has been chilled. Chill these items in the fridge. Do not use items frozen in the freezer.
- Age over 12 months. A piece of chilled banana may help.
- Do not use hard foods that could cause choking. An example is a raw carrot.
- Do not use ice or popsicles that could cause frostbite of the gums.
-
Cup Feeding:
- If your baby refuses nipple feedings, try a cup.
- A spoon or syringe can also be used for a short time as needed.
-
Pain Medicine:
- Pain medicines usually are not needed for the mild discomfort of teething.
- Fussiness often gets better with gum massage. If not, you can give an acetaminophen product (such as Tylenol). If age over 6 months, another choice is an ibuprofen product (such as Advil). Just do this for one or two days. (Reason: Frequent use can cause liver or kidney damage).
-
Teething Gels: Do Not Use
- You can get special teething gels without a prescription.
- Most have benzocaine in them. They are not approved by the FDA at any age.
- Reason: Benzocaine can cause choking, bluish skin and allergic reactions. It can be very harmful if used during the first 2 years of life.
- Also, teething gels only give brief pain relief.
- Gum massage works much better.
-
What to Expect:
- Most often, teething does not cause any symptoms.
- If your child is having some discomfort, it should pass in 2 or 3 days.
-
Call Your Doctor If:
- Crying occurs
- Fever occurs
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.
Thrush
Is this your child's symptom?
- A yeast infection of the mouth in young babies
- White patches in the front of the mouth
If NOT, try one of these:
Symptoms of Thrush
- White, odd shaped patches in the mouth
- Coats the inner cheeks or inner lips
- Sometimes also coats the tongue
- Sticks to the mouth. It can't be washed away or wiped off easily like milk curds.
- Sometimes causes a painful mouth, decreased sucking and reduced milk intake
- Mild discomfort or no symptoms in most newborns
- The infant is bottle-fed or breast-fed
Cause of Thrush
- Caused by a yeast (called Candida)
- Occurs on parts of the mouth involved with sucking
- Made worse by friction from too much time sucking on a pacifier
White Tongue Alone: Not Thrush
- If a white tongue is the only finding, it's not due to thrush.
- A milk diet often causes a white coated tongue.
- This is normal.
- It will go away after your baby starts eating solid foods.
- If white patches occur inside the lips or cheeks, call your child's doctor. It's safe to call during office hours.
When to Call for Thrush
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Call Doctor or Seek Care Now
- Dehydration suspected. No urine in more than 8 hours, dark urine, very dry mouth and no tears.
- Age less than 1 month old and looks or acts abnormal in any way
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Call Doctor Within 24 Hours
- Fever occurs
- Bleeding in the mouth
- Drinking less than normal
- You think your child needs to be seen, but the problem is not urgent
Call Doctor During Office Hours
- Thrush, but none of the symptoms above. Reason: may need a prescription medicine to treat it.
- You have other questions or concerns
Care Advice for Thrush
-
What You Should Know About Thrush:
- Thrush is common during the early months of life.
- It's caused by a yeast infection in the mouth. Most often, it's due to prolonged sucking.
- Thrush causes only mild discomfort. It's easy to treat at home.
- Here is some care advice that should help until you call your doctor.
-
Anti-Yeast Medicine (Prescription):
- Your doctor will probably prescribe an anti-yeast liquid medicine. Use it as follows:
- Age Under 1 Month: Use 1 mL.
- Age Over 1 Month: Use 2 mLs.
- Place in the front of the mouth on each side. Also, put it wherever you see the thrush. It doesn't do any good once it's swallowed.
- Do this 4 times per day.
- If the thrush isn't getting better, rub the medicine directly on the thrush. Use a cotton swab to do this.
- Don't feed your baby anything for 30 minutes after the medicine.
- Keep this up for at least 7 days. Also, continue it until all thrush has been gone for 3 days.
-
Decrease Sucking Time to 20 Minutes per Feeding:
- Reason: Too much sucking can irritate the lining of the mouth. This makes it more prone to a yeast infection. A common example of this is when a baby sleeps with a bottle.
- For severe mouth pain with bottle feeding, don't use a bottle. Reason: The nipple can make pain worse.
- Try giving fluids in a cup, spoon or syringe instead.
-
Limit Pacifier Use:
- Too much sucking on a pacifier can irritate the mouth.
- Limit pacifier use to times when nothing else will calm your baby.
- If your infant is using an orthodontic pacifier, switch to a smaller, regular one. Reason: Bigger ones can cause more friction in the mouth.
- Special washing or boiling of pacifiers or bottle nipples is not needed or helpful.
-
Special Washing of Pacifiers and Nipples - Not Helpful:
- Pacifiers and bottle nipples can be washed the usual way with soap and water.
- They do not need to be boiled or sterilized.
- They do not need to be thrown out.
- Yeast is a germ that is found in normal mouths.
- It only causes thrush if the lining of the mouth is irritated or damaged.
- Get better results by reducing nipple time and pacifier time.
- Note: Follow your doctor's advice if it is different.
-
Breastfeeding and Yeast Symptoms:
- If the mother's nipples are red and sore, it's probably a yeast infection.
- Use an anti-yeast cream (such as Lotrimin) on the nipple area.
- No prescription is needed.
- Put it on 4 times per day after feedings.
- Wash the cream off the nipples before each nursing. Avoid soap which dries out the skin.
- Many mothers will need treatment with an oral anti-yeast medicine (such as Diflucan). Call your PCP or OB within 24 hours for advice.
-
Diaper Rash Treatment:
- If there's a bad diaper rash, it can also be due to yeast.
- Use an anti-yeast cream (such as Lotrimin) on the diaper rash.
- No prescription is needed.
- Put it on 4 times per day.
- See Diaper Rash care guide.
-
Return to Child Care:
- Thrush cannot be spread to others, since it does not invade normal skin.
- Your child can go to child care with thrush.
-
What to Expect:
- With treatment, thrush usually clears up in 4 to 5 days.
- Without treatment, it clears up in 2-8 weeks.
-
Call Your Doctor If:
- Starts drinking less than normal
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.
Tick Bite
Is this your child's symptom?
- A tick (small brown bug) is attached to the skin
- A tick was removed from the skin
If NOT, try one of these:
Symptoms of a Tick Bite
- A tick bite does not cause pain or itch. So, ticks may not be noticed for a few days.
- After feeding on blood, ticks get swollen and easier to see.
- Ticks fall off on their own after sucking blood for 3 to 6 days.
- After the tick comes off, a little red bump may be seen.
- The red bump or spot is the body's response to the tick's saliva (spit).
- While it's sucking blood, some of its spit gets mixed in.
Causes of Tick Bites
- The wood tick (dog tick) is the size of an apple seed. After feeding, it can double or triple in size. Sometimes, it can pass on Rocky Mountain spotted fever or Colorado tick fever.
- The deer tick is the size of a poppy seed. After a feeding, it can triple in size. Sometimes, it can pass on Lyme disease.
Lyme Disease
- Over 95% of people who get Lyme disease live in or have traveled to 14 high-risk states. Lyme disease mainly occurs in the Northeast, Mid-Atlantic and upper Midwest. Many states do not have Lyme disease. The CDC reports over 30,000 new cases per year (2015).
- About 80% of Lyme disease starts with a bull's eye rash called erythema migrans. The rash starts at the site of the tick bite. It starts on the average at 7 days. It grows larger quickly, to more than 2 inches (5 cm) wide. It can become as large as 12 inches (30 cm). It lasts 2 or 3 weeks. Treatment of this rash with an antibiotic is advised. This almost always prevents the later stages of Lyme Disease. If Lyme Disease isn't treated, heart, joint and neurologic problems can occur.
- Giving antibiotics after deer tick bites to prevent Lyme Disease depends on the risk. The risk is low with brief attachment. The risk is high if the deer tick was attached for longer than 36 hours. It's also higher if the tick is swollen, not flat. Ask your doctor for advice.
- The risk of Lyme Disease after a deer tick bite is low. Even in high risk areas, only 2% of deer tick bites cause Lyme Disease.
When to Call for Tick Bite
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Self Care at Home
|
Call Doctor or Seek Care Now
- Can't remove the tick after trying this care advice
- Widespread rash starts 2 to 14 days after the bite
- Fever or headache starts 2 to 14 days after the bite
- Fever and bite looks infected (spreading redness)
- Weak, droopy eyelid, droopy face or crooked smile
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Call Doctor Within 24 Hours
- Deer tick was attached for more than 36 hours
- Deer tick is swollen, not flat
- New redness starts more than 24 hours after the bite. Note: bacterial infection is rare. It does not start until at least 24-48 hours after the bite.
- More than 48 hours since the bite and redness now getting larger
- Red-ring or bull's eye rash occurs around a deer tick bite. Note: the rash of Lyme disease starts 3 to 30 days after the bite.
- You think your child needs to be seen, but the problem is not urgent
Call Doctor During Office Hours
- You have other questions or concerns
Self Care at Home
- Wood tick bite
- Deer tick bite
- Preventing tick bites
Care Advice
Treating Tick Bites
-
What You Should Know About Wood Tick Bites:
- Most wood tick bites are harmless.
- The spread of disease by wood ticks is not common.
- If the tick is still attached to the skin, it needs to be taken off.
- Try one of the methods described below to take out the tick.
-
Wood Tick - How to Remove with Tweezers:
- Use tweezers. Grasp the tick as close to the skin as possible (on its head).
- Hold the tweezers sideways next to the top of the skin.
- Pull the wood tick straight upward without twisting or crushing it.
- Keep a steady pressure until the tick lets go of its grip.
- If you don't have tweezers, you can use your fingers.
- Other options. You can use a loop of thread around the jaws. You can also use a needle pushed between the jaws for traction. Jaws are the part of the head attached to the skin.
- Not helpful: Covering the tick with petroleum jelly or nail polish doesn't work. Neither does rubbing alcohol or a soapy cotton ball. Touching the tick with a hot or cold object also doesn't work.
-
What You Should Know About Deer Tick Bites:
- Most deer tick bites are harmless.
- The spread of disease by deer ticks is not common.
- Even in high risk areas, only 2% of deer tick bites cause Lyme disease.
- Most people who get Lyme disease live in or have traveled to 14 high-risk states. Lyme disease mainly occurs in the Northeast and upper Midwest. Many states do not have Lyme disease.
-
Deer Tick - How to Remove:
- If it is swollen, try to remove with a tweezers. See wood tick advice.
- Tiny deer ticks need to be scraped off.
- You can remove them with the edge of a credit card.
-
Tick's Head - When to Remove:
- If the wood tick's head (mouth parts) breaks off in the skin, remove any large pieces.
- Clean the skin with rubbing alcohol.
- Use a clean tweezers or needle to scrape it off.
- If a small piece remains, the skin will slowly heal and shed it.
-
Antibiotic Ointment:
- After the tick is removed, wash the wound with soap and water. Also, wash your hands after you are done.
- This helps to prevent catching any infections carried by the tick.
- Use an antibiotic ointment (such as Polysporin). No prescription is needed.
- Put it on the bite once.
-
What to Expect:
- Most often, tick bites don't itch or hurt.
- That's why they may not be noticed.
- The little bump goes away in 2 days.
- If the tick transferred a disease, a rash will occur. It will appear in the next 4 weeks.
-
Call Your Doctor If:
- You tried and can't remove the tick
- Fever or rash happens in the next 4 weeks
- Bite starts to look infected
- You think your child needs to be seen
- Your child becomes worse
Prevent Tick Bites
-
Prevent Tick Bites:
- After being outdoors in deer tick areas, check for ticks. Remove any that are attached. Also, take a shower soon after coming inside.
- Tumble any clothing in a hot dryer for 10 minutes. That should kill any ticks left in the clothing.
- When hiking outside where there are ticks, wear long clothing. Tuck the ends of pants into socks.
- Use a bug repellent to shoes, socks and exposed skin.
-
Tick Repellent for Clothing - Permethrin:
- Permethrin products (such as Duranon) work well to repel ticks.
- Unlike DEET, these products are put on clothing instead of skin. They also can last through many washes. Use it on pant cuffs, socks and shoes. You can also put it on other outdoor items (bug netting, sleeping bags).
- Do not put it on skin. Reason: Sweat changes it so it does not work.
-
Tick Repellent for Skin - DEET:
- DEET also works well to repel ticks. It can be used on the skin not covered by clothing.
- Use 20-30% DEET for children and teens (AAP). Note: 30% DEET protects for 6 hours.
- DEET is approved for use in children over 2 months of age (AAP).
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.

This is a picture of a brown Wood Tick.
The Wood Tick (also called dog tick) can sometimes transmit Rocky Mountain spotted fever and Colorado tick fever.

The Deer Tick (also called black-legged tick) is between the size of a poppy seed and an apple seed.
The deer tick is found on a wide rage of hosts including mammals, birds and reptiles.
This tick can transmit Lyme disease to humans and animals during feeding; this occurs when the tick insert its mouth parts into the skin of a host and slowly ingests the host's blood.
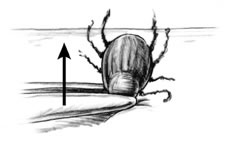
Wood Tick Removal:
- Use a pair of tweezers and grasp the wood tick close to the skin (on its head). See image.
- Pull the wood tick straight upward without twisting or crushing it. Maintain a steady pressure until it releases its grip.
- If tweezers aren't available, use fingers, a loop of thread around the jaws, or a needle between the jaws for traction.
Tiny Deer Tick Removal:
- Needs to be scraped off with a knife blade or credit card edge.
- Place tick in a sealed container (e.g., glass jar, zip lock plastic bag), in case your doctor wants to see it.
Note: Covering the tick with petroleum jelly, nail polish or rubbing alcohol doesn't work. Neither does touching the tick with a hot (like a match) or cold object.

The majority of cases of Lyme disease start with a bull's eye rash at the site of the tick bite. The rash can occur days to weeks (typically 7-10 days) after a tick bite.
Treatment with antibiotics is indicated if this rash appears.
It is thought that Lyme Disease can be prevented if the tick is removed within 24 hours of attachment.
Toe Injury
Is this your child's symptom?
- Injuries to toes
If NOT, try one of these:
Types of Toe Injuries
- Cuts, Scrapes and Bruises. These are the most common injuries.
- Jammed Toe. The end of a straightened toe receives a blow. This is usually from stubbing the toe on an object. The energy is absorbed by the joint surface and the injury occurs there. This is called traumatic arthritis.
- Crushed or Smashed Toe. This is usually from something heavy falling on the toe. Sometimes, the nail can be damaged. Fractures are unusual, but are at risk for a bone infection (osteomyelitis).
- Toenail Injury. If the nailbed is cut, it may need sutures to prevent a permanently deformed nail. This is less important for toenails.
- Subungual Hematoma (Blood Clot under the Nail). Most often caused by a crush injury. It can be from a heavy object falling on the nailbed. Many are only mildly painful. Some are severely painful and throbbing. These need the pressure under the nail released. A doctor can put a small hole through the nail to release the blood. This can relieve the pain and prevent loss of the nail.
- Dislocations. The toe has been pushed out of its joint.
- Fractures. Toe has a broken bone. The treatment is the same whether the toe is broken or just bruised. Broken toes are not put in a cast.
Concerns About Missing a Broken Toe
- Most swollen, bruised and painful toes are not broken.
- X-rays are only needed for severe pain and severe injuries.
- If the big toe might be broken, it should be seen by a doctor. The other injured toes generally don't need to be seen.
- A broken great toe is not urgent. It can be checked during office hours.
- The treatment is the same whether or not the toe is broken.
- The treatment of all broken toes is pain medicine and comfortable footwear.
Pain Scale
- Mild: Your child feels pain and tells you about it. But, the pain does not keep your child from any normal activities. School, play and sleep are not changed.
- Moderate: The pain keeps your child from doing some normal activities. It may wake him or her up from sleep.
- Severe: The pain is very bad. It keeps your child from doing all normal activities.
When to Call for Toe Injury
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Self Care at Home
|
Call Doctor or Seek Care Now
- Skin is split open or gaping and may need stitches
- Large swelling is present
- Blood under a nail is causing more than mild pain
- Nail is torn
- Base of nail has popped out from under the skin fold
- Dirt in the wound is not gone after 15 minutes of scrubbing
- Severe pain and not better 2 hours after taking pain medicine
- Age less than 1 year old
- Age less than 2 years and toe tourniquet suspected. (Hair wrapped around toe, groove, swollen red or bluish toe)
- You think your child has a serious injury
- You think your child needs to be seen, and the problem is urgent
Call Doctor Within 24 Hours
- Broken toe suspected
- Toe injury that causes bad limp
- You think your child needs to be seen, but the problem is not urgent
Call Doctor During Office Hours
- Dirty cut and no tetanus shot in more than 5 years
- Clean cut and no tetanus shot in more than 10 years
- Pain not better after 3 days
- Not using the toe normally after 2 weeks
- You have other questions or concerns
Self Care at Home
- Minor toe injury
Care Advice for Minor Toe Injuries
-
What You Should Know About Toe Injuries:
- There are many ways that children can hurt their toes.
- There are also many types of toe injuries.
- You can treat minor toe injuries at home.
- Here is some care advice that should help.
-
Pain Medicine:
- To help with the pain, give an acetaminophen product (such as Tylenol).
- Another choice is an ibuprofen product (such as Advil).
- Use as needed.
-
Bruised/Swollen Toe:
- Soak in cold water for 20 minutes.
- Repeat as needed.
-
Small Cuts or Scratches:
- For any bleeding, put direct pressure on the wound. Use a gauze pad or clean cloth. Press down firmly on the place that is bleeding for 10 minutes. This is the best way to stop bleeding. Keep using pressure until the bleeding stops.
- Wash the wound with soap and water for 5 minutes.
- For any dirt in the wound, scrub gently.
- For any cuts, use an antibiotic ointment (such as Polysporin). No prescription is needed.
- Cover it with a bandage (such as Band-Aid). Change daily.
-
Jammed Toe:
- Caution: Be certain range of motion is normal. Your child should be able to bend and straighten each toe. If movement is limited, your doctor must check for a broken bone.
- Soak the foot in cold water for 20 minutes.
- If the pain is more than mild, "buddy-tape" it to the next toe.
-
Smashed or Crushed Toe:
- Wash the toe with soap and water for 5 minutes.
- For any cuts, use an antibiotic ointment (such as Polysporin). No prescription is needed.
- Cover it with a bandage (such as Band-Aid). Change daily.
-
Torn Nail (from catching it on something):
- For a cracked nail without rough edges, leave it alone.
- For a large flap of nail that's almost torn through, cut it off. Use a pair of scissors that have been cleaned. Cut along the line of the tear. Reason: Pieces of nail taped in place will catch on objects.
- Soak the toe for 20 minutes in cold water for pain relief.
- Use an antibiotic ointment (such as Polysporin). No prescription is needed. Then cover with a bandage (such as Band-Aid). Change daily.
- After about 7 days, the nailbed should be covered by new skin. It should no longer hurt. A new nail will grow in over 6 to 8 weeks.
-
Shoes to Reduce Pain:
- If regular shoes cause too much pain, make a change in footwear.
- Wear a shoe with a firm sole to limit motion. Reason: Injured toes hurt when they bend (are flexed).
- If the top of the shoe increases pain, wear an open-toe sandal. Another option is to use an old sneaker. Then cut out the part over the toe.
-
Buddy-taping:
- Buddy-taping is taping the injured toe to the one next to it.
- Method: Gauze padding must be placed between the toes before taping them together.
- How long to buddy tape: Usually needed for 1 - 2 weeks. By then new bone formation will close the break. Then pain with movement will be reduced.
- Usefulness: Buddy-taping is optional. Sometimes, it makes the pain worse. Wearing the right shoe is much more helpful.
-
Call Your Doctor If:
- Pain becomes severe
- Pain not better after 3 days
- Toe not normal after 2 weeks
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.

- Apply direct pressure to the entire wound with a sterile gauze dressing or a clean cloth.
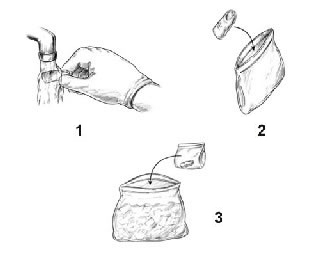
- Step 1: Briefly rinse amputated part with water (to remove any dirt)
- Step 2: Place amputated part in plastic bag (to protect and keep clean)
- Step 3: Place plastic bag containing the part in a container of ice (to keep cool and preserve tissue).
Note: Take patient and amputated part to emergency department immediately.
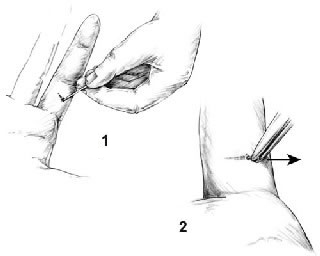
You can remove splinters, larger slivers, and thorns with a needle and tweezers. Check the tweezers beforehand to be certain the ends (pickups) meet exactly. (If they do not, bend them.) Sterilize the tools with rubbing alcohol or a flame.
Clean the skin surrounding the sliver briefly with rubbing alcohol before trying to remove it. Be careful not to push the splinter in deeper. If you don't have rubbing alcohol, use soap and water, but don't soak the area if FB is wood (Reason: can cause swelling of the splinter).
Remove the splinter:
- Step 1: Use the needle to completely expose the large end of the sliver. Use good lighting. A magnifying glass may help.
- Step 2: Then grasp the end firmly with the tweezers and pull it out at the same angle that it went in. Getting a good grip the first time is especially important with slivers that go in perpendicular to the skin or those trapped under the fingernail.
Toenail - Ingrown
Is this your child's symptom?
- The corner of the toenail grows into the skin around it
- Almost always involves the big toe (great toe)
Symptoms of an Ingrown Toenail
- Toe pain from sharp corner of toenail cutting into surrounding skin.
- Redness and swelling around the corner of the toenail is usually present.
- The area may drain pus or yellow fluid.
- The red area is very tender to touch or pressure from a shoe.
- Some teens with an ingrown toenail can barely walk.
Cause of an Ingrown Toenail
- The toenail is usually pushed into the skin by wearing tight shoes.
- The tiny cut made by the nail allows bacteria to enter the skin. The cut then becomes infected.
- The sharp corner of buried nail keeps growing. The deeper it goes, the more painful it becomes.
When to Call for Toenail - Ingrown
Call 911 Now
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Self Care at Home
|
Call 911 Now
- You think your child has a life-threatening emergency
Call Doctor or Seek Care Now
- Spreading red area or streak with fever
- Spreading red area or streak that's very large
- Severe pain not improved 2 hours after pain medicine and antibiotic ointment
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Call Doctor Within 24 Hours
- Spreading red area or streak, but no fever
- Entire toe is red and swollen
- Pus pocket (yellow or green) seen in skin around toenail or under toenail. Reason: needs to be drained.
- You think your child needs to be seen, but the problem is not urgent
Call Doctor During Office Hours
- Can't locate and free up corner of toenail
- After using Care Advice more than 2 days, pus discharge not gone
- After using Care Advice more than 3 days, still hard to walk
- After using Care Advice more than 7 days, not improved
- After using Care Advice more than 14 days, not gone
- Ingrown toenails are a frequent problem
- You have other questions or concerns
Self Care at Home
- Minor ingrown toenail
Care Advice for Ingrown Toenail
-
What You Should Know About Ingrown Toenails:
- Ingrown toenails are always painful.
- Pain is caused by the sharp toenail edge cutting into the skin around it.
- The pain can be stopped. Find the toenail corner and lift it out of the raw tissue.
- This will allow the area to heal.
- Most ingrown toenails can be treated at home. Surgery or nail removal is rarely needed.
- Here is some care advice that should help.
-
Warm Soaks:
- Soak the toe in warm water and soap for 20 minutes twice a day.
- While soaking, massage the swollen part of the cuticle (skin next to the nail). Massage away from the nail.
- While soaking, also try to bend the corners of the toenail upward.
- Dry the toe and foot completely.
-
Elevate Corner of Toenail with Dental Floss:
- Goal: To help the toenail corner grow over the cuticle, rather than into it.
- Take a short strip of dental floss or fishing line. Try to slip it under the corner of the nail. Then, lift the nail upward. Cut off any sharp edge.
- Take a small wedge of cotton from a cotton ball. Try to place the wedge under the nail corner to keep it elevated. (Sometimes this step is impossible).
- Elevate the corner away from the cuticle with every soak.
-
Antibiotic Ointment:
- After each soak, use an antibiotic ointment (such as Polysporin). Put it on the swollen part of the toe.
- You can buy this ointment without a prescription.
-
Taking Pressure Off Toenail With a Cotton Ball:
- Until it heals, try to wear sandals or go barefoot.
- When your child must wear closed shoes protect the ingrown toenail as follows:
- Inner Edge of Toe. If the inner edge of the big toe is involved, try this technique. Tape a cotton ball or foam pad between the lower part of the first and second toes. This will keep the upper toes from touching.
- Outer Edge of Toe. If the outer edge is involved, use a cotton ball. Tape it to the outside of the lower toe.
- This will keep the toenail from touching the side of the shoe.
- Never wear tight, narrow, or pointed shoes.
-
Pain Medicine:
- To help with the pain, give an acetaminophen product (such as Tylenol).
- Another choice is an ibuprofen product (such as Advil).
- Use as needed.
-
Prevention - Nail Trimming:
- Cut your child's toenails straight across so you can see the corners. Use a nail clipper.
- Do not round off corners. Keep the corners visible.
- Do not cut them too short.
- After baths or showers, the nails are soft. Bend the corners of the toenails upward.
-
Prevention - Wear Shoes That Fit:
- Make sure that your child's shoes are not too narrow. Give away any pointed or tight shoes.
- Tight narrow shoes are the most common cause of ingrown toenails.
- Shoes should have a wide toe box. The toes should not feel cramped.
-
What to Expect:
- With treatment, the pus should be gone in 48 hours.
- Pain should be gone in 1 week.
- Area should be healed up in 2 weeks.
-
Call Your Doctor If:
- Spreading redness or fever occur
- Pus pocket occurs
- Not improved after 7 days
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.
Tooth Injury
Is this your child's symptom?
- Injury to a tooth
Types of Tooth Injuries
- Loosened Tooth. May bleed a little from the gums. Usually tightens up on its own.
- Displaced Tooth. Usually pushed inward. Needs to be seen.
- Chipped Tooth. Minor fracture with small corner of tooth missing tooth. The fracture goes to the dentin (yellow color), not the pulp (red color). Not painful. See dentist during office hours.
- Fractured Tooth. The fracture goes down to the pulp. The pulp is where the blood supply and nerves to the tooth are located. The main finding is a red dot or bleeding in the center of the tooth. Very painful. Needs a root canal to save the tooth.
- Knocked-Out Permanent Tooth. Also called an avulsed tooth. A dental emergency. Needs to be re-implanted within 2 hours.
- Knocked-Out Baby Tooth. It cannot be re-implanted. See during dental office hours.
Symptoms
- The main symptom is pain.
- Minor bleeding from the gums may occur.
When to Call for Tooth Injury
Self Care at Home
|
Self Care at Home
- Minor tooth injury
Care Advice for Minor Dental Injuries
-
Cold for Pain:
- For pain, put a piece of ice or a popsicle on the injured gum.
- You can also use a cold pack on the cheek.
- Apply for 20 minutes.
-
Pain Medicine:
- To help with the pain, give an acetaminophen product (such as Tylenol).
- Another choice is an ibuprofen product (such as Advil).
- Use as needed.
-
Soft Diet:
- For any loose teeth, offer a soft diet.
- Avoid foods that need much chewing.
- You can go back to a normal diet after 3 days. By then, the tooth should be tightened up.
-
What to Expect:
- Tooth pain most often goes away in 2 or 3 days.
-
Call Your Dentist If:
- Pain becomes severe
- Cold fluids cause tooth pain
- Tooth turns a darker color
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.
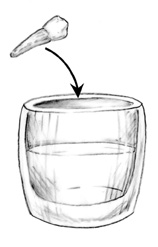
- To save the tooth, it must be put back in its socket as soon as possible. 2 hours is the outer limit for survival. Right away is best. If more than 30 minutes away from dental care, try to replace the tooth. Put it back in the socket before going to the dentist. Use the method below:
- Rinse off the tooth with saliva or water (do not scrub it).
- Replace the tooth into the socket, facing the correct way.
- Press down on the tooth with your thumb. Do this until the crown is level with the tooth next to it.
- Have your child bite down on a wad of cloth. This will help to keep the tooth in place until you can reach your dentist.
- Note: Baby teeth can't be re-implanted.
If not able to put the permanent tooth back in its socket, follow these instructions:
- It is very important to keep the tooth moist. Do not let it dry out.
- Transport the tooth in milk or saliva. Milk is best.
- Milk Transport Option 1 (best). Place the tooth in a small plastic bag with some milk. Put the plastic bag in a cup of ice.
- Milk Transport Option 2. Place the tooth in a cup of cold milk.
- Saliva Transport Option 1 - for Child 12 Years or Older. Put the tooth inside the child's mouth. Be careful not to swallow it.
- Saliva Transport Option 2. Put the tooth in a cup. Keep the tooth moist with child's saliva (spit).
Toothache
Is this your child's symptom?
- Pain or discomfort in a tooth
- Not caused by an injury
If NOT, try one of these:
Causes of a Toothache
- Tooth Decay. If the pain persists more than a day, this is the most common cause. A yellow-brown defect in the enamel may be seen. The most common site is the surface of one of the molars. The pain is dull.
- Dental Abscess. If the pain is severe and throbbing, the decay has become a tooth abscess. That means a pus pocket has formed within the root of the tooth. Tapping on the tooth causes increased pain. If not treated, the abscess will erode through the bone. A "gum boil" or pimple will be seen below the gum line. The patient needs to see a dentist for a root canal.
- Cracked Enamel. Biting on a hard object by mistake can crack a tooth. The tooth becomes sensitive to hot and cold liquids. The tooth may look normal. The fracture line may be below the gum line or just hard to see.
- Gum Disease. Gingivitis is a medical name for irritated gums. They are red and tender. If tooth brushing and flossing are ignored, the gums may even bleed. Can be very painful. Responds to getting the teeth cleaned and daily flossing.
- Stuck Food. Hard food may become wedged between 2 teeth. Proper flossing will remove the food and stop the pain.
Tooth Abscess and Severe Pain
- A tooth abscess can cause severe pain not controlled by normal pain medicines.
- Root canal therapy by an endodontist is needed to cure this problem.
- In the meantime, call your dentist's office. If you can't reach your dentist, call your doctor for advice. They can often bring the pain under control by calling in a prescription. Most often, this is for an antibiotic such as penicillin.
When to Call for Toothache
Self Care at Home
|
Self Care at Home
- Mild toothache present less than 24 hours
Care Advice for Mild Toothache
-
What You Should Know About Toothaches:
- Most toothaches don't last too long. They are due to a sensitive tooth.
- If the pain becomes worse or doesn't go away in 24 hours, call your dentist. The pain could be due to a small cavity.
- Here is some care advice that should help.
-
Floss:
- Floss on either side of the painful tooth to remove any wedged food.
-
Pain Medicine:
- To help with the pain, give an acetaminophen product (such as Tylenol).
- Another choice is an ibuprofen product (such as Advil).
- Use as needed.
-
Cold Pack for Pain:
- Put a cold pack or ice in a wet washcloth on the painful jaw. Do this for 20 minutes.
-
What to Expect:
- Most minor causes of toothache go away in less than a day.
-
Call Your Dentist If:
- Toothache lasts more than 24 hours
- The toothache gets worse
- You think your child needs to be seen
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.
Umbilical Cord Symptoms
Is this your child's symptom?
- Umbilical cord or navel questions about newborns
- The navel is also called the belly button or umbilicus
If NOT, try one of these:
Symptoms
- Umbilicus (navel) has a cloudy discharge or even some dried pus on the surface
- Bleeding occurs from cord's point of separation
- Separation of cord is delayed past 3 weeks
Omphalitis: Serious Complication
- Definition. Bacterial infection of the umbilical stump with spread to the skin around it. It's a medical emergency.
- How Often. 1 out of 200 newborns.
- Symptoms. Redness spreads around the navel. The area may be tender, swollen and have a foul odor.
Umbilical Granuloma: Minor Complication
- Definition. Small round growth in center of navel after the cord falls off. It's red. Covered with clear mucus. Not dry like normal skin.
- How Often. 1 out of 500 newborns.
- Outcome. Usually grows in size if not treated. Can become an entry point for umbilical infections.
- Treatment. Easily treated in the doctor's office by putting on a chemical called silver nitrate.
Dry Cord Care or Alcohol Cord Care
- The AAP and ACOG both advise dry cord care (natural drying). (Guidelines for Perinatal Care, 2012). It has become common practice in US hospitals.
- The book advises against using alcohol for routine umbilical cord care.
- Alcohol cord care is advised in less developed countries with high infection rates.
When to Call for Umbilical Cord Symptoms
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Self Care at Home
|
Call Doctor or Seek Care Now
- Age less than 1 month old and looks or acts abnormal in any way
- Bleeding won't stop after 10 minutes of direct pressure applied twice
- Spot of blood more than 2 inches (5 cm) across
- Red streak runs from the navel
- Red skin spreads from around the navel
- Age less than 12 weeks old with fever. Caution: do NOT give your baby any fever medicine before being seen.
- You think your child needs to be seen, and the problem is urgent
Call Doctor Within 24 Hours
- Small bleeding lasts more than 3 days
- Pimples, blisters or sores near navel
- Lots of drainage (such as urine, mucus, pus) from the navel
- You think your child needs to be seen, but the problem is not urgent
Call Doctor During Office Hours
- After using care advice for 3 days, navel is not dry and clean
- Small piece of red tissue inside the navel
- Cord stays attached more than 6 weeks
- You have other questions or concerns
Self Care at Home
- Normal cord care
- Normal navel care after cord falls off
- Minor infection of cord or navel
- Normal bleeding from cord or navel
- Normal delayed separation of the cord after 3 weeks
Care Advice
Treatment for Normal Umbilical Cord
-
What You Should Know About Normal Umbilical Cords:
- Normal cords don't need any special treatment.
- Just keep them dry (called dry cord care or natural drying).
- Reason: Cords need to dry up, before they will fall off.
- As they dry up, cords normally change color. They go from a shiny yellowish hue, to brown or grey.
- The cord will normally fall off between 1 and 3 weeks.
- Here is some care advice that should help.
-
Normal Dry Cord Care:
- Check the skin around the base of the cord once a day.
- Usually the area is dry and clean. No treatment is needed.
- If there are any secretions, clean them away. Use a wet cotton swab. Then dry carefully.
- You will need to push down on the skin around the cord to get at this area. You may also need to bend the cord a little to get underneath it.
- Caution: Don't put alcohol or other germ killer on the cord. Reason: Dry cords fall off sooner. (Exception: instructed by your doctor to use alcohol).
-
Bathing:
- Keep the cord dry. Avoid tub baths.
- Use sponge baths until the cord falls off.
-
Fold Diaper Down:
- Keep the area dry to help healing.
- To provide air contact, keep the diaper folded down below the cord.
- Another option for disposable diapers is to cut off a wedge with a scissors. Then seal the edge with tape.
-
Poop on Cord:
- Getting some poop on the cord or navel is not serious.
- If it occurs, clean the area with soap and water.
- This should prevent any infections.
-
Call Your Doctor If:
- Develops a red streak or redness around belly button
- Fever occurs
- Your baby starts to look or act abnormal
- You think your child needs to be seen
Treatment for Normal Navel After Cord Falls Off
-
What You Should Know About Navels After the Cord Falls Off:
- The cord can't fall off too early.
- The average cord falls off between 10 and 14 days. Normal range is 7 to 21 days. Even if it falls off before 7 days, you can follow this advice.
- After the cord has fallen off, the navel will gradually heal.
- It's normal for the center to look red at the point of separation.
- It's not normal if the redness spreads on to the belly.
- It's normal for the navel to ooze some secretions.
- Sometimes the navel forms a scab. Let it heal up and fall off on its own.
- The navel has a small risk of becoming infected.
- Here is some care advice that should help.
-
Normal Navel Care:
- Keep the navel (belly button) clean and dry.
- If there are any secretions, clean them away. Use a wet cotton swab. Then dry carefully.
- Do this gently to prevent any bleeding.
- Caution: Don't use any rubbing alcohol. Reason: can interfere with healing.
-
Bathing:
- After the cord falls off, continue sponge baths for a few more days.
- Help the belly button area dry up.
- Then, tub baths will be fine.
-
Fold Diaper Down:
- Keep the navel dry to help healing.
- To provide air contact, keep the diaper folded down below the navel.
- What to Expect: The belly button should be healed and dry by 7 days.
-
Call Your Doctor If:
- Develops a red streak or redness around belly button
- Fever occurs
- Cloudy discharge occurs
- Your baby starts to look or act abnormal
- You think your child needs to be seen
Treatment for Minor Infection of Cord or Navel
-
What You Should Know About a Minor Infection of Cord or Navel:
- The belly button will ooze secretions for several days.
- Normal secretions are clear or blood tinged mucus.
- A cloudy discharge is usually a mild infection.
- This can be from normal skin bacteria.
- A small amount of pus may be present.
- Here is some care advice that should help.
-
Clean the Navel:
- Clean the navel (belly button) 2 times a day.
- Use a wet cotton swab or cloth.
- Clean away any dried secretions or pus.
- Do this gently to prevent any bleeding.
- Caution: Don't use any rubbing alcohol. Reason: Can interfere with healing.
-
Antibiotic Ointment for Pus:
- If any pus is present, use an antibiotic ointment (such as Polysporin).
- No prescription is needed.
- Put a tiny amount on the belly button.
- Do this 2 times per day after the area has been cleaned.
- Do this for 2 days. After that, use the antibiotic ointment only if you see more pus.
-
Bathing:
- Do not use tub baths until the cord falls off. The navel should be well healed.
-
Fold Diaper Down:
- Keep the belly button dry to help healing.
- To provide air contact, keep the diaper folded down. Keep it below the cord and belly button.
-
What to Expect:
- With treatment, the cloudy discharge and pus should be gone in 2 to 3 days.
- The navel should become dry and healed by 7 days.
-
Call Your Doctor If:
- Develops a red streak or redness around the belly button
- Fever occurs
- Cloudy discharge not gone after 3 days of using this care advice
- Your baby starts to look or act abnormal
- You think your child needs to be seen
Treatment for Normal Bleeding Around Cord
-
What You Should Know About Mild Bleeding Around the Cord:
- A few drops of blood are normal when the cord falls off or catches on something.
- The diaper rubbing against the belly button may make it start up again.
- Here is some care advice that should help.
-
Bleeding:
- To stop bleeding, put direct pressure on the navel for 10 minutes. Use a clean cloth.
- Clean the area beforehand, rather than afterwards.
- Reason: This helps prevent bleeding from starting back up.
-
Diaper:
- Prevent the diaper from rubbing on the belly button.
- Do this by folding the diaper down away from the belly button.
- You can also cut a wedge out of the diaper.
-
What to Expect:
- The bleeding may come back a few times.
- It should only be a small smear of blood.
- The bleeding site should heal up by 2 days.
-
Call Your Doctor If:
- Bleeding gets worse
- Few drops of blood lasts more than 3 days
- Your baby starts to look or act abnormal
- You think your child needs to be seen
Treatment for Normal Delayed Separation of the Cord Beyond 3 Weeks
-
What You Should Know Cords Falling Off:
- Most cords fall off between 10 and 14 days. Normal range is 7 to 21 days.
- All cords slowly fall off on their own.
- Continue to be patient.
- Here is some care advice that should help.
-
Stop Alcohol:
- If you have been using rubbing alcohol to the cord, stop doing so.
- Rubbing alcohol can kill the good bacteria that help the cord fall off.
-
Diaper:
- Help the cord dry up faster by keeping the diaper folded below it.
- Another approach is to cut out a wedge of the diaper (if disposable).
- Air contact helps the cord stay dry.
-
Call Your Doctor If:
- Cord starts to look infected
- Fever occurs
- Cord is still on for more than 6 weeks
- Your baby starts to look sick or act abnormal
- You think your child needs to be seen
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.
Urinary Tract Infection - Female
Is this your child's symptom?
- Your child was diagnosed with a urinary tract infection (UTI)
- The most common UTI is a bacterial infection of the bladder. The medical name is cystitis.
- Your child is taking an antibiotic for the UTI
- You are worried that the fever or pain is not getting better fast enough
If NOT, try one of these:
Symptoms of UTI
- Pain, burning or stinging when passing urine
- Suspect pain if a young child starts to cry while passing urine
- The feeling of "can't wait" to pass urine may occur. This is called urgency.
- Passing small amounts of urine at a time often. This is called frequency.
- New onset of day or night -time wetting
- Pain in the lower tummy may also occur. If the kidney is infected, the pain is in the flank. The flank is the side right below the ribs.
- UTIs are a common cause of fevers without other symptoms in young children.
- The urine may be cloudy and have a bad odor. Sometimes, there is some blood in the urine.
Causes of UTI
- UTIs are caused by bacteria that travel up the urethra into the bladder. The opening of the urethra is just above the vagina.
- The vulva is the area outside the vagina. Soaps can cause this area to be red, sore and itchy. This can lead to UTIs. Stool that gets on the vulva is another big factor. This can happen with careless wiping. It can also happen with constipation.
- A rare cause is if the bladder isn't emptied all the way. Reason: Urine that stays in the bladder too long can become infected.
- Cystitis is more common in girls than boys. This is due to the much shorter length of the urethra in girls.
Diagnosis of UTI
- A clean catch urine sample needs to be tested. A UTI is confirmed by finding white blood cells in the urine. A positive culture for bacteria is also needed.
When to Call for Urinary Tract Infection - Female
Call 911 Now
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Self Care at Home
|
Call 911 Now
- Not moving or too weak to stand
- You think your child has a life-threatening emergency
Call Doctor or Seek Care Now
- Side (flank) or lower back pain and new onset since starting antibiotic
- Stomach, side or back pain and worse since starting antibiotic
- Vomited 2 or more times and interferes with taking antibiotic
- Fever over 104° F (40° C)
- Shaking chills
- Age less than 1 year and any symptoms worse
- Taking antibiotic more than 24 hours and you think your child is worse
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Call Doctor Within 24 Hours
- Blood in urine and new onset since starting antibiotic
- Taking antibiotic more than 24 hours, and pain with passing urine is severe. (Plus the pain is not better 2 hours after taking pain medicine)
- Taking antibiotic more than 48 hours and fever still there or comes back
- Taking antibiotic more than 3 days and pain not better
- You think your child needs to be seen, but the problem is not urgent
Call Doctor During Office Hours
- You have other questions or concerns
Self Care at Home
- Bladder infection on antibiotic with no other problems
- Questions about prevention of bladder infections
Care Advice
Treatment for a Bladder Infection
-
What You Should Know about Bladder Infections:
- Bladder infections are common in girls.
- Most infections do not respond to the first dose of an antibiotic.
- Often the bladder symptoms do not improve the first day.
- Here is some care advice that should help.
-
Keep Giving the Antibiotic by Mouth:
- UTIs need a prescription antibiotic. It will kill the bacteria that are causing the bladder infection.
- Give it as directed.
- Try not to forget any of the doses.
- Give the antibiotic until it is gone. Reason: To keep the bladder infection from flaring up again.
-
Pain Medicine:
- For pain when passing urine, give a pain medicine.
- You can use an acetaminophen product (such as Tylenol).
- Another choice is an ibuprofen product (such as Advil).
- Use as needed.
-
Fever Medicine:
- For fevers above 102° F (39° C), give an acetaminophen product (such as Tylenol).
- Another choice is an ibuprofen product (such as Advil).
- Note: Fevers less than 102° F (39° C) are important for fighting infections.
- For all fevers: Keep your child well hydrated. Give lots of cold fluids.
-
Give More Fluids:
- Give extra fluids to drink. Cranberry juice may be helpful.
- Reason: Fluids dilute the urine so that it does not sting.
-
Baking Soda Baths - For Young Girls:
- Soak for 10 minutes to remove germs and to help with healing.
- Add 2 ounces (60 mL) baking soda per tub of warm water.
- Reason: Baking soda is better than vinegar for young girls.
- During soaks, be sure she spreads her legs. This allows the water to cleanse the genitals.
- Repeat baking soda soaks 2 times per day for 2 days.
-
Vinegar Warm Water Soaks - For Older Girls After Puberty:
- Soak the genital area for 10 minutes to remove irritants and decrease pain.
- Add 2 ounces (60 mL) vinegar per tub of warm water. Reason: After puberty, vinegar water matches the normal acid level of the vagina.
- During soaks, be sure she spreads her legs. This allows the water to clean the genital area.
- Repeat vinegar water soaks once per day until is better.
-
Young Girls - Avoid Soaps:
- Avoid bubble bath, soap, and shampoo to the vulva. Reason: They are irritants and can lead to a UTI.
- Only use warm water to clean the vulva area.
-
What to Expect:
- Fever is usually gone in 48 hours.
- Pain and burning are often much better in 48 hours.
- Frequency (passing small amounts of urine often) is also usually better in 48 hours.
- Bladder infections occur more than once in 10% of girls.
- For any future fever without other symptoms, call your doctor's office. Your child should be seen for a urine check.
-
Return to School:
- Bladder infections cannot be spread to others.
- Your child does not need to miss any school or child care.
-
Call Your Doctor If:
- Pain when passing urine becomes severe
- Fever lasts over 48 hours after starting the antibiotic
- Vomiting and can't keep down the antibiotic
- You think your child needs to be seen
- Your child becomes worse
Prevention of Bladder Infections in Girls
-
Tips for How to Prevent UTIs in Girls:
- When your child bathes, clean the genital area with warm water. Soap is not needed for young girls.
- Don't use bubble bath, shampoo or other soaps in the bath water. Reason: They are irritants.
- Keep bath time less than 10 minutes. Your child also should pass urine right after baths.
- Teach your daughter to wipe herself correctly from front to back after a stool.
- Drink enough fluids each day to keep the urine light-colored.
- Pass urine at least every 4 hours during the day and avoid "holding back."
- Wear cotton panties. Reason: To allow the skin to breathe. Your child doesn't need to wear panties during the night.
- Avoid constipation.
-
Call Your Doctor If:
- You have other questions or concerns
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.
Urination Pain - Female
Is this your child's symptom?
- Pain, burning or stinging when passing urine
- Female
- Also, suspect pain if your young child starts to cry while passing urine
- The feeling of "can't wait" to pass urine may occur. This is called urgency.
- Passing small amounts of urine (a few drops) at a time may also occur. This is called frequency.
- Not caused by an injury to the genitals
If NOT, try one of these:
Causes of Pain Passing Urine
- Soap Vulvitis. Bubble bath, shampoo or soap in bath water is the main cause in young girls. Can cause the genital area to become red and sore. This is called "soap vulvitis." It can cause pain when passing urine. Using a soapy washcloth can also be the cause. Vaginal itching or redness can also occur.
- Bladder or Kidney Infections (urinary tract infections) are possible at any age. It can be diagnosed by checking a urine sample.
- Labial Fusion. (Also called labial adhesions.) This is when the vaginal lips or folds are stuck together. The vaginal opening looks closed off. Labia that are closed more than half way can collect soap or stool. The main symptom is itching in this area. It can also cause pain when passing urine.
When to Call for Urination Pain - Female
Call 911 Now
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
|
Call 911 Now
- Not moving or too weak to stand
- You think your child has a life-threatening emergency
Call Doctor or Seek Care Now
- Blood in urine
- Severe pain when passing urine
- Fever is present
- Stomach, side or back pain
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Call Doctor Within 24 Hours
- Painful to pass urine, but none of the symptoms above. Reason: could be a bladder infection.
Care Advice for Pain When Passing Urine
-
What You Should Know:
- In young girls, soap is the most common cause of pain with passing urine.
- To rule out a bladder infection, she needs to have her urine checked.
- Here is some care advice that should help, until you talk with your doctor.
-
Baking Soda Baths - Young Girls Only:
- Soak for 10 minutes to remove germs and to help with healing.
- Add 2 ounces (60 mL) baking soda per tub of warm water.
- Reason: Baking soda is better than vinegar for young girls.
- During soaks, be sure she spreads her legs. This allows the water to cleanse the genitals.
- Repeat baking soda soaks 2 times per day for 2 days.
-
Do Not Use Soaps - Young Girls Only:
- Do not use bubble bath, soap and shampoo in the bath water. They can cause the genitals to be red, sore or itchy. This is the most common cause of pain with passing urine in young girls.
- Only use warm water to cleanse the genitals.
- Baby oil can be used to remove any dried body fluids.
- After puberty, soap can be used.
-
Vinegar - Warm Water Soaks - Girls After Puberty:
- Soak the genital area for 10 minutes to remove germs and irritants.
- Add 2 ounces (60 mL) vinegar per tub of warm water.
- Reason: After puberty, vinegar water matches the normal acidity of the vagina.
- During soaks, be sure she spreads her legs. Reason: This allows the water to cleanse the genital area.
- Repeat vinegar water soaks once per day until seen.
-
Fluids - Offer More:
- Give extra fluids to drink.
- Reason: Dilutes the urine so that it does not sting.
-
Pain Medicine:
- For pain when passing urine, give a pain medicine.
- You can use an acetaminophen product (such as Tylenol).
- Another choice is an ibuprofen product (such as Advil).
- Use as needed.
-
Return to School:
- Even if your child has a bladder infection, it cannot be spread to others.
- Your child does not need to miss any school or child care.
-
What to Expect:
- If soap is the cause, the pain should go away within 24 hours.
- Itching or skin redness may last 2 days.
-
Call Your Doctor If:
- Pain when passing urine becomes severe
- Fever occurs
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.
Urination Pain - Male
Is this your child's symptom?
- Pain, burning or stinging when passing urine
- Male
- Also, suspect pain if your young child starts to cry while passing urine
- The feeling of "can't wait" to pass urine may occur. This is called urgency.
- Passing small amounts of urine (a few drops) at a time may also occur. This is called frequency.
- Not caused by an injury to the genitals
If NOT, try one of these:
Causes of Pain Passing Urine
- Any boy who has pain when passing urine needs his urine checked. Sometimes in young boys, the urine is normal.
- Meatitis. This means redness at the opening of the penis. It may have a sore or scab on it. Passing urine is painful. It occurs in boys who are circumcised. Can be caused by any irritant, such as bubble bath. Sometimes, the opening becomes infected with a bacteria, such as Strep.
- Foreskin Infection. This means an infection under the foreskin. The main symptom is a red and tender foreskin. Pus may also ooze out of the foreskin opening. Passing urine is painful. It occurs in boys who are not circumcised.
- Urethral Injury (Serious). The urethra passes through the entire penis. It can be injured by any straddle injury, such as falling on the crossbar of a bike. It can be bruised or torn. The main symptoms are bloody urine and pain when passing urine. There may be a bruise on the shaft of the penis. Some boys don't report an injury to the penis or scrotum.
- Bladder or Kidney Infections (urinary tract infections) are possible at any age. They are not common in boys.
- STI. In teens, pain when passing urine can be from diseases spread during sex.
When to Call for Urination Pain - Male
Call 911 Now
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
|
Call 911 Now
- Not moving or too weak to stand
- You think your child has a life-threatening emergency
Call Doctor or Seek Care Now
- Blood in urine
- Severe pain when passing urine
- Fever is present
- Stomach, side or back pain
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Call Doctor Within 24 Hours
- Painful to pass urine, but none of the symptoms above. Reason: could be a bladder infection.
Care Advice for Pain When Passing Urine
-
What You Should Know About Pain When Passing Urine:
- In boys, pain when passing urine is not common.
- Most of them need a urine sample tested for a bladder infection.
- Here is some care advice that should help, until you talk with your doctor.
-
Do Not Use Soaps - Young Boys Only:
- Do not use bubble bath, soap and shampoo in the bath water. They can cause the penis opening to be red and sore.
- Only use warm water to cleanse the head of the penis.
- After puberty, soap can be used.
-
Fluids - Offer More:
- Give extra fluids to drink.
- Reason: Dilutes the urine so that it does not sting.
-
Pain Medicine:
- For pain when passing urine, give a pain medicine.
- You can use an acetaminophen product (such as Tylenol).
- Another choice is an ibuprofen product (such as Advil).
- Use as needed.
-
Return to School:
- Even if your child has a bladder infection, it cannot be spread to others.
- Your child does not need to miss any school or child care.
-
What to Expect:
- If soap is the cause, the pain should go away within 24 hours.
- Itching or skin redness may last 2 days.
-
Call Your Doctor If:
- Pain when passing urine becomes severe
- Fever occurs
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.
Vaginal Symptoms
Is this your child's symptom?
- Genital symptoms in young girls (before puberty)
- Symptoms include pain, itching, discharge, bleeding and rashes
- Vulva itching and irritation from soap is the most common problem
- Symptoms not caused by an injury
If NOT, try one of these:
Symptoms Covered in this Topic
- Vaginal symptoms include discharge, bleeding and pain
- Vulva symptoms include itching, pain and pain when passing urine
- Genital area skin symptoms include itching, pain, rash and swelling
Causes of Genital Symptoms in Young Girls
- Soap Vulvitis. The vulva is the area outside the vagina. Soaps can cause this area to be red, sore and itchy. Bubble baths are the most common cause of genital itching.
- Poor Hygiene. Not rinsing the genitals at all can also cause itching. Any stool left on the vulva is very irritating. This can happen with loose stools or back to front wiping. It's also seen in children who leak stool because they are blocked up. Traces of sand or dirt may do the same.
- Yeast Vulvitis. Yeast infections of the female genital area are rare before the teen years. They do occur in girls who are still wearing diapers. They can happen after a course of antibiotics. They can also happen in girls with diabetes.
- Labial Fusion. (Also called labial adhesions.) This is when the vaginal lips or folds are stuck together. The vaginal opening looks closed off. Labia that are closed more than half way can collect soap or stool. The main symptom is itching in this area.
- Pinworms. Sometimes, an adult pinworm will travel into the vagina. The pinworm's secretions are very irritating. This leads to intense itching.
- Vaginitis. Vaginitis is a bacterial infection of the vagina. The main symptom is a yellow discharge. The most common cause is Strep, the same one that causes bad sore throats. Vaginal discharge from STIs (sexually transmitted infections) is not common before the teen years.
- Vaginal Foreign Object. Young girls may put an object (such as a bead) in the vagina. This can be part of normal behavior as young girls explore their bodies. It will cause a bad-smelling discharge. If the object is sharp, the discharge will be blood-tinged.
- Bladder Infection. These are common in young girls because the urethra is so short. The main symptom is pain or burning when passing urine.
- Skin Rash. Most skin rashes are from contact with some irritant. The irritant is often on dirty hands. The cause is from not washing them before using the toilet.
- Serious Cause: Sexual Abuse. Suspect for any symptoms that are strange or not explained.
Soap Vulvitis
- Soap is the most common cause of genital itching in young girls. It can also cause the area to become red and sore. This is called soap or chemical vulvitis.
- The vulva is very sensitive to the drying effect of soaps.
- Sitting for a long time in a bubble bath is the main cause.
- Shampoo or soap in the bath water can also cause redness and itching. So can washing the genitals with a soapy washcloth.
- In young girls, the inner female genitals should only be washed with warm water. The skin around the genitals can be washed with soap.
- Soap vulvitis only occurs in young girls before puberty. Breast buds are the first sign of puberty. This diagnosis is easy if young girls are using bubble bath.
When to Call for Vaginal Symptoms
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Self Care at Home
|
Call Doctor or Seek Care Now
- Could have been caused by sexual abuse
- Vaginal bleeding
- Severe genital pain
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Call Doctor Within 24 Hours
- Vaginal discharge
- Fever is present
- Pain or burning when passing urine
- Vaginal pain
- Vaginal foreign object suspected
- Genital area looks infected (such as spreading redness, draining sore)
- You think your child needs to be seen, but the problem is not urgent
Call Doctor During Office Hours
- Puberty has started. Reason: soap vulvitis is not the cause.
- Vaginal itching lasts more than 2 days using this care advice
- Vaginal itching is a frequent problem
- Mild rash of genital area present 3 or more days using this care advice
- You have other questions or concerns
Self Care at Home
- Soap vulvitis suspected
- Mild skin rash of genital area
Care Advice
Soap Vulvitis - Treatment
-
What You Should Know About Soap Vulvitis:
- Genital itching in young girls is most often caused by soap (especially bubble bath). The vulva area is sensitive to the drying effect of soap.
- Only clean the genitals with warm water.
- After puberty, soap can be tolerated.
- Here is some care advice that should help.
-
Baking Soda Baths - Young Girls Only:
- Soak for 10 minutes to remove germs and to help with healing.
- Add 2 ounces (60 mL) baking soda per tub of warm water.
- Reason: Baking soda is better than vinegar for young girls.
- During soaks, be sure she spreads her legs. This allows the water to cleanse the genitals.
- Repeat baking soda soaks 2 times per day for 2 days.
-
Steroid Cream for Itching:
- Put a tiny amount of 1% hydrocortisone cream (such as Cortaid) on the genitals.
- No prescription is needed.
- Use after soaks for 1 or 2 days. Do not use more than 2 days.
-
Prevention - Do Not Use Soaps:
- Do not use bubble bath, soap and shampoo in the bath water. They can cause the genitals to be red, sore or itchy.
- Only use warm water to cleanse the genitals.
- Baby oil can be used to remove any dried body fluids.
- After puberty, soap can be used.
-
What to Expect:
- If soap is the cause, symptoms should go away within 2 days.
-
Call Your Doctor If:
- Itching lasts over 48 hours using this care advice
- Vaginal discharge or bleeding occurs
- Passing urine becomes painful
- You think your child needs to be seen
- Your child becomes worse
Mild Skin Rash near Genital Area - Treatment
-
What You Should Know about Genital Rashes:
- Rashes can be caused by skin irritants. The hand may touch the genital area when passing urine. Rashes are commonly from an irritant that was on the hands.
- Examples are a plant (such as an evergreen) or chemicals (such as bug repellents). Fiberglass, pet saliva or even food can also be irritants.
- Most small rashes can be treated at home.
- Here is some care advice that should help.
-
Clean the Area:
- Wash the area once with soap to remove any irritants.
-
Steroid Cream for Itching:
- For itchy rashes, use 1% hydrocortisone cream (such as Cortaid). No prescription is needed.
- Do this 2 times per day for a few days.
-
Antibiotic Ointment for Infections:
- For any cuts, sores or scabs that look infected, put on an antibiotic ointment. An example is Polysporin. No prescription is needed.
- Use 2 times per day until seen.
-
What to Expect:
- Small rashes from irritants should go away in 2 days with treatment.
-
Prevention of Rashes:
- Teach your daughter to wash her hands if they are dirty.
- Have her clean her hands before touching her genital area.
-
Call Your Doctor If:
- Rash spreads or gets worse
- Rash lasts more than 3 days
- Fever occurs
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.
Vomiting With Diarrhea
Is this your child's symptom?
- Vomiting and diarrhea occur together
- Vomiting is the forceful emptying (throwing up) of what is in the stomach
- It's normal for nausea (upset stomach) to come before each bout of vomiting
- Diarrhea means 2 or more watery or very loose stools. Reason: 1 loose stool can be normal.
- If vomiting is done, use the Diarrhea care guide.
If NOT, try one of these:
Causes of Vomiting with Diarrhea
- Viral Gastroenteritis. GI infection from a virus is the most common cause. A common agent is the Rotavirus. The illness starts with vomiting. Watery loose stools follow within 12-24 hours. On cruise ship outbreaks, the most common viral cause is Norovirus.
- Food Poisoning. This causes rapid vomiting and diarrhea within hours after eating the bad food. Caused by toxins from germs growing in foods left out too long. An example is Staph toxin in egg salad.
- Traveler's Diarrhea. Caused by germs in food or drink. Suspect this if it follows recent foreign travel.
- Bacterial GI Infection. Diarrhea can also be caused by some bacteria. Most bacterial diarrhea goes away on its own. A few can cause a severe large bowel infection (such as Shigella colitis).
- Serious Complication: Dehydration. This is the health problem where the body has lost too much fluid. (See below for more on this).
Vomiting Scale
- Mild: 1 - 2 times/day
- Moderate: 3 - 7 times/day
- Severe: Vomits everything, nearly everything or 8 or more times per day
- Severity relates even more to how long the vomiting goes on for. At the start of the illness, it's common to vomit everything. This can last for 3 or 4 hours. Children then often become stable and change to mild vomiting.
- The main risk of vomiting is dehydration. Dehydration means the body has lost too much fluid.
- Watery stools with vomiting carry the greatest risk for causing dehydration.
- The younger the child, the greater the risk for dehydration.
Diarrhea Scale
- Mild: 2-5 watery stools per day
- Moderate: 6-10 watery stools per day
- Severe: Over 10 watery stools per day
- The main risk of diarrhea is dehydration.
- Frequent, watery stools can cause dehydration.
- Loose or runny stools do not cause dehydration.
Dehydration: How to Know
- Dehydration means that the body has lost too much fluid. This can happen with vomiting and/or diarrhea. A weight loss of more than 3% is needed. Mild diarrhea or mild vomiting does not cause this. Neither does a small decrease in fluid intake.
- Vomiting with watery diarrhea is the most common cause of dehydration.
- Dehydration is a reason to see a doctor right away.
- These are signs of dehydration:
- Decreased urine (no urine in more than 8 hours) happens early in dehydration. So does a dark yellow color. If the urine is light straw colored, your child is not dehydrated.
- Dry tongue and inside of the mouth. Dry lips are not helpful.
- Dry eyes with decreased or absent tears
- In babies, a sunken soft spot
- Slow blood refill test: Longer than 2 seconds. First, press on the thumbnail and make it pale. Then let go. Count the seconds it takes for the nail to turn pink again. Ask your doctor to teach you how to do this test.
- Fussy, tired out or acting ill. If your child is alert, happy and playful, he or she is not dehydrated.
- A child with severe dehydration becomes too weak to stand. They can also be very dizzy when trying to stand.
When to Call for Vomiting With Diarrhea
Call 911 Now
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Self Care at Home
|
Call 911 Now
- Can't wake up
- Not moving or too weak to stand
- You think your child has a life-threatening emergency
Call Doctor or Seek Care Now
- Dehydration suspected. No urine in more than 8 hours, dark urine, very dry mouth and no tears.
- Blood in the stool
- Stomach pain when not vomiting. Exception: stomach pain or crying just before vomiting is quite common.
- Age less than 12 weeks old with vomiting 2 or more times. Exception: normal spitting up.
- Age less than 12 months old and vomited Pedialyte 3 or more times
- Severe vomiting (vomits everything) for more than 8 hours while getting clear fluids
- Weak immune system. Examples are: sickle cell disease, HIV, cancer, organ transplant, taking oral steroids.
- Vomiting a prescription medicine
- Fever over 104° F (40° C)
- Age less than 12 weeks old with fever. Caution: do NOT give your baby any fever medicine before being seen.
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Call Doctor Within 24 Hours
- Age less than 1 year with vomiting
- Has vomited for more than 24 hours
- Fever lasts more than 3 days
- You think your child needs to be seen, but the problem is not urgent
Call Doctor During Office Hours
- Vomiting is a frequent problem
- You have other questions or concerns
Self Care at Home
- Mild or moderate vomiting with diarrhea
Care Advice for Vomiting with Diarrhea
-
What You Should Know About Vomiting With Diarrhea:
- Most vomiting is caused by a viral infection of the stomach. Sometimes, mild food poisoning is the cause.
- Throwing up is the body's way of protecting the lower intestines.
- Diarrhea is the body's way of getting rid of the germs.
- When vomiting and diarrhea occur together, treat the vomiting. Don't do anything special for the diarrhea.
- The main risk of vomiting is dehydration. Dehydration means the body has lost too much fluid.
- Here is some care advice that should help.
-
Formula Fed Babies - Give Oral Rehydration Solution (ORS) for 8 Hours:
- If your child vomits more than once, offer ORS for 8 hours. If you don't have ORS, use formula until you can get some.
- ORS is a special fluid that can help your child stay hydrated. You can use Pedialyte or the store brand of ORS. It can be bought in food stores or drug stores.
- Spoon or syringe feed small amounts. Give 1-2 teaspoons (5-10 mL) every 5 minutes.
- After 4 hours without throwing up, double the amount.
- Return to Formula. After 8 hours without throwing up, go back to regular formula.
-
Breastfed Babies - Reduce the Amount Per Feeding:
- If vomits more than once, nurse for 5 minutes every 30 to 60 minutes. After 4 hours without throwing up, return to regular nursing.
- If continues to vomit, switch to pumped breastmilk. ORS is rarely needed in breastfed babies. It can be used if vomiting becomes worse.
- Spoon or syringe feed small amounts of pumped milk. Give 1-2 teaspoons (5-10 mL) every 5 minutes.
- After 4 hours without throwing up, return to regular feeding at the breast. Start with small feedings of 5 minutes every 30 minutes. As your baby keeps down the smaller amounts, slowly give more.
-
Older Children (over 1 Year Old), Offer Small Amounts of ORS For 8 Hours:
- ORS. Vomiting with watery diarrhea needs ORS (such as Pedialyte). If refuses ORS, use half-strength Gatorade. Make it by mixing equal amounts of Gatorade and water.
- The key to success is giving small amounts of fluid. Offer 2-3 teaspoons (10-15 mL) every 5 minutes. Older kids can just slowly sip ORS.
- After 4 hours without throwing up, increase the amount.
- After 8 hours without throwing up, go back to regular fluids.
- Avoid fruit juices and soft drinks. They make diarrhea worse.
-
Stop All Solid Foods:
- Avoid all solid foods and baby foods in kids who are vomiting.
- After 8 hours without throwing up, gradually add them back.
- Start with starchy foods that are easy to digest. Examples are cereals, crackers and bread.
-
Do Not Give Medicines:
- Stop using any drug that is over-the-counter for 8 hours. Reason: Some of these can make vomiting worse.
- Fever: Mild fevers don't need to be treated with any drugs. For higher fevers, you can use an acetaminophen suppository (such as FeverAll). This is a form of the drug you put in the rectum (bottom). Ask a pharmacist for help finding this product. Do not use ibuprofen. It can upset the stomach.
- Call your doctor if: Your child vomits a drug ordered by your doctor.
-
Return to School:
- Your child can return to school after the vomiting and fever are gone.
-
What to Expect:
- For the first 3 or 4 hours, your child may vomit everything. Then the stomach settles down.
- Moderate vomiting usually stops in 12 to 24 hours.
- Mild vomiting (1-2 times per day) with diarrhea may last a little longer. It can continue off and on for up to a week.
-
Call Your Doctor If:
- Vomits all clear fluids for more than 8 hours
- Vomiting lasts more than 24 hours
- Blood or bile (green color) in the vomit
- Stomach ache present when not vomiting
- Dehydration suspected (no urine in over 8 hours, dark urine, very dry mouth, and no tears)
- Diarrhea becomes severe
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.
Vomiting Without Diarrhea
Is this your child's symptom?
- Vomiting (throwing up) stomach contents
- It's normal for nausea (upset stomach) to come before each bout of vomiting
- Other names for vomiting are puking, barfing and heaving
If NOT, try one of these:
Causes of Vomiting
- Viral Gastritis. Stomach infection from a stomach virus is the most common cause. Also called stomach flu. A common cause is the Rotavirus. The illness starts with vomiting. Watery loose stools may follow within 12-24 hours.
- Food Poisoning. This causes rapid vomiting within hours after eating the bad food. Diarrhea may follow. Caused by toxins from germs growing in foods left out too long. An example is Staph toxin in egg salad.
- Ibuprofen. Ibuprofen products (such as Advil) can be a stomach irritant. If taken on an empty stomach, it can cause vomiting.
- Food Allergy. Vomiting can be the only symptom of a food reaction. The vomiting comes on quickly after eating the food. Common foods are peanuts, tree nuts, fish and shellfish (such as shrimp).
- Coughing. Hard coughing can also cause your child to throw up. This is more common in children with reflux.
- Motion Sickness. Vomiting and dizziness are triggered by motion. Sea sickness or fun-park ride sickness are the most common types. Strongly genetic.
- Migraine Headaches. In children, most migraine headaches also have vomiting.
- Serious Causes. Vomiting alone (without diarrhea) should stop within about 24 hours. If it lasts over 24 hours, you must think about more serious causes. Examples are appendicitis, a kidney infection, diabetes and head injury. A serious cause in young babies is pyloric stenosis. See below for more on this.
- Cyclic Vomiting. Cyclic vomiting is the most common cause of recurrent attacks of vomiting. Attacks have a sudden onset and offset. Often occur in children who later develop migraine headaches.
Pyloric Stenosis (Serious Cause)
- The most common cause of true vomiting in young babies.
- Onset of vomiting is age 2 weeks to 2 months
- Vomiting is forceful. It becomes projectile and shoots out.
- Right after vomiting, the baby is hungry and wants to feed. ("hungry vomiter")
- Cause: the pylorus is the channel between the stomach and the gut. In these babies, it becomes narrow and tight.
- Risk: weight loss or dehydration
- Treatment: cured by surgery.
Vomiting Scale
- Mild: 1 - 2 times/day
- Moderate: 3 - 7 times/day
- Severe: vomits everything, nearly everything or 8 or more times/day
- Severity relates even more to how long the vomiting goes on for. At the start of the illness, it's common for a child to vomit everything. This can last for 3 or 4 hours. Children then often become stable and change to mild vomiting.
- The main risk of vomiting is dehydration. Dehydration means the body has lost too much fluid.
- The younger the child, the greater the risk for dehydration.
Dehydration: How to Tell
- The main risk of vomiting is dehydration. Dehydration means the body has lost too much water.
- Vomiting with watery diarrhea is the most common cause of dehydration.
- Dehydration is a reason to see a doctor right away.
- Your child may have dehydration if not drinking much fluid and:
- The urine is dark yellow and has not passed any in over 8 hours.
- Inside of the mouth and tongue are very dry.
- No tears if your child cries.
- Slow blood refill test: longer than 2 seconds. First, press on the thumbnail and make it pale. Then let go. Count the seconds it takes for the nail to turn pink again. Ask your doctor to teach you how to do this test.
- A child with severe dehydration becomes too weak to stand. They can also be very dizzy when trying to stand.
When to Call for Vomiting Without Diarrhea
Call 911 Now
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Self Care at Home
|
Call 911 Now
- Can't wake up
- Not moving or too weak to stand
- You think your child has a life-threatening emergency
Call Doctor or Seek Care Now
- Headache
- Dehydration suspected. No urine in more than 8 hours, dark urine, very dry mouth and no tears.
- Stomach pain when not vomiting. Exception: stomach pain or crying just before vomiting is quite common.
- Diabetes suspected (drinking lots, frequent urine, weight loss)
- Kidney infection suspected (side or back pain, fever, painful to pass urine)
- Age less than 12 weeks old with vomiting 2 or more times. Exception: normal spitting up.
- Severe vomiting (vomits everything) more than 8 hours while getting clear fluids
- High-risk child (such as diabetes, stomach or head injury)
- Weak immune system. Examples are: sickle cell disease, HIV, cancer, organ transplant, taking oral steroids.
- Vomiting a prescription medicine
- Fever over 104° F (40° C)
- Age less than 12 weeks old with fever. Caution: do NOT give your baby any fever medicine before being seen.
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Call Doctor Within 24 Hours
- Age less than 1 year with vomiting
- Vomits for more than 24 hours
- Fever lasts more than 3 days
- Fever returns after being gone more than 24 hours
- You think your child needs to be seen, but the problem is not urgent
Call Doctor During Office Hours
- Vomiting is a frequent problem
- You have other questions or concerns
Self Care at Home
- Mild or moderate vomiting (most likely viral gastritis)
Care Advice for Vomiting without Diarrhea
-
What You Should Know About Vomiting Without Diarrhea:
- Most vomiting is caused by a viral infection of the stomach. Sometimes, mild food poisoning is the cause.
- Vomiting is the body's way of protecting the lower gut.
- The good news is that stomach illnesses last only a short time.
- The main risk of vomiting is dehydration. Dehydration means the body has lost too much fluid.
- Here is some care advice that should help.
-
Formula Fed Babies - Give Oral Rehydration Solution (ORS) for 8 Hours:
- If your child vomits more than once, offer ORS for 8 hours. If you don't have ORS, use formula until you can get some.
- ORS is a special fluid that can help your child stay hydrated. You can use Pedialyte or the store brand of ORS. It can be bought in food stores or drugstores.
- Spoon or syringe feed small amounts. Give 1-2 teaspoons (5-10 mL) every 5 minutes.
- After 4 hours without throwing up, double the amount.
- Return to Formula. After 8 hours without throwing up, go back to regular formula.
-
Breastfed Babies - Reduce the Amount Per Feeding:
- If vomits more than once, nurse for 5 minutes every 30 to 60 minutes. After 4 hours without throwing up, return to regular nursing.
- If continues to vomit, switch to pumped breastmilk. ORS is rarely needed in breastfed babies. It can be used if vomiting becomes worse.
- Spoon or syringe feed small amounts of pumped milk. Give 1-2 teaspoons (5-10 mL) every 5 minutes.
- After 4 hours without throwing up, return to regular feeding at the breast. Start with small feedings of 5 minutes every 30 minutes. As your baby keeps down the smaller amounts, slowly give more.
-
Older Children (over 1 Year Old) - Offer Small Amounts of Clear Fluids For 8 Hours:
- Water or ice chips are best for older children. Reason: Water is easily absorbed in the stomach.
- Other clear fluids: Use half-strength Gatorade. Make it by mixing equal amounts of Gatorade and water. Can mix apple juice the same way. ORS (such as Pedialyte) is usually not needed in older children. Popsicles work great for some kids.
- The key to success is giving small amounts of fluid. Offer 2-3 teaspoons (10-15 mL) every 5 minutes. Older kids can just slowly sip a clear fluid.
- After 4 hours without throwing up, increase the amount.
- After 8 hours without throwing up, return to regular fluids.
- Caution: If vomits over 12 hours, switch to ORS or half-strength Gatorade.
-
Stop All Solid Foods:
- Avoid all solid foods and baby foods in kids who are vomiting.
- After 8 hours without throwing up, gradually add them back.
- Start with starchy foods that are easy to digest. Examples are cereals, crackers and bread.
-
Do Not Give Medicines:
- Stop using any drug that is over-the-counter for 8 hours. Reason: Some of these can make vomiting worse.
- Fever. Mild fevers don't need to be treated with any drugs. For higher fevers, you can use an acetaminophen suppository (such as FeverAll). This is a form of the drug you put in the rectum (bottom). Ask a pharmacist for help finding this product. Do not use ibuprofen. It can upset the stomach.
- Call your doctor if: Your child vomits a drug ordered by your doctor.
-
Try to Sleep:
- Help your child go to sleep for a few hours.
- Reason: Sleep often empties the stomach and removes the need to vomit.
- Your child doesn't have to drink anything if his stomach feels upset and he doesn't have any diarrhea.
-
Return to School:
- Your child can return to school after the vomiting and fever are gone.
-
What to Expect:
- For the first 3 or 4 hours, your child may vomit everything. Then the stomach settles down.
- Vomiting from a viral illness often stops in 12 to 24 hours.
- Mild vomiting and nausea may last up to 3 days.
-
Call Your Doctor If:
- Vomits clear fluids for more than 8 hours
- Vomiting lasts more than 24 hours
- Blood or bile (green color) in the vomit
- Stomach ache present when not vomiting
- Dehydration suspected (no urine in over 8 hours, dark urine, very dry mouth, and no tears)
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.
Warts
Is this your child's symptom?
- Small raised growths that have a rough surface
- Viral infection of the skin
If NOT, try one of these:
Symptoms of Warts
- Raised, round, rough-surfaced growths on the skin
- Skin-colored or pink
- Most commonly occur on the hands, especially the fingers
- Not painful unless located on the sole of the foot (plantar wart). Also can be painful if on part of a finger used for writing.
Cause of Warts
- Warts are caused by several human papilloma viruses
- Different types of warts are caused by different papilloma viruses
Prevention of Spread to Others
- Avoid baths or hot tubs with other children. Reason: Warts can spread in warm water.
- Also, avoid sharing washcloths or towels.
- Contact sports: Warts can spread to other team members. Warts should be covered or treated.
- Time it takes to get warts after close contact: 3 months
When to Call for Warts
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Self Care at Home
|
Call Doctor or Seek Care Now
- Redness or red streak spreading from wart with fever
- Your child looks or acts very sick
Call Doctor Within 24 Hours
- Redness or red streak spreading from wart without fever
- Boil suspected (painful, non-itchy, red lump)
- You think your child needs to be seen
Call Doctor During Office Hours
- Wart on bottom of foot (plantar wart)
- Wart on face
- Wart on genitals or anus
- 4 or more warts
- Pus is draining from the wart (Apply antibiotic ointment 3 times per day until seen)
- On treatment more than 2 weeks and new warts appear
- On treatment more than 8 weeks and warts not gone
- You have other questions or concerns
Self Care at Home
- Common warts - 3 or less
Care Advice for Warts
-
What You Should Know About Warts:
- Warts are common (10% of children).
- Warts are harmless and most can be treated at home.
- The sooner you treat them, the less they will spread.
- Here is some care advice that should help.
-
Wart-Removing Acid:
- Buy a wart medicine with 17% salicylic acid (such as Compound W). No prescription is needed.
- Apply the acid once a day to the top of the wart. If there are many warts, treat the 3 largest ones.
- Since it's an acid, avoid getting any near the eyes or mouth. Also try to keep it off the normal skin.
- The acid will turn the wart into dead skin (it will turn white).
-
Duct Tape - Cover the Wart:
- The acid will work faster if it is covered with duct tape. Do not use regular tape.
- If you don't want to use an acid, use duct tape alone.
- Covering warts with duct tape can irritate the warts. This will turn on the body's immune system.
- Cover as many of the warts as possible. Cover at least 3 of them.
- The covered warts become red and start to die. Once this happens, often all the warts will go away.
- Try to keep the warts covered all the time.
- Remove the tape once per day, usually before bathing. Then replace it after bathing.
- Some children object to having the tape on at school. At the very least, tape it every night.
-
Remove Dead Wart:
- Once or twice a week, remove the dead wart material. Do this by paring it down with a disposable razor.
- This is easier to do than you think. It shouldn't cause any pain or bleeding.
- Soak the area first in warm water for 10 minutes. Reason: The dead wart will be easier to remove.
- Some children won't want you to cut off the layer of dead wart. Rub it off with a washcloth instead.
-
Prevention of Spread to Other Areas of Your Child's Body:
- Discourage your child from picking at the wart. Picking it and scratching a new area with the same finger can spread warts. A new wart can form in 1 to 2 months.
- Chewing or sucking on them can lead to similar warts on the face.
- If your child is doing this, cover the wart. Use a bandage (such as Band-Aid).
- Keep your child's fingernails cut short and wash your child's hands more often.
-
What to Expect:
- Without treatment, warts go away in about 2 years.
- With home treatment, they can usually be cleared up in 2 to 3 months.
- There are no shortcuts to treating warts.
-
Return to School:
- Your child doesn't have to miss any child care or school for warts.
- There is only a mild risk that warts spread to others.
-
Call Your Doctor If:
- Warts develop on the feet, genitals, or face
- New warts develop after 2 weeks of treatment
- Warts are still present after 12 weeks of treatment
- You think your child needs to be seen
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.
Wheezing (Other Than Asthma)
Is this your child's symptom?
- Breathing sound that is high-pitched and tight
- A purring or whistling sound
- You can hear it best when your child is breathing out
- Use this guide only if your child has not been diagnosed with asthma
If NOT, try one of these:
Causes of Wheezing
- Bronchiolitis. This is the main cause in the first 2 years of life. Bronchiolitis peaks at 6-12 months. This is a viral infection (usually RSV) of the small airways. These small airways are called bronchioles.
- Asthma. This is the main cause after age 2. The first attack of asthma can be hard to diagnose. Asthma is defined as attacks of wheezing that recur.
- Airway Foreign Object (Serious). Suspect this when there is a sudden onset of coughing, choking and wheezing. A clue is wheezing heard only on one side. Common examples of inhaled objects are peanuts and seeds. Peak age is 1 to 4 years.
- Nasal Sounds. When the nose is congested, it can produce some whistling sounds. This can happen during a cold or with nasal allergies. Unlike wheezing, the breathing is not tight. Also, nasal rinses with saline will make the sound go away.
When to Call for Wheezing (Other Than Asthma)
Call 911 Now
Call Doctor or Seek Care Now
|
Call 911 Now
- Wheezing and life-threatening allergic reaction to similar substance in the past
- Start to wheeze suddenly after a bee sting, taking medicine, or eating an allergic food
- Severe trouble breathing (struggling for each breath, very tight wheezing, can barely cry)
- Passed out or stopped breathing
- Bluish lips or face
- Choked on a small object or food recently
- You think your child has a life-threatening emergency
Call Doctor or Seek Care Now
- Wheezing, but none of the symptoms above. Reason: needs a doctor's exam.
Care Advice for Mild Wheezing
-
What You Should Know About Wheezing:
- Wheezing is a high-pitched purring or whistling sound.
- Wheezing means the lower airway is tight.
- This is often part of a cold, but it can become worse.
- Here is some care advice that should help until you talk with your doctor.
-
Coughing Fits or Spells:
- Breathe warm mist (such as with shower running in a closed bathroom).
- Give warm clear fluids to drink. Examples are apple juice and lemonade.
- Age under 3 months. Don't use.
- Age 3 - 12 months of age. Give 1 ounce (30 mL) each time. Limit to 4 times per day.
- Age over 1 year of age. Give as much as needed.
- Reason: Both relax the airway and loosen up any phlegm.
-
Homemade Cough Medicine:
- Do not give any over-the-counter cough medicine to children with wheezing. Instead, treat the cough using the these tips:
- Age 3 months to 1 year: Give warm clear fluids to treat the cough. Examples are apple juice and lemonade. Amount: Use a dose of 1-3 teaspoons (5-15 mL). Give 4 times per day when coughing. Caution: Do not use honey until 1 year old.
- Age 1 year and older: Use Honey ½ to 1 teaspoon (2-5 mL) as needed. It works as a homemade cough medicine. It can thin the secretions and loosen the cough. If you don't have any honey, you can use corn syrup.
-
Nasal Saline To Open a Blocked Nose:
- Use saline (salt water) nose drops or spray to loosen up the dried mucus. If you don't have saline, you can use a few drops of water. Use distilled water, bottled water or boiled tap water.
- Step 1. Put 3 drops in each nostril. If under 1 year old, use 1 drop.
- Step 2. Blow (or suction) each nostril out while closing off the other nostril. Then, do the other side.
- Step 3. Repeat nose drops and blowing (or suctioning) until the discharge is clear.
- How Often. Do nasal saline when your child can't breathe through the nose.
- Limit. If under 1 year old, no more than 4 times per day or before every feeding.
- Saline nose drops or spray can be bought in any drugstore. No prescription is needed.
- Saline nose drops can also be made at home. Use ½ teaspoon (2 mL) of table salt. Stir the salt into 1 cup (8 ounces or 240 mL) of warm water. Use bottled water or boiled water to make saline nose drops.
- Reason for nose drops: Suction or blowing alone can't remove dried or sticky mucus. Also, babies can't nurse or drink from a bottle unless the nose is open.
- Other option: use a warm shower to loosen mucus. Breathe in the moist air, then blow each nostril.
- For young children, can also use a wet cotton swab to remove sticky mucus.
-
Humidifier:
- If the air in your home is dry, use a humidifier. Reason: Dry air makes coughs worse.
-
Smaller Feedings:
- Use small, frequent feedings whenever your child has the energy to drink.
- Reason: Children with wheezing don't have enough energy for long feedings.
-
Avoid Tobacco Smoke:
- Tobacco smoke makes coughs and wheezing much worse.
-
Return to School:
- Your child can return to child care after the wheezing and fever are gone.
-
Call Your Doctor If:
- Trouble breathing gets worse
- Wheezing gets worse
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.
Wound Infection
Is this your child's symptom?
- Signs of wound infection include pus, spreading redness, increased pain or swelling, and fever
- A break in the skin (a wound) shows signs of infection
- Includes infected cuts, scrapes, sutured wounds, puncture wounds and animal bites
- Most dirty wounds become infected 24 to 72 hours later
If NOT, try one of these:
Symptoms of Wound Infections
- Pus. Pus or cloudy fluid is draining from the wound.
- Pimple. A pimple or yellow crust has formed on the wound.
- Soft Scab. The scab has increased in size.
- Red Area. Increasing redness occurs around the wound.
- Red Streak. A red streak is spreading from the wound toward the heart.
- More Pain. The wound has become very tender.
- More Swelling. Pain or swelling is increasing 48 hours after the wound occurred.
- Swollen Node. The lymph node draining that area of skin may become large and tender.
- Fever. A fever occurs.
- The wound hasn't healed within 10 days after the injury.
When to Call for Wound Infection
Call 911 Now
Call Doctor or Seek Care Now
|
Call Doctor Within 24 Hours
Call Doctor During Office Hours
|
Self Care at Home
|
Call 911 Now
- Not moving or too weak to stand
- You think your child has a life-threatening emergency
Call Doctor or Seek Care Now
- Fever occurs
- Red streak runs from the wound
- Spreading redness around the wound
- Severe pain in the wound
- Any face wound with signs of infection
- No past tetanus shots
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Call Doctor Within 24 Hours
- Pus or cloudy drainage from the wound
- Wound gets more painful or tender after 2 days
- Last tetanus shot was more than 5 years ago
- You think your child needs to be seen, but the problem is not urgent
Call Doctor During Office Hours
- Pimple where a stitch (or staple) comes through the skin
- You have other questions or concerns
Self Care at Home
- Mild redness of wound
Care Advice for Mild Redness of Wound
-
What You Should Know About Normal Healing:
- Some pink or red skin on the edge of the wound is normal.
- It's more common if the wound is sutured.
- It's also normal for it to be swollen for a few days.
- Your child's wound is not infected unless the redness spreads or pain increases.
- Here is some care advice that should help.
-
Warm Soaks or Warm Wet Cloth:
- For any redness or other signs of early infection, use heat.
- Open Cuts or Scrapes. Soak it in warm water. You can also put a warm wet cloth on the wound. Do this for 10 minutes 3 times per day. Use a warm saltwater solution. You can make your own. Put 2 teaspoons (10 mL) of table salt in a quart (liter) of warm water.
- Closed or Sutured Cuts. Put a heating pad on the wound. You can also use a warm, moist washcloth. Do this for 10 minutes 3 times per day.
- Cautions for Sutured Wounds. Do not put anything wet on the wound for first 24 hours. After 24 hours, can take brief showers. Never soak the wound before all sutures are removed.
-
Antibiotic Ointment:
- Use an antibiotic ointment (such as Polysporin).
- No prescription is needed.
- Put it on the wound 3 times a day.
- If the area could become dirty, cover with a bandage (such as Band-Aid).
-
Pain Medicine:
- To help with the pain, give an acetaminophen product (such as Tylenol).
- Another choice is an ibuprofen product (such as Advil).
- Use as needed.
-
Fever Medicine:
- For fevers above 102° F (39° C), give an acetaminophen product (such as Tylenol).
- Another choice is an ibuprofen product (such as Advil).
- Note: Fevers less than 102° F (39° C) are important for fighting infections.
- For all fevers: Keep your child well hydrated. Give lots of cold fluids.
-
What to Expect:
- Pain and swelling normally peak on day 2.
- Any redness should go away by day 4.
- Complete healing should occur by day 10.
-
Return to School:
- For true wound infections, your child can return after the fever is gone. Your child should also be taking an antibiotic by mouth for 24 hours.
- For minor redness around the wound, your child does not need to stay home.
-
Call Your Doctor If:
- Wound becomes more painful
- Redness starts to spread
- Pus or fever occurs
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Copyright 2000-2019 Schmitt Pediatric Guidelines LLC.

There is a pimple where a stitch comes through the skin. The pimple suggests a low-grade infection.

If you look closely at this photo, you should be able to see a red streak (lymphangitis) spreading from the hand wound up into the arm.
The presence of lymphangitis means that there is an infection that needs urgent antibiotic treatment. Admission to the hospital is sometimes required.